Although headache prevalence decreases in patients older than 65, headaches are a common complaint and their different clinical and therapeutic features must be understood. This article analyses the clinical characteristics of elderly patients treated in an outpatient headache unit.
MethodsWe collected demographic and clinical data from patients treated in a tertiary hospital headache unit between January 2008 and May 2013. Headaches were codified according to the International Classification of Headache Disorders, 2nd edition (ICHD-2).
ResultsOf a total of 1868 patients treated, 262 patients (14%, 189 women and 73 men) were older than 65 years. Ninety-nine (68 women, 31 men, 5.3% of the total) were over 75. Headaches began after the age of 65 in only 136 patients (51.9%). The 362 headaches were codified as follows: 23.8% as Group 1 (migraine) and 28.7% as Group 2 (tension-type headache). We diagnosed 58 (16%) secondary headaches; 26 (7.2%) were classified as Group 13 (cranial neuralgias) and 23 (6.4%) in Group 14 (other headaches). Symptomatic medication overuse was detected in 38 patients (14.5%). We also identified headaches considered typical in the elderly, including chronic migraine (41 cases), hypnic headache (6), occipital neuralgia (4), SUNCT (2), cervicogenic headache (1), primary cough headache (1), and giant cell arteritis (2).
ConclusionsElderly patients were frequently treated in our outpatient headache unit. Tension-type headache was the most common diagnosis in this population. Geriatric headache syndromes such as hypnic headache or occipital neuralgia were also represented in our series.
Aunque la prevalencia de las cefaleas disminuye en las personas mayores (≥ 65 años), son causa importante de consulta, con particularidades diagnósticas y terapéuticas que es necesario conocer. Analizamos las características de este grupo etario en una consulta de cefaleas.
MétodosRecogimos las variables demográficas y clínicas de los pacientes atendidos en una consulta de cefaleas de un hospital terciario (enero del 2008-mayo del 2012). Las cefaleas se codificaron según la Clasificación Internacional de Cefaleas, 2.a edición (CIC-2).
ResultadosDoscientos sesenta y dos pacientes (189 mujeres, 73 varones) con ≥ 65 años fueron atendidos sobre un total de 1.868 (14%); 99 (68 mujeres, 31 varones, 5,3% del total) superaban los 75 años. Inicio de la cefalea tras los 65 años en 136 casos (51,9%). Se codificaron 362 cefaleas, el 23,8% en el grupo 1 de CIC-2 (migrañas) y el 28,7% en el grupo 2 (cefalea tensional). Se diagnosticaron 59 (16%) cefaleas secundarias; 26 (7,2%) se encuadraron en el grupo 13 (neuralgias) y 23 (6,4%) en el grupo 14 (no clasificables). En 38 casos (14,5%) había sobreuso de medicación sintomática. Entre las cefaleas típicas de esta edad identificamos 41 migrañas crónicas, 6 cefaleas hípnicas, 4 neuralgias del occipital, 2 SUNCT, una cefalea cervicogénica, una cefalea primaria de la tos y 2 arteritis de la temporal.
ConclusionesEl porcentaje de personas mayores atendidas en una consulta de cefaleas es elevado. La cefalea tensional es la más frecuente en esta población. Cefaleas típicas de esta edad, como la cefalea hípnica o la neuralgia del occipital, están presentes.
The Spanish population is ageing. According to data from INE, Spain's National Statistics Institute, 17.33% of that country's citizens were aged 65 years or older in 2011. It is estimated that the percentage will reach 20.35% by 2021.1 The elderly, who require frequent medical attention, therefore constitute a large segment of our society. Multiple epidemiological studies show that headaches are more frequent among younger patients and that their prevalence decreases in older segments of the population.2–4 Despite this fact, the impact of headaches on the elderly is considerable.3,5
Most headaches diagnosed in elderly individuals are classified as primary headaches, and they are mainly migraines and tension headaches. In patients aged 65 and older, migraine frequency decreases and headache symptoms become more atypical and more commonly accompanied by aura.6–9 While secondary headaches remain more infrequent than primary headaches overall, they are more significant in this age group, accounting for 15% of the total headaches in the elderly, compared to 1% to 6% among patients younger than 65.10 It is therefore necessary to take additional precautions in light of the potentially severe underlying causes in this segment of the population.11
Some headaches are characteristic of and nearly exclusive to the elderly, including hypnic headaches and headaches secondary to giant cell arteritis. We must therefore be mindful of these entities when treating elderly patients.12
The purpose of this study is to describe the characteristics of a series of elderly patients cared for in a specialist headache unit at a tertiary hospital. In doing so, we attempt to provide epidemiological data to help promote a more thorough understanding of these patients, as well as better patient management.
