Multiple sclerosis is a demyelinating disease that causes severe disability in younger patients. Many epidemiology studies have confirmed a variable prevalence. The objective of this study was to analyse the prevalence of this disease in La Rioja (Spain), using such variables as age and sex; type of progression, initial form of the disease, EDSS and number of relapses; disease-modifying treatment and reasons for treatment withdrawal; personal and family history of cancer; and incidence and mortality.
MethodsAnalysis of patients in La Rioja diagnosed with MS (according to Poser criteria or the 2005 McDonald criteria) during a 10-year period (2001-2011). Data were collected from hospital records, multiple sclerosis associations, and personal records kept by neurologists.
ResultsThe MS prevalence rate in La Rioja is 65 patients/100000 inhabitants with an incidence rate of 3.5 cases/100000 residents per year. Relapsing-remitting MS is present in 67.6% of the patient total. Mean age of onset is 20-29 years (range 12-70). Most EDSS scores were mostly ≤2. Untreated MS cases account for 47.6% of the total, and the most commonly used therapy is interferon. We detected four haematological tumours and seven families with multiple members affected by MS.
ConclusionsPrevalence and incidence are similar to those found in other regions of Spain. The average age at onset age for primary progressive MS is slightly higher than in other papers (40-49 years). In families with multiple patients, MS may be more aggressive. Disability in these patients remains very severe. We require more epidemiology studies with a variety of data gathering methods to support findings for prevalence obtained in different provinces.
La esclerosis múltiple (EM) es una enfermedad desmielinizante que causa gran discapacidad en jóvenes. Se han realizado múltiples estudios epidemiológicos en los que se ha constatado una prevalencia variable. El objetivo de este estudio era analizar la prevalencia de esta enfermedad en La Rioja (España) con variables como la edad, el sexo, la forma evolutiva, la clínica de inicio de la enfermedad, la EDSS y el número de brotes, el tratamiento modificador de la enfermedad y los motivos de su retirada, el cáncer y los antecedentes familiares, y la incidencia y la mortalidad.
MétodosAnalizar los pacientes diagnosticados de EM según los criterios de McDonald 2005 o Poser, residentes en La Rioja, durante 10 años (2001-2011), recogidos a través del registro hospitalario, la Asociación de Esclerosis Múltiple y los registros personales de los neurólogos.
ResultadosEn La Rioja, existe una prevalencia de EM de 65 pacientes/100.000 habitantes y una incidencia de 3,5 casos/100.000 habitantes-año. El 67,6% de los pacientes presentan una EM remitente-recurrente. La edad media de inicio es 20-29 años (desde los 12 hasta los 70). La puntuación EDDS es mayoritariamente ≤ 2. Las EM sin tratamiento suponen el 47,6% y el tratamiento más usado son los interferones. Hallamos 4 tumores hematológicos y 7 familias con varios afectados por EM.
ConclusionesLa prevalencia y la incidencia son similares a las halladas en el resto de España. La edad media de inicio de la forma primaria progresiva es ligeramente mayor que en otras publicaciones (40-49 años). En familias con varios miembros afectados, la EM podría tener un curso más agresivo. La discapacidad de estos pacientes sigue siendo muy elevada. Son necesarios más estudios epidemiológicos con métodos variables de recogida de datos para afianzar los hallazgos obtenidos en diferentes provincias acerca de la prevalencia.
Multiple sclerosis (MS) is an inflammatory demyelinating disease of the central nervous system characterised by focal destruction of myelin sheaths, glial scar formation by astrocytes, and varying degrees of axonal damage. The aetiology of MS remains unknown. The most widely accepted theory is that MS manifests in genetically predisposed individuals1 under the influence of one or more unknown environmental factors, such as viral infection (Epstein–Barr virus,2 cytomegalovirus,3 varicella zoster virus,4 etc.), vitamin D deficit during pregnancy (more prevalent in Northern countries; exposure to sunlight is thought to have a protective effect)5, white race, and excess hygiene in industrialised countries.6
MS is the most frequent cause of non-traumatic neurological disability in young adults. Disease onset rarely occurs in patients younger than 15 or older than 50 years old. Mean age of onset ranges from 29 to 32 years in patients with relapsing-recurrent (RR) MS, while onset of progressive forms occurs at older ages (35-39 years). It is well-established that incidence rates are higher among women. Mortality due to MS is estimated at 0.7/100000 population, and it is associated with a 10-year reduction in life expectancy.7
Epidemiological studies vary greatly from region to region, and differences can be observed even between studies conducted in the same area. This heterogeneity can result from using different diagnostic criteria or from issues with data collection.
