Delirium is a condition with a high prevalence in hospitalised patients (10–30%), and it has important prognostic implications. There are few prospective studies of the incidence of delirium in Spain, and most of these were carried out in surgical wards or intensive care units. Our objective is to calculate the incidence of delirium in a neurological department and describe characteristics of affected patients.
MethodsLongitudinal descriptive study including all patients admitted to the neurology department in an 8-week period. The CAM score for diagnosing delirium was recorded on the first, second and fifth day of hospitalisation and we recorded demographic data, medical history, analytical data (including inflammatory markers), use of anticholinergic treatments, cognitive and functional state at admission, reason for admission, length of stay, and other events during hospitalisation.
ResultsWe studied 115 patients and found an incidence of delirium of 16.52%. There was a significant correlation between delirium and age, cognitive state at admission according to the Pfeiffer test, functional situation at admission according to the Canadian Neurological Scale, kidney failure, history of stroke, anticholinergic treatment, erythrocyte sedimentation rate, and C-reactive protein. These patients were also hospitalised for longer periods of time.
ConclusionsThese results confirm a high incidence of delirium in our geographical area. Although additional studies with larger samples are needed, we would like to emphasise the importance of several risk factors which may enable early detection of patients who are at risk for developing delirium during hospitalisation. This would permit preventive action and early treatment for these patients.
El delírium es una afección con una prevalencia elevada entre los pacientes ingresados (10–30%), con importantes implicaciones pronósticas. Existen pocos estudios prospectivos de incidencia en España y la mayoría se han realizado en plantas quirúrgicas o en unidades de cuidados intensivos. Nuestro objetivo es conocer su incidencia en una planta de neurología y describir las características de estos pacientes.
MétodosSe ha realizado un estudio longitudinal descriptivo, incluyendo a todos los pacientes ingresados en la planta de neurología durante 8 semanas, realizándose la escala CAM para el diagnóstico de delírium el primero, segundo y quinto días de ingreso y recogiéndose de cada paciente datos demográficos, antecedentes patológicos, analíticos (incluyendo marcadores inflamatorios), toma de fármacos anticolinérgicos, situación cognitiva y funcional al ingreso, causa de ingreso, tiempo de estancia y eventos durante la misma.
ResultadosSe estudió a 115 pacientes con una incidencia de delírium del 16,52%. Se observó una relación significativa con la edad, la situación cognitiva al ingreso valorada por el test de Pfeiffer, la situación funcional al ingreso medida por la escala Canadiense, la insuficiencia renal, los antecedentes de ACV, la toma de fármacos con actividad anticolinérgica, VSG y PCR. Se observó, además, una mayor estancia media en estos pacientes.
ConclusionesEstos resultados confirman una alta incidencia de esta afección en nuestro medio y, aunque son necesarios más estudios, con muestras mayores, destacamos la importancia de unos factores de riesgo que podrían contribuir a una detección precoz de pacientes en riesgo de desarrollar delírium durante el ingreso, permitiendo actividades preventivas y un tratamiento precoz de estos pacientes.
Delirium is defined as an acute onset, fluctuating alteration of consciousness that affects cognitive functions and attention.1
It is a common condition with a prevalence of about 11% to 30% in hospitalised patients. It may present at any time of life, although its incidence increases progressively with age (between 6% and 56% of hospitalised patients older than 65 are affected).2,3 It has important prognostic implications, a high mortality rate (6%–60%), and its presence is associated with longer mean hospital stays.3,4
Despite being a frequent and relevant condition, delirium often cannot be diagnosed early or correctly due to its variable symptoms and fluctuating course, which results in treatment delays and a poorer prognosis.5
Prospective studies on the incidence of delirium in Spain are scarce, and those that are available were conducted in surgical wards or intensive care units, where patients’ characteristics, drugs, and treatment measures differ from those commonly found in a medical ward.6–9
The pathophysiology of this disorder is not yet completely understood. Researchers suspect that there are multiple factors involved, which result from a series of triggers in vulnerable patients with decreased cognitive function.10
The aim of the current study is to ascertain delirium incidence in patients admitted to a neurology department, describe patients’ epidemiological characteristics, and calculate the prevalence of risk factors and markers (both predisposing and precipitating) that are related to this disease. This will help researchers create explanatory models contributing to our understanding of the pathophysiology of delirium, and thereby promote early diagnosis and appropriate treatment for these patients.