Patients and methodsDuring a period spanning 4 years and 5 months (January 2008-May 2012), we prospectively registered all patients attended in the headache unit indicated above. We first recorded demographic data (age and sex). Headaches were coded according to ICHD-2 criteria.13 If the patient met criteria for multiple types of headache, all types were considered and coded.
Researchers also analysed clinical data, such as age at onset of each syndrome, impact of migraine as measured by the HIT-6 scale, and symptomatic and preventive treatments used before the patient had been referred to the headache unit. Doctors indicated the complementary studies that were considered necessary in each case according to the patient's individual characteristics.
We compared the distribution of headaches in this group with that among patients younger than 65 who were seen in this unit during the inclusion period. The mean was used as the measure of central tendency in the results, except in the case of age which shows the median. Lastly, we analysed headache distribution in the subgroup of patients aged 75 years or older.
ResultsTwo hundred sixty-two patients (189 women, 73 men) aged 65 years and older, comprising 14% of a total of 1868 patients, made an initial visit to the headache unit during the period specified above. The median age was 72 years (range, 65-94).
Primary care referred 149 cases (56.8%), while 70 were referred by general neurology clinics (26.7%); 35 patients (13.4%) were in-hospital consultations referred by other departments. Eight patients (3.1%) were seen without a scheduled appointment and most were family members of hospital employees.
The median age of onset of the headaches for which patients sought medical attention was 65.5 (range, 10-93). Onset of headaches occurred after the age of 65 years in 136 cases (51.9%).
The mean score on the HIT-6 scale in these patients was 54±8.2 (range, 40-72); values exceeded 55 in 44.4% of the cases.