The more than 30 prevalence studies that have been conducted in Spain have yielded rates of 47.7–79/100000 population-years.8–18 However, a recent study by Fernández et al.,19 carried out in Málaga using the capture-recapture method, obtained a significantly higher prevalence rate of 125 patients/100000 population. Regarding incidence, figures between 2.2 and 5.3 cases/100000 population have been calculated in the last 10 years. The mean value for mortality was 0.35 cases/100000 population-years.
Since no studies of MS prevalence have been carried out in La Rioja, we present the first epidemiological study of that entity in our region. In our study we have considered the following aspects: mortality rate, the influence of latitude according to Kurzke,20 the possible influence of other factors on prevalence (as in the case of the infectious vector in the Orkney Islands21,22), and recent statistical shifts. These changes refer to the recent increase in incidence that can be attributed to better diagnostic methods (MRI) and possibly to environmental factors, and the increase in prevalence23 arising from the longer life expectancy of these patients.24
ObjectivesMain objectiveSecondary objectives- –
Determine the incidence and mortality rates of patients with MS in La Rioja during the 10-year period between 1 October 2001 and 30 September 2011.
- –
Examine the characteristics associated with the disease in our patients: progression, age and clinical picture at symptom onset, mean level of disability determined by the EDSS, mean annual relapse rate in RRMS, complementary diagnostic tests carried out, specific treatment (immunomodulatory drugs and immunosuppressants), reasons for changing treatment, and family history of MS.
- –
La Rioja. This region of northern Spain covers a total area of 5045km2, and its geographical coordinates are 42°39′N at its northernmost point and 41°55′N at its southernmost point; longitude 1°41′W at its eastern point and 3°08′W at its western point.27 Its northern area contains part of the Ebro river valley, and its southern mountains are part of the Iberian System. This location enjoys a Mediterranean climate with continental climate influence. Mean yearly temperature in the Ebro river valley is 13.5°C, decreasing to 6.6°C in mountainous areas.28
- –
This is a retrospective study, which includes data collected between 1 October 2001 and 30 September 2011 (10 years) for subsequent analysis.
- –
Population: subjects living in the region of La Rioja during the study period.
- –
Patients diagnosed with MS defined according to the 2005 McDonald criteria when possible, or alternatively according to the Poser criteria.
- –
Study period: 1 October 2001 to 30 September 2011.
- –
Patients with MS diagnosed after 30 September 2011, or deceased before 1 October 2001.
- –
Patients who met the 2010 McDonald criteria but not the 2005 McDonald criteria or the Poser criteria.
- –
Patients who have visited the neurology department only sporadically without routine follow-up, or those not residing in La Rioja region.
We used population data published by Spain's National Statistics Institute as of 1 October 2011 as a reference to determine the prevalence of MS in the region of La Rioja.29
Different sources were used to recruit sample patients, such as the records kept by Hospital de San Pedro de Logroño (since patients from Hospital Fundación de Calahorra who need treatment are referred to Logroño), our hospital's pharmacy department, the database kept by the Multiple Sclerosis Association of La Rioja (ARDEM), and records from neurology clinics in the region.
Regarding diagnostic techniques, our department provides neuroimaging (CT, 1.5T MRI), evoked potential testing, and optical coherence tomography. CSF oligoclonal band screening was performed at the laboratory of Hospital de Donostia.
The following diagnoses were reviewed: MS, clinically isolated syndrome, optic neuritis, spastic paraparesis, and internuclear ophthalmoplegia.
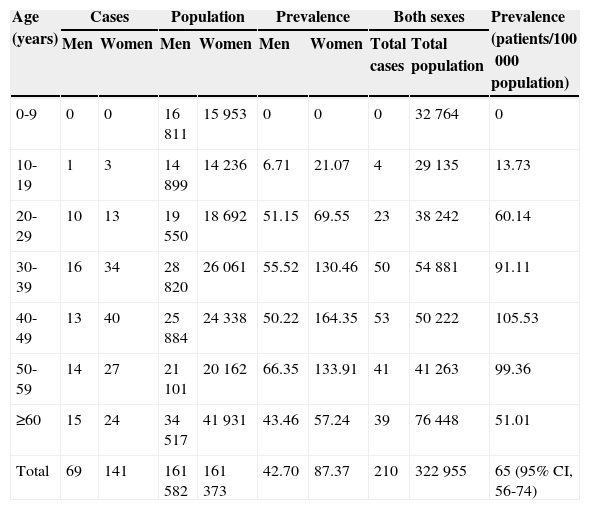
Data was processed using EPIDAT software.