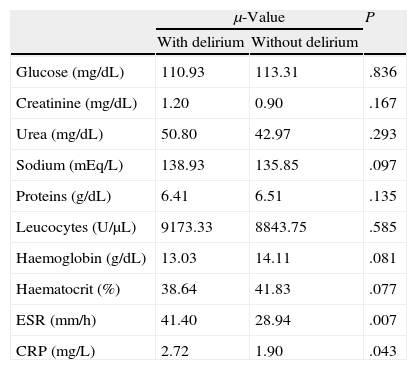
Patients and methodsWe carried out an observational descriptive study of all patients admitted to the neurology department at Hospital Universitario Miguel Servet in Zaragoza (HUMS) in the 8-week period between 5 July and 30 August 2010. Patients with a low level of consciousness (GCS<9) upon admission that would hamper an evaluation were excluded. From included patients we recorded demographic data, diagnosis upon admission, comorbidities and incidents during hospitalisation, perceptual alterations, cognitive state according to the Pfeiffer test, and functional state upon admission and discharge according to the Rankin and Canadian Neurological scales. We also collected the analytical data shown in Table 1, including systemic inflammatory markers and a record of drug treatments so as to classify patients according to whether or not they had taken drugs with anticholinergic effects.
Values of analytical parameters studied here in patients with or without delirium.
| μ-Value | P | ||
| With delirium | Without delirium | ||
| Glucose (mg/dL) | 110.93 | 113.31 | .836 |
| Creatinine (mg/dL) | 1.20 | 0.90 | .167 |
| Urea (mg/dL) | 50.80 | 42.97 | .293 |
| Sodium (mEq/L) | 138.93 | 135.85 | .097 |
| Proteins (g/dL) | 6.41 | 6.51 | .135 |
| Leucocytes (U/μL) | 9173.33 | 8843.75 | .585 |
| Haemoglobin (g/dL) | 13.03 | 14.11 | .081 |
| Haematocrit (%) | 38.64 | 41.83 | .077 |
| ESR (mm/h) | 41.40 | 28.94 | .007 |
| CRP (mg/L) | 2.72 | 1.90 | .043 |
CRP, C-reactive protein; ESR, erythrocyte sedimentation rate.
A single doctor used the CAM scale (confusion assessment method) to diagnose delirium on the first, second, and fifth days of hospitalisation.
Bivariate analysis employed the chi-squared test for dependent qualitative variables; the Yates correction was used when necessary. The relationship between dichotomous qualitative variables and quantitative variables was verified using the t-test or the non-parametric Mann–Whitney test, depending on whether they met criteria for normality and homogeneity of variance. The Kolmogorov–Smirnov test was used to check the normality of the data distribution. Values of P<.05 associated with the test statistic were considered statistically significant.
We used a multivariate logistic regression analysis for variables shown to be statistically significant by bivariate analysis.
ResultsOf the 120 patients studied, 4 were excluded due to death during the first 5 days and 1 due to having a Glasgow coma score of less than 9 upon admission. The final sample consisted of 115 patients (69 men and 46 women) of whom 19 presented delirium (13 men and 6 women), yielding an incidence rate of 16.52%. Within the delirium group, 11 presented hyperactive delirium (57.80%); 4, hypoactive delirium (21.05%); and 4, mixed delirium (21.05%).
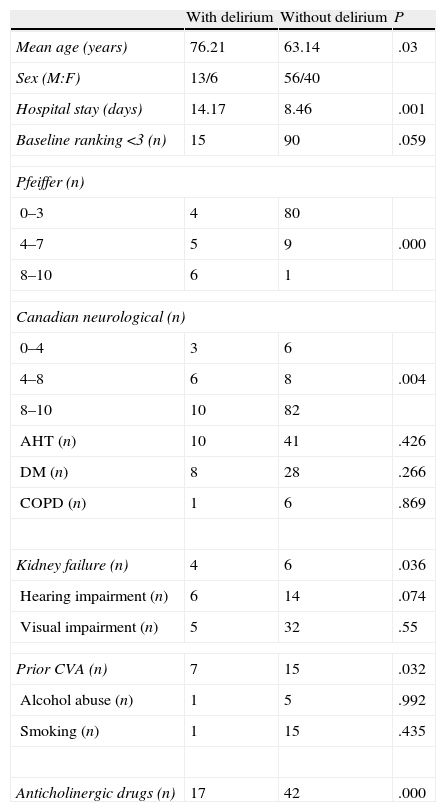
Patients’ characteristics are listed in Table 2.