Most patients (90.5%) had been taking some sort of symptomatic treatment for headache relief, while only 32.9% had been taking preventive treatment. Complementary studies had been ordered for 33.1% of the elderly patients in our series; most were neuroimaging studies or laboratory analyses, and tests measuring erythrocyte sedimentation rate (ESR) were particularly common.
In this elderly population, 99 patients (68 women and 31 men, 37.8%) were aged 75 years or older. This segment represents 5.3% of our total sample.
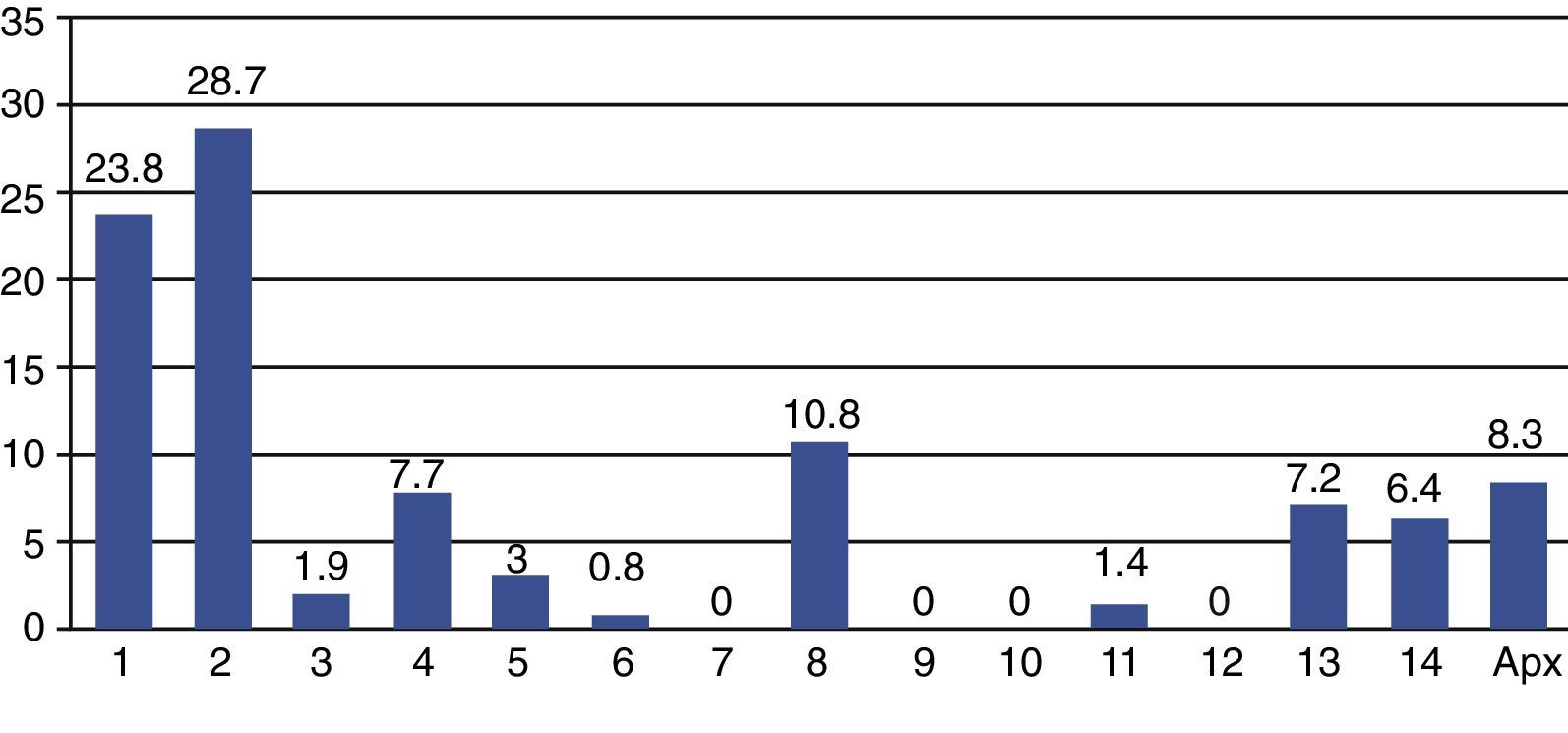
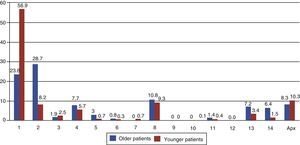
In the group of 262 patients aged 65 or older, researchers coded 362 headache episodes. Primary headaches, or groups 1 through 4 in the ICHD-2 classification, accounted for 225 (62.2%). The most frequent groups were 2 (tension-type headache) with 104 cases (28.7%) and 1 (migraine) with 86 cases (23.8%). There were 58 headache episodes (16%) coded as secondary headaches in groups 5 through 12; 26 in group 13 (cranial neuralgia, 7.2%), 23 in group 14 (other headaches, 6.4%) and 30 in the ICHD-2 appendix (8.3%). Regarding secondary headaches, the most frequent were attributed to substances (39 cases), followed by those associated with cranial trauma (11 headaches). Only the 3 headaches classified in group 6 (due to vascular disorders) can be considered secondary to severe causes. Percentages for each group are shown in Fig. 1.
Headaches considered typical at older ages were also present among the diagnoses assigned to our elderly population. We recorded 41 cases of chronic migraine, 6 of hypnic headache, 4 cases of occipital neuralgia, 2 cases of short-lasting unilateral neuralgiform headache with conjunctival injection and tearing (SUNCT), 1 case of cervicogenic headache, 1 primary cough headache, and 2 headaches related to temporal arteritis.