ResultsPrevalenceThe population of La Rioja, according to data from Spain's National Statistics Institute for the year 2011, was 322955 inhabitants (161582 men and 161373 women). Considering a total of 210 MS patients as of 30 September 2011, prevalence amounts to 65 patients/100000 population (95% CI, 56-74). Women accounted for 67% (141), and men, 33% of the total (69), for a ratio of approximately 2:1. Table 1 shows prevalence rates adjusted by age and sex.
Prevalence per 100000 population, adjusted by age group and sex.
| Age (years) | Cases | Population | Prevalence | Both sexes | Prevalence (patients/100000 population) | ||||
|---|---|---|---|---|---|---|---|---|---|
| Men | Women | Men | Women | Men | Women | Total cases | Total population | ||
| 0-9 | 0 | 0 | 16811 | 15953 | 0 | 0 | 0 | 32764 | 0 |
| 10-19 | 1 | 3 | 14899 | 14236 | 6.71 | 21.07 | 4 | 29135 | 13.73 |
| 20-29 | 10 | 13 | 19550 | 18692 | 51.15 | 69.55 | 23 | 38242 | 60.14 |
| 30-39 | 16 | 34 | 28820 | 26061 | 55.52 | 130.46 | 50 | 54881 | 91.11 |
| 40-49 | 13 | 40 | 25884 | 24338 | 50.22 | 164.35 | 53 | 50222 | 105.53 |
| 50-59 | 14 | 27 | 21101 | 20162 | 66.35 | 133.91 | 41 | 41263 | 99.36 |
| ≥60 | 15 | 24 | 34517 | 41931 | 43.46 | 57.24 | 39 | 76448 | 51.01 |
| Total | 69 | 141 | 161582 | 161373 | 42.70 | 87.37 | 210 | 322955 | 65 (95% CI, 56-74) |
Most of the patients were recruited using hospital records and neurologists’ records (duplicate entries in many cases); records from the pharmacy department listed approximately half of the cases (patients on disease-modifying treatment). ARDEM's database also listed about half of the total (most of whom were duplicates of the hospital records).
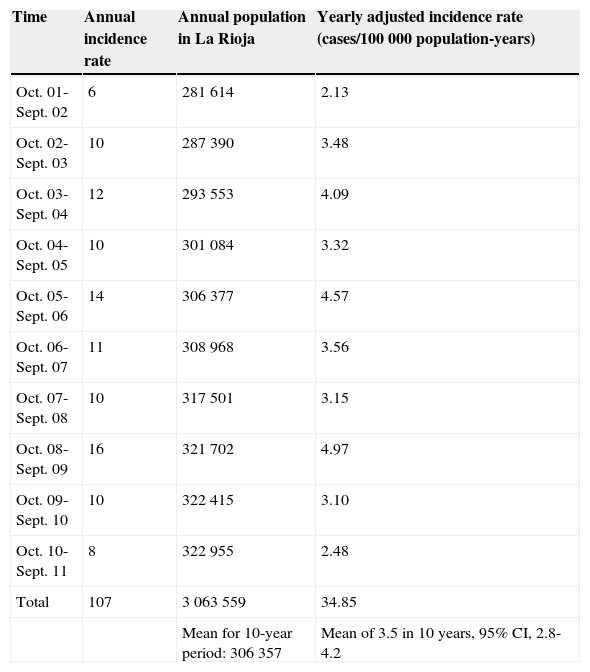
IncidenceIncidence of MS in our region reaches 3.5 cases/100000 population-years, with a 95% CI for range 2.8-4.2 (107 patients diagnosed in the 10 years preceding 30 September 2011). Since interyear variation was considerable, we have included a breakdown of these values in Table 2.
Specific incidence rate per year.
| Time | Annual incidence rate | Annual population in La Rioja | Yearly adjusted incidence rate (cases/100000 population-years) |
|---|---|---|---|
| Oct. 01-Sept. 02 | 6 | 281614 | 2.13 |
| Oct. 02-Sept. 03 | 10 | 287390 | 3.48 |
| Oct. 03-Sept. 04 | 12 | 293553 | 4.09 |
| Oct. 04-Sept. 05 | 10 | 301084 | 3.32 |
| Oct. 05-Sept. 06 | 14 | 306377 | 4.57 |
| Oct. 06-Sept. 07 | 11 | 308968 | 3.56 |
| Oct. 07-Sept. 08 | 10 | 317501 | 3.15 |
| Oct. 08-Sept. 09 | 16 | 321702 | 4.97 |
| Oct. 09-Sept. 10 | 10 | 322415 | 3.10 |
| Oct. 10-Sept. 11 | 8 | 322955 | 2.48 |
| Total | 107 | 3063559 | 34.85 |
| Mean for 10-year period: 306357 | Mean of 3.5 in 10 years, 95% CI, 2.8-4.2 |
During the 10-year study period, 11 patients with MS died. From this number, we should exclude one patient who died of multiple myeloma when her EDSS score was still low, as well as two patients who died of unknown causes (all other patients presented very high EDSS scores at the time of, and related to, their deaths). Therefore, the mortality rate calculated for the remaining eight patients would be 0.26/100000 population (95% CI, 0.1-0.5).