Characteristics of patients with or without delirium.
| With delirium | Without delirium | P | |
| Mean age (years) | 76.21 | 63.14 | .03 |
| Sex (M:F) | 13/6 | 56/40 | |
| Hospital stay (days) | 14.17 | 8.46 | .001 |
| Baseline ranking <3 (n) | 15 | 90 | .059 |
| Pfeiffer (n) | |||
| 0–3 | 4 | 80 | |
| 4–7 | 5 | 9 | .000 |
| 8–10 | 6 | 1 | |
| Canadian neurological (n) | |||
| 0–4 | 3 | 6 | |
| 4–8 | 6 | 8 | .004 |
| 8–10 | 10 | 82 | |
| AHT (n) | 10 | 41 | .426 |
| DM (n) | 8 | 28 | .266 |
| COPD (n) | 1 | 6 | .869 |
| Kidney failure (n) | 4 | 6 | .036 |
| Hearing impairment (n) | 6 | 14 | .074 |
| Visual impairment (n) | 5 | 32 | .55 |
| Prior CVA (n) | 7 | 15 | .032 |
| Alcohol abuse (n) | 1 | 5 | .992 |
| Smoking (n) | 1 | 15 | .435 |
| Anticholinergic drugs (n) | 17 | 42 | .000 |
DM, diabetes mellitus; COPD, chronic obstructive pulmonary disorder; AHT, arterial hypertension.
The mean age of patients with delirium was 76 and that of healthy patients was 63 (P=.03).
Patients with delirium were significantly older, presented a poorer baseline functional state, and were more likely to have cognitive impairment. We also found a statistically significant correlation between delirium and history of acute cerebrovascular accident (CVA), kidney failure, and use of drugs with anticholinergic effects before and during hospitalisation (Table 2).
Of all the laboratory analyses studied, we only observed statistically significant associations between delirium and serum levels of C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) (Table 1).
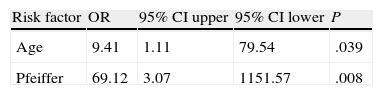
The multivariate logistic regression analysis revealed that a high number of errors on the Pfeiffer test and age greater than 65 constitute significant risk factors for delirium among hospitalised patients (Table 3).
A longer mean hospital stay was also recorded for patients with delirium (14.2 days) than for patients without delirium (8.5 days).
DiscussionThese results confirm the high incidence of delirium in patients admitted to a neurology department, as well as the longer mean hospital stay in this group compared to stays for patients without delirium (14.17 days vs 8.46 days).
Clinical features distinguish 3 types of delirium: hyperactive delirium (characterised by differing degrees of motor restlessness and agitation), hypoactive delirium (decreased psychomotor activity and lethargy), and mixed delirium (a combination of the above). According to most studies, mixed and hyperactive delirium are the most common types. However, researchers suspect that hypoactive delirium is underdiagnosed since diagnosing this type is more difficult.11 Our study describes a higher prevalence of hyperactive delirium, accounting for more than half of the patient total (57.8%).
The most commonly accepted risk factor for developing delirium is the presence of prior cognitive impairment. Some consider that delirium is simply an exacerbated phase or episode within the progression of dementia.12 Our study supports these results since we observed a statistically significant correlation between risk of delirium and baseline cognitive impairment (confirmed by the Pfeiffer test at time of admission).
Although the pathophysiology of delirium has not yet been fully explained, it has been linked to impairment of the cholinergic pathways, which play an important role in cognition and attention tasks. Several studies have observed a relationship between the use of drugs with anticholinergic effects and the development of delirium.13 Our study demonstrates this association by describing a higher prevalence of delirium in patients who were prescribed drugs with anticholinergic effects.
Researchers have studied different biomarkers for delirium that provide more complete information about its pathophysiology and promote early diagnosis and treatment.14 Inflammatory markers have been studied more thoroughly than other types of serological markers since researchers suspect a direct relationship between delirium and systemic inflammation.15 Although the pathophysiology of this association is poorly known, there is a suspected relationship between these mediators and the changes in the blood-brain barrier and cholinergic pathways.
Over the last few years, CRP has been the subject of several studies; most have shown a higher risk of developing delirium, with a poorer prognosis, in patients with high levels of CRP.16,17
Our study supports this association, as it describes a statistically significant correlation between both CRP and ESR levels and the incidence of delirium.
We suggest that factors that have been shown to be risk markers for delirium may allow researchers to develop preventive activities and early treatments that will improve prognosis for these patients.
We would like to highlight the finding that patients may be screened for risk of developing delirium at admission to hospital by recording their age and applying the Pfeiffer test, a simple tool that can be used by nursing staff. At-risk patients may then receive preventive care.
Studies with larger samples are needed in order to confirm our findings and provide explanatory models.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Ruiz Bajo B, et al. Incidencia y factores predictivos del delírium en pacientes neurológicos hospitalizados. Neurología. 2013;28:356–60.
This study was presented in poster format at the 2011 Annual Meeting of the Spanish Society of Neurology.