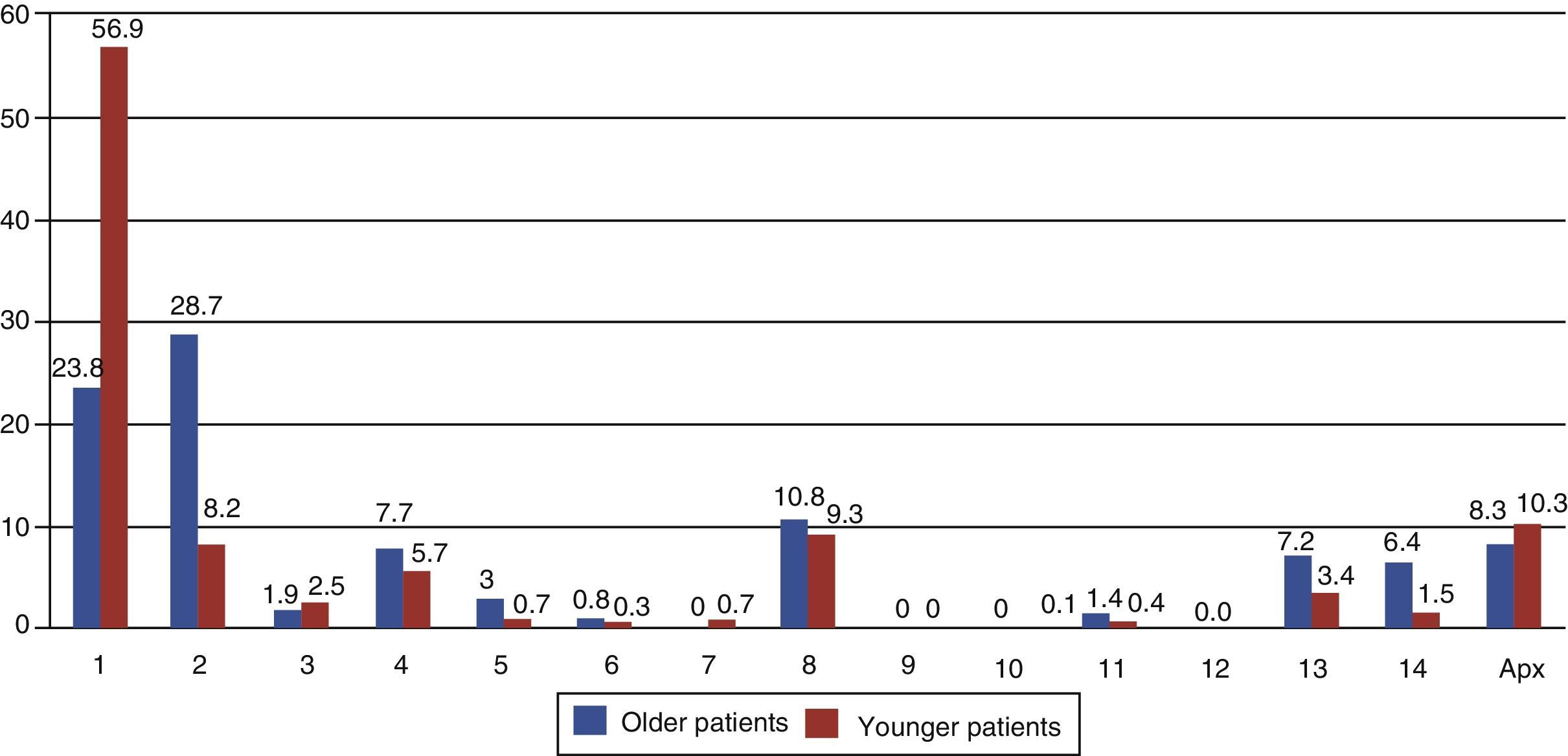
We compared the distribution of headaches in the elderly patients series with that in the 1606 patients younger than 65 (1159 women and 447 men) attended in the same unit during the inclusion period. Researchers coded 2522 headaches. Of this total, 1849 (73.3%) were recorded as primary headaches, 290 (11.5%) were classified as secondary headaches, 86 (3.4%) were assigned to group 13, 38 (1.5%) were classified in group 14, and 259 (10.3%) were coded in the appendix. In younger patients, we find higher percentages of tension-type headaches, secondary headaches, neuralgias, and other headaches (unspecified or unclassifiable). We also find a higher percentage of trigeminal-autonomic headaches. Fig. 2 shows the comparison between older and younger patients.