Clinical characteristics of cases included in the prevalence calculation and other variables analysed- –
Type of MS. Most patients with this disease experience relapses, which were consistent with RRMS in 67.6% (142 patients), secondary progressive MS in 19% (SP, 40 patients), primary progressive MS in 9% (PP, 19 cases), and 4.3% progressive relapsing MS (PR, nine cases). RRMS usually takes a mean of 14 years to progress to SPMS (range, 1-39 years).
- –
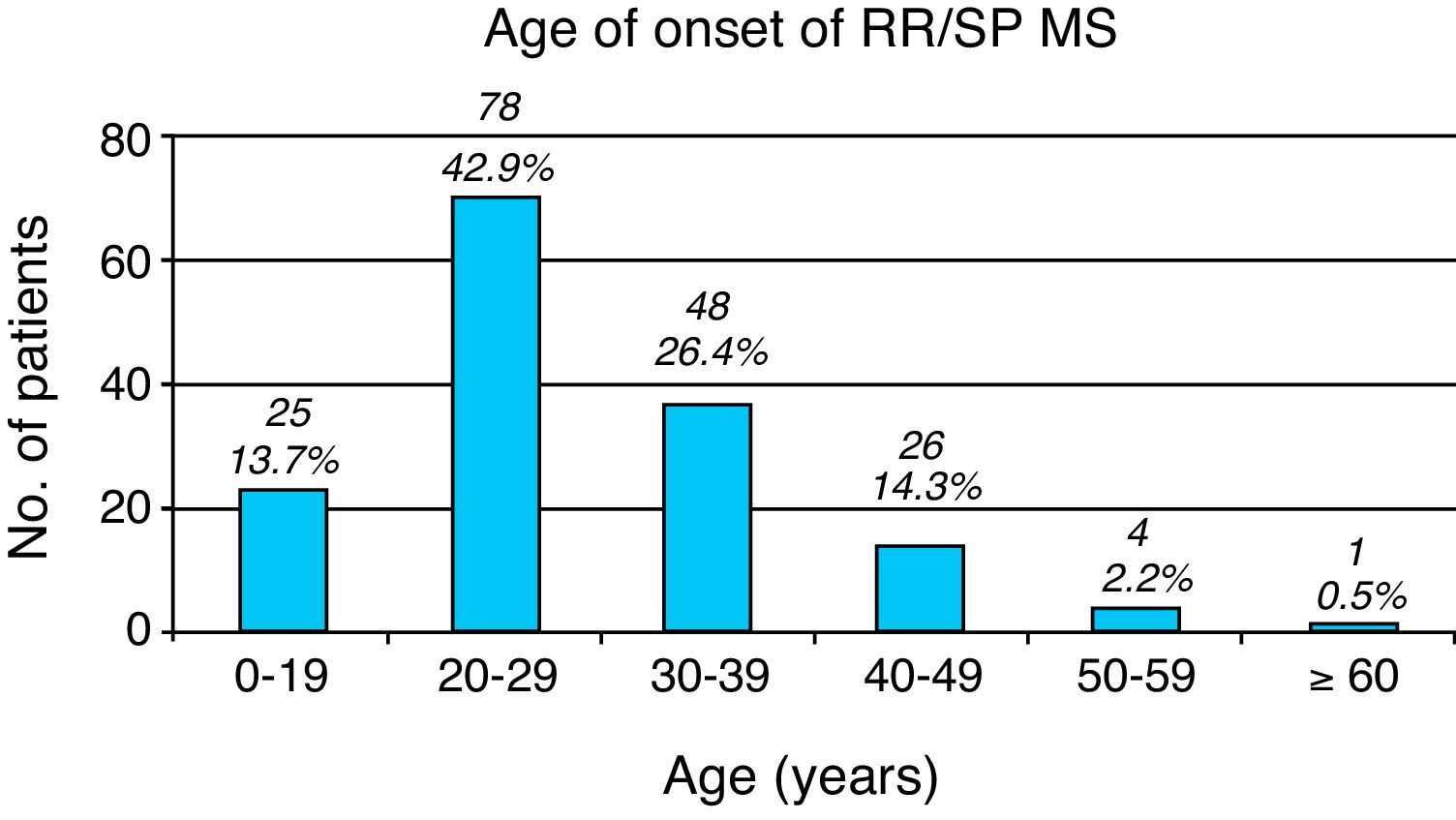
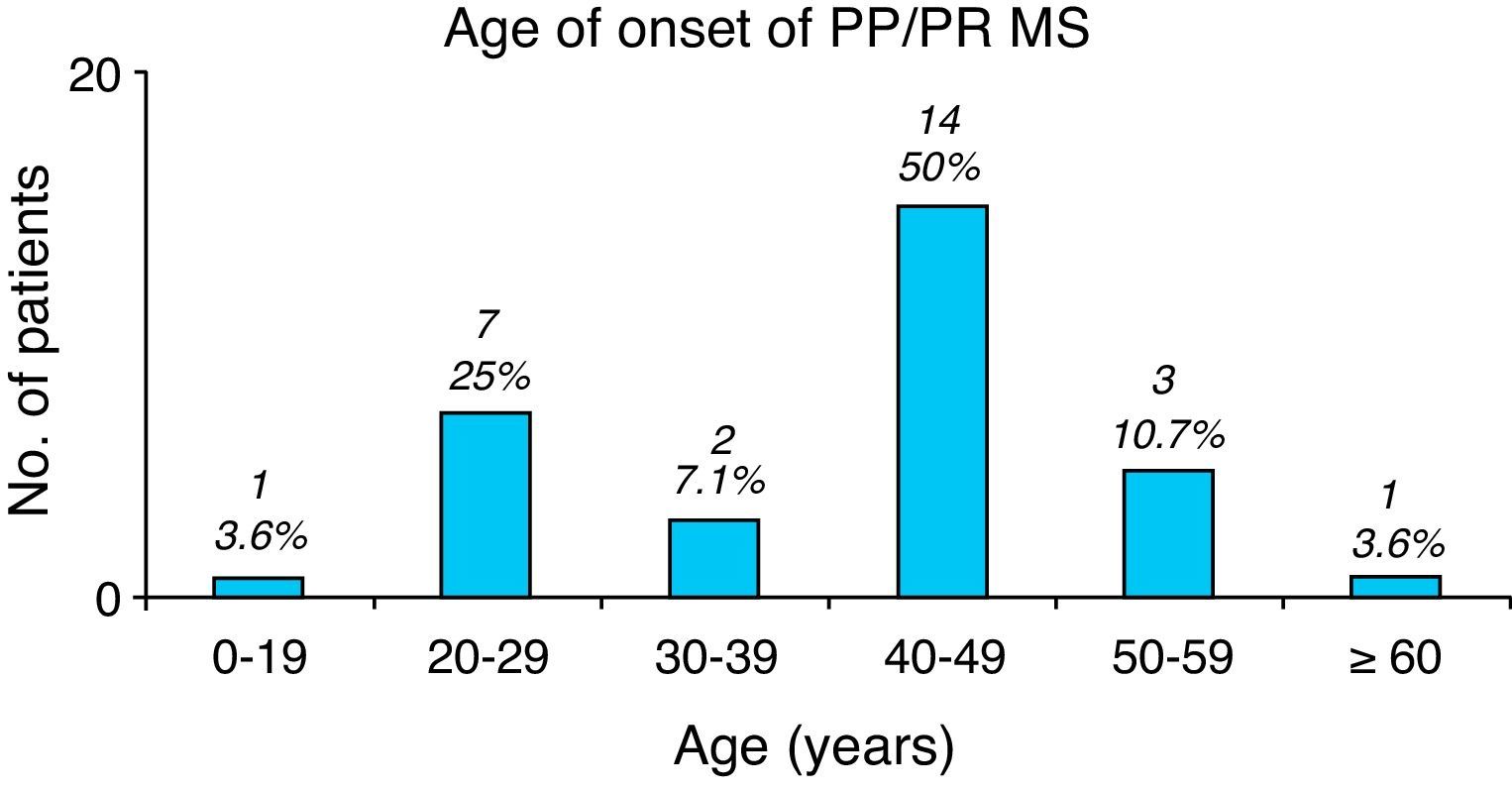
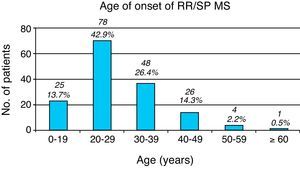
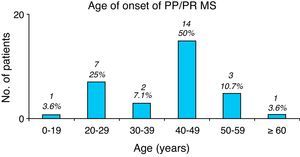
Age at symptom onset. Overall, most patients with any type of MS ranged in age between 20 and 29 years at symptom onset (85 patients [40.5%]). The youngest patient was a 12-year-old girl (not counting two patients who suffered peripheral facial paralysis in the first year of life); the eldest patient at symptom onset was 70 years old. Seven patients were younger than 16, accounting for 3.3% of the total. In RRMS (including patients currently affected by SPMS), onset normally takes place in ages ranging from 20 to 29 years (Fig. 1), while PP/PR forms have an older age of onset, between 40 and 49 years (Fig. 2).
