Hemifacial spasm (HFS) is characterised by involuntary tonic or clonic contractions of muscles innervated by the facial nerve. The pathogenesis of this condition is usually attributed to vascular compression at the emergence of the nerve root from the brainstem. This could be due to the appearance of ectopic discharges and the ephaptic transmission of abnormal impulses. Another potential mechanism could be central hyperexcitability with neural impairment in the facial nerve motor nucleus. To date, 5 cases of HFS caused by migraine have been published.1–3
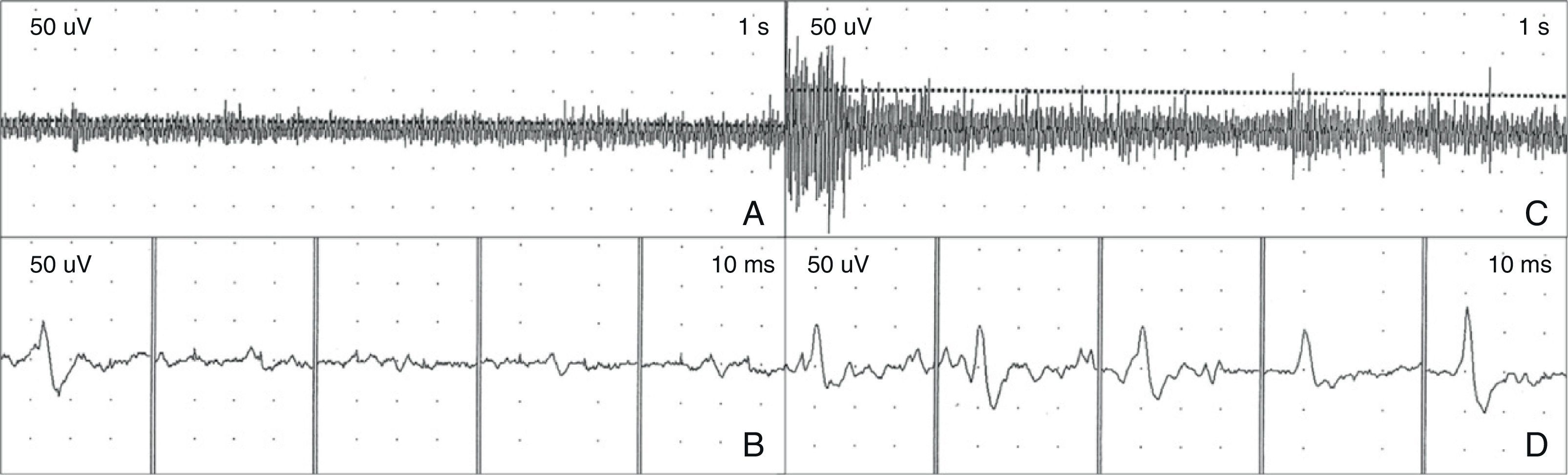
We present the case of a woman aged 30 with no relevant personal history who had experienced migraine attacks without aura since adolescence. In the previous year, headache episodes became more intense and were sometimes preceded by visual aura. Pain always presented on the right side of the head; upon reaching its maximum intensity, it was accompanied by involuntary contractions of the periocular ipsilateral muscles. Contractions decreased as pain subsided and only appeared during migraine attacks. These episodes occurred an average of 4 times per month. Initial neurological examination was normal. However, during one of the migraine episodes, we were able to observe the contractions of the right periocular muscles described above. Electromyography (EMG) showed tonic activity of the right orbicularis oculi with high-frequency bursts of increased muscle fibre recruitment (Fig. 1) coinciding with clonic spasms. The study of facial nerve motor conduction and blink reflex showed no relevant abnormalities. Brain MRI and MRA revealed a loop of the right anterior inferior cerebellar artery in contact with the facial nerve (Fig. 2). Treatment with topiramate was prescribed at increasing doses reaching 75mg per day, which decreased the frequency and intensity of migraine episodes and suppressed the associated muscle spasm.
Electromyogram showing spasm of the right orbicularis oculi during a migraine episode. (A, B) Baseline tonic muscle activity coinciding with tonic contraction and reduced palpebral fissure. (C, D) High-frequency bursts of muscle fibre recruitment coinciding with clonic spasms of the upper and lower eyelids.
High-resolution MRI at the level of the cerebellopontine angle. (A) 3D-FIESTA MR image (three-dimensional fast imaging employing steady-state acquisition) showing vascular contact (long arrow) with the right facial nerve (short arrow). (B, C) Three-dimensional time-of-flight MRA (3D-TOF MRA) showing a vascular loop of the right anterior inferior cerebellar artery (arrow) in the internal auditory canal.
The temporal relationship between migraine and HFS in the 6 published cases supports the idea of a pathophysiological link existing between those processes. As in prior cases,1–3 our patient presented episodes of HFS that coincided with maximum pain intensity. Therefore, rather than being a migraine aura phenomenon with positive signs, HFS seems to be a consequence of migraine. Husid raised the possibility that HFS could be due to a mechanism of central hyperexcitability related to migraine or to facial nerve compression caused by the dilation of nearby vessels, which in turn is produced by the trigeminovascular system in cases of migraine attacks.2 On the other hand Cuadrado et al. suggested that potentiation of certain trigeminofacial reflexes could cause HFS during a migraine episode.3 Barahona et al. combined all these hypotheses by proposing that central hyperexcitability phenomena, along with activation of trigeminofacial reflexes due to nociceptive stimuli arriving in the caudate nucleus of the trigeminal nerve, plus the possible compression of the facial nerve caused by the dilation of vessels that are in contact with the nerve, may provoke episodes of HFS during migraine attacks in predisposed patients.1
We believe that migraine-triggered HFS, like migraine-triggered seizure, could be included among the complications of migraine headaches.4 Both central and peripheral mechanisms may be involved in the pathogenesis of this condition.
Please cite this article as: Valencia C, Cuadrado ML, Barahona-Hernando R, Ordás CM, González-Hidalgo M, Jorquera M, et al. Espasmo hemifacial desencadenado por migraña: un caso más. Neurología. 2014;29:61–62.