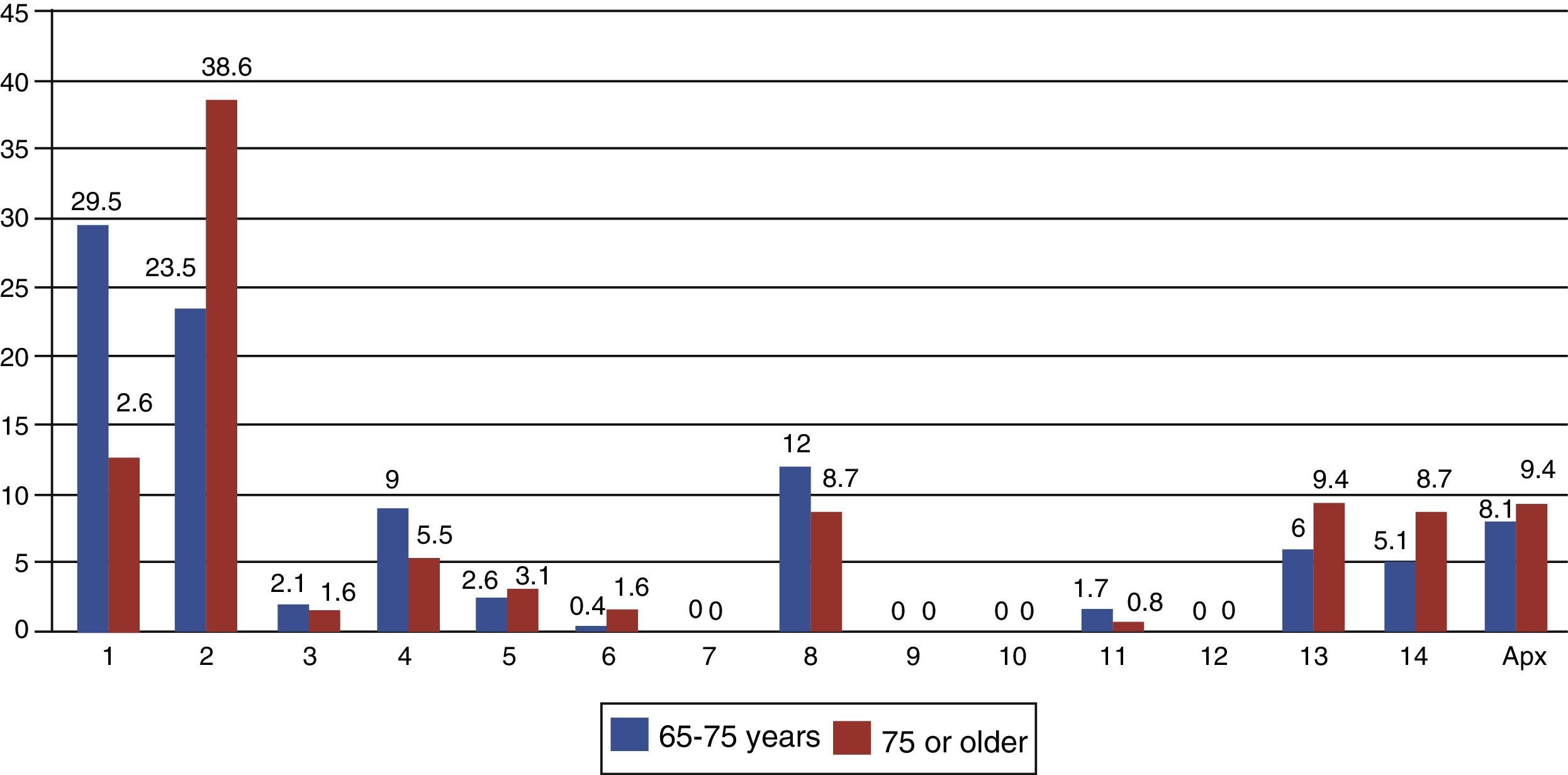
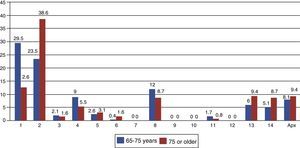
Lastly, we compare the headache distribution between the younger segment of the elderly population (65-75 years) and the very elderly population (75 years or more). In the latter group, researchers coded 127 headache events; most were primary headaches (74, 58.3%). A striking feature in the analysis of the two populations is that tension-type headaches are even more predominant in the very elderly population. A complete comparison by ICHD-2 diagnostic group is provided in Fig. 3.