- –
Clinical signs at onset. Diagnosis is not typically established at the time of the first symptoms, and in many cases the patient will not see a neurologist for several years, especially if symptoms are mild. Initial symptoms of RRMS or SPMS vary, and infratentorial signs are slightly dominant, with lower percentages of impairment at other localisations: optic tracts (35 patients, 19.2%), supratentorial region (39 patients, 21.4%), brainstem (51 patients, 28%), spinal cord (53 patients, 29.1%), and unknown (4 patients, 2.2%).
- –
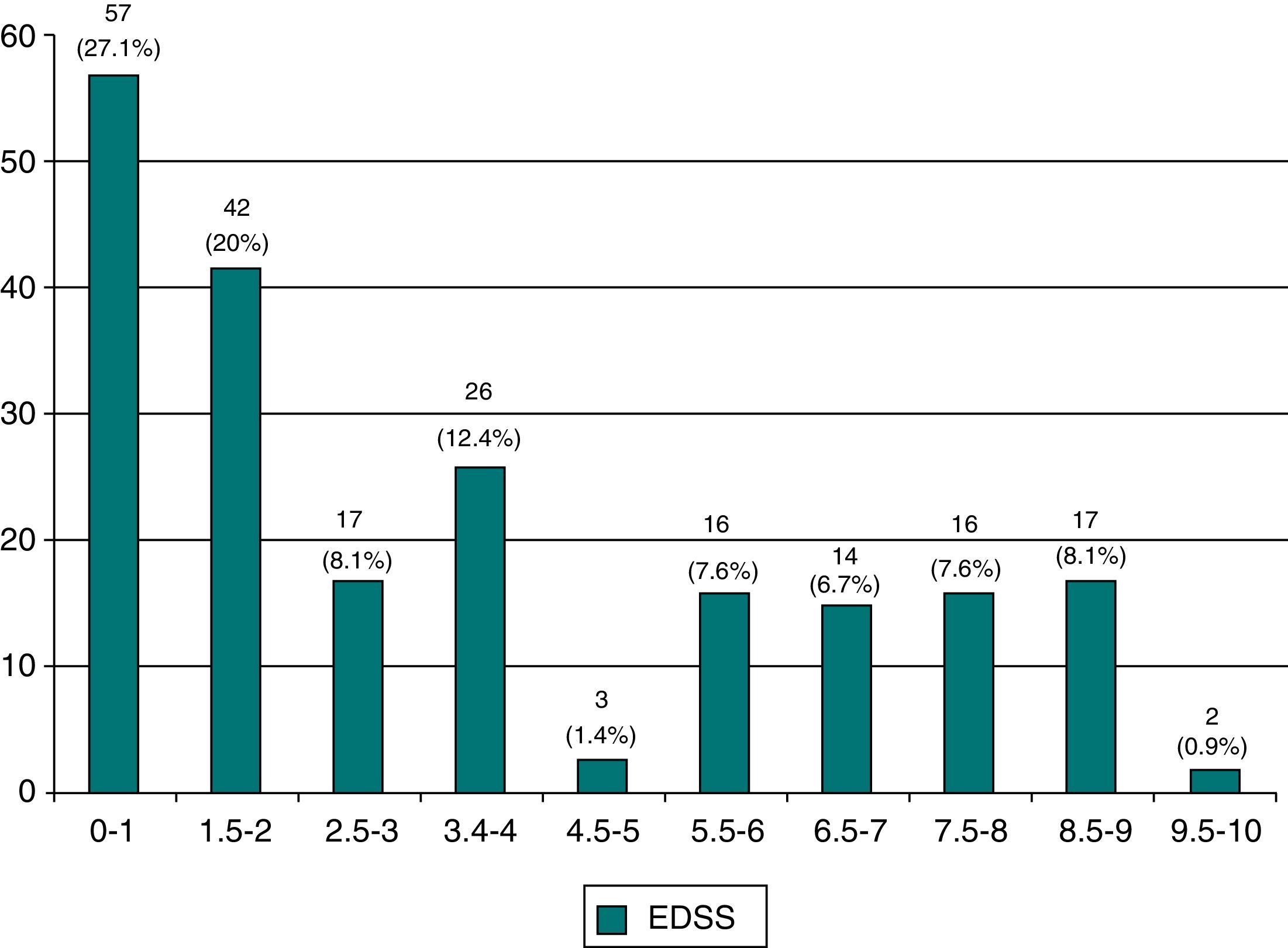
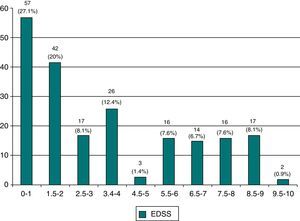
EDSS at last visit. According to the usual scale measuring disability status, 46.8% of the patients present minimal impairment (98 patients with an EDSS score≤2 [Fig. 3]). In contrast, 16.7% are highly dependent and unable to walk (35 patients with an EDSS score≥7.5).