DiscussionIt is a known fact that headache prevalence decreases in older age groups. The review of European epidemiological studies on headaches by Stovner et al.2 offers a diagram of this decreasing tendency in each age group after adulthood. For example, these authors calculate a yearly headache prevalence of 35% for patients aged 60 to 70, but 25% among patients aged 70 to 80.
However, despite this decrease, headaches remain an important problem among the elderly; half of this population may experience different types of headaches3,14–16 and one in 5 elderly patients has recurrent headaches.17
In our study, patients aged 65 or older made up 14% of the population treated in a specialist headache unit. A similar study in Italy shows that elderly patients made up 6.4% of the population,12 but as that study does not describe where its patients came from, we cannot attempt to explain the difference in percentages. However, the percentage of patients aged 75 and older treated in our unit is comparable to that recorded in a general neurology clinic in our setting.18
Most authors point out the higher percentage of secondary headaches among elderly individuals.3,11,19,20 Researchers have proposed several causes of secondary headaches in this age group. Our results coincide with those from other studies in that the higher rate of secondary headaches in older than in younger patients is mainly explained by ICHD-2 classification groups 5 (headache attributed to head and/or neck trauma) and 8 (headache attributed to a substance).21–23
Headaches secondary to serious conditions were uncommon in our series and complementary testing was only necessary for about a third of our patient total (33.1%). It seems clear, at least in our sample, that the patient's medical history and physical examination provide the fundamental basis for diagnosing headaches in this age group as well as in others.
Giant cell arteritis is considered an infrequent disease; its incidence rate is between 1 and 30/100000 patients aged 50 or older (between 3 and 16/100000 in Spain).24 Headache is the first symptom of this disease in almost half the affected patients, and it will appear at some point during the course of the disease in 90%.25–28 Our series only identified 2 cases of headache related to temporal arteritis (0.76% of the total population aged 65 or older). One of our criteria for referring patients to our unit from primary care is an ESR measurement in patients aged 50 and older. This requirement is also stated in official guidelines published by the Spanish Society of Neurology.29 For this reason, these patients are probably diagnosed in primary care centres or internal medicine consultations due to headache or other accompanying symptoms. Only a small minority of these patients will be treated by a specialist headache unit; the fact that only 0.62% of the headache cases in patients aged 75 or older and visiting in a general neurology consultation were related to temporal arteritis18 supports this hypothesis.
The most frequent diagnosis in our series was tension-type headache (28.7% of the total). Studies carried out to determine the prevalence of tension-type headache in the general population have obtained highly variable results, ranging from a yearly prevalence rate of 86.5% to a lifetime rate of 11.5%.21 Regarding more specific studies in the age group in question, annual prevalence rates of 16% to 44% have been established in individuals aged 50 and over.3,17,30–32 Presence of tension-type headache is even higher among patients older than 75 years,12,18 as we also observed in our series. According to these results, and considering the vast difference between the percentage of tension-type headaches in younger and in older patients, we can state that this entity is typical in the elderly.