- –
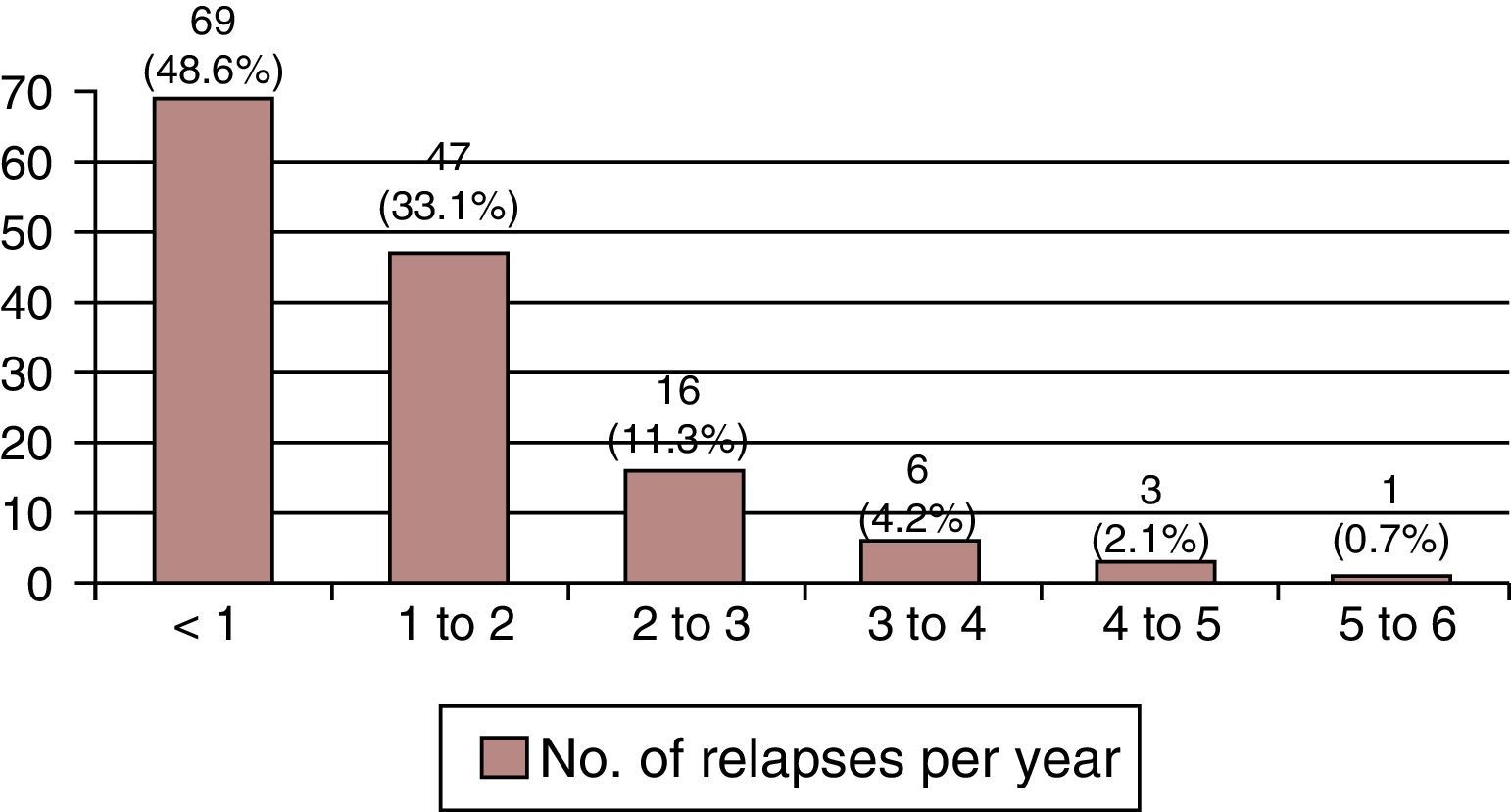
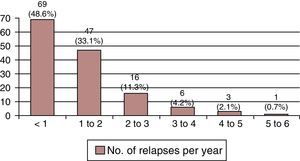
Relapses per year. Most patients with RRMS suffer 0 to 2 relapses per year (Fig. 4).