At 23.8%, the second most common diagnosis in our population of elderly patients was migraine. Multiple epidemiological studies have shown that, after a peak in frequency (whether unimodal or bimodal) between the ages of 20 and 50,6,11,33 migraine prevalence decreases progressively in older age ranges. For patient populations aged 65 and older, the annual migraine prevalence rate is approximately 10%.3,17 This percentage is higher, with values resembling those in our study, in a specialist headache unit.12 In patients older than 75, as we also observed in our population, percentages continue to decrease.18
Forty-one patients in our series (15.6%) met diagnostic criteria for chronic migraine34; transformation of episodic migraine to chronic migraine is well-documented in elderly patients.19,21,35,36 It is important to note that migraines change with age, and this may make diagnosis more difficult in elderly patients. Characteristics such as pulsatility, associated photophobia or phonophobia, exacerbation with exercise, and high intensity will diminish over time.6 On the other hand, autonomic symptoms and bilateral pain are more common in elderly patients.7 The importance and significance of migraine with aura in elderly patients remains a controversial topic. Firstly, it is uncommon to find de novo migraines in patients older than 65, but in cases of onset in middle age, migraine with aura may occur over longer time periods. This occurs because the patient maintains, at an older age, the mechanism responsible for cortical spreading depression, while losing the propensity for neurovascular inflammation and the pain it produces.6,9 We identified only 3 patients with migraine with aura in our series, and only one case experienced onset after the age of 55. Differential diagnosis for transient ischaemic attack and migraine with aura is not always easy in patients in this age group. Visual and sensory changes with symptom progression are more suggestive of aura, whereas neurovascular events tend to show a sudden onset.37,38
Hypnic headaches are another type of primary headache present in our sample in 6 cases (1.7%). Although they are uncommon outside of this age range,39 both our group and other authors have seen cases of onset before the age of 65.40
SUNCT is an uncommon entity; its prevalence is 6.6/100000 and its annual incidence rate is 1.2/100000.41 The syndrome is characterised by multiple daily attacks of intense unilateral pain of short duration (less than 2minutes). The headaches affect the periorbital region and they are associated with homolateral cranial autonomic symptoms. Typical age of onset is about 50 years.37 This entity appeared in 2 patients in our series.
Cervicogenic headache is considered a typical disease in the elderly, but it only appears in one patient in our series. Many of these patients will seek medical care in rheumatology or traumatology departments; on the other hand, ICHD-2 criteria for this entity are extremely strict. It will be necessary to review the prevalence of this type of headache using the criteria in the new third edition of the classification; these criteria place less importance on the requirement of pain resolution after treatment and more importance on the manoeuvres that trigger the pain.
We noticed that our population of patients aged 65 and older showed a high percentage of neuralgias (group 13 in ICHD-2); this was even higher in those older than 75. The most common type of neuralgia in our series is essential trigeminal neuralgia (8 patients).
The percentage of headaches in group 14 (not classified or unspecified) is also higher in our population; at least in this population, the older the patient, the more difficult it is to identify or classify the headaches he or she experiences. This may be due to the added difficulty of taking down a patient history from some patients with cognitive impairment; better care for headache sufferers in this age range might help us describe other syndromes that are typical in the elderly.
In conclusion, headache is a common motive for a neurological consultation among the elderly. Although one of our study's limitations may be a selection bias, these results from a series of patients aged 65 and older who visited a specialist unit due to headaches show that primary headaches are the most frequent type in this age group, with tension-type headache being the most common entity. According to our results, a group of entities that include headache related to medication problems, chronic migraine, and neuralgia may be considered typical in these patients. Correctly identifying these entities on a case-by-case basis will help us offer our elderly patients the most appropriate treatment.
Conflict of interestThe authors have no conflicts of interest to declare.
Many thanks again to Lourdes; without your dedicated efforts in the headache unit, none of this would have been possible.
Please cite this article as: Ruiz M, Pedraza MI, de la Cruz C, Barón J, Muñoz I, Rodríguez C, et al. Cefaleas en la persona mayor: características de una serie de 262 pacientes. Neurología. 2014;29:321–326.
Part of this study was presented as an oral communication at the 64th Annual Meeting of the Spanish Society of Neurology, Barcelona, November 2012.