- –
MRI. An MRI scan was not performed for 3 of the 210 patients assessed here.
- –
CSF. A CSF study (whether a partial study or a complete study including oligoclonal bands [OCB] and immunology study [IS]) was conducted in 143 patients; results were abnormal in 108 patients or 75.5% of the total, with normal results in 35 (24.5% of the requested CSF studies).
Of the 108 patients showing pathological CSF results, 47 underwent a partial study only: 31 tested positive for OCB and 16 had positive results on the IS. In contrast, both studies were conducted in 61 patients: 39 showed abnormalities on both tests, 15 yielded a positive OCB with a negative IS, and seven showed negative OCB with a positive IS.
Six patients underwent a biochemistry study only (cases with long-standing MS). The OCB screen found negative results in 10 patients, while IS delivered negative results in 11 patients, and OCB and IS were negative in eight patients. Therefore, 35 patients showed normal results.
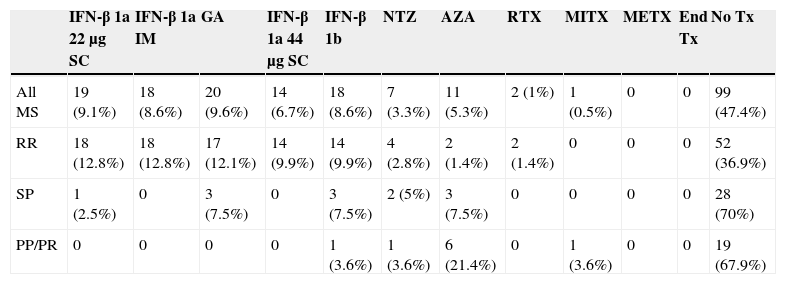
Specific treatmentsApproximately half of the patients (47.6%, 100 patients) were not given any disease-modifying treatments (Table 3).
MS-modifying treatments.
| IFN-β 1a 22μg SC | IFN-β 1a IM | GA | IFN-β 1a 44μg SC | IFN-β 1b | NTZ | AZA | RTX | MITX | METX | End Tx | No Tx | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| All MS | 19 (9.1%) | 18 (8.6%) | 20 (9.6%) | 14 (6.7%) | 18 (8.6%) | 7 (3.3%) | 11 (5.3%) | 2 (1%) | 1 (0.5%) | 0 | 0 | 99 (47.4%) |
| RR | 18 (12.8%) | 18 (12.8%) | 17 (12.1%) | 14 (9.9%) | 14 (9.9%) | 4 (2.8%) | 2 (1.4%) | 2 (1.4%) | 0 | 0 | 0 | 52 (36.9%) |
| SP | 1 (2.5%) | 0 | 3 (7.5%) | 0 | 3 (7.5%) | 2 (5%) | 3 (7.5%) | 0 | 0 | 0 | 0 | 28 (70%) |
| PP/PR | 0 | 0 | 0 | 0 | 1 (3.6%) | 1 (3.6%) | 6 (21.4%) | 0 | 1 (3.6%) | 0 | 0 | 19 (67.9%) |
Of the patients in the RRMS group, 71.9% were treated with IFN (64 in total: 50 with IFN-β 1a and 14 with IFN 1b), 19.1% were treated with glatiramer acetate (GA, 17 cases), 4.5% with natalizumab (NTZ, four cases), 2.2% with azathioprine (AZA, 2), and 2.2% with rituximab (RTX, 2, but one is receiving that treatment for chronic lymphocytic leukaemia).
Most of the 40 patients with SPMS were not taking any specific treatment for MS (28, 70%); however, 12 patients (30%) were treated at some point with immunomodulatory or immunosuppressant drugs: NTZ (2), AZA (3), IFN-β 1b (3), IFN-β 1a 22μg SC (1), and GA (3).
It is also common for patients with PPMS or PRMS to remain untreated, but we should explain that treatment with AZA (in six cases), IFN (1), NTZ (1), and mitoxantrone (MITX, 1) is occasionally prescribed due to erroneous diagnosis of the MS subtype or to a very aggressive progression (nine out of 28 patients, 32.1%).
Methotrexate (METX) is no longer administered (however, 11 of our patients had used it in the first few years of the 21st century). At that time, fingolimod was not yet fully authorised (it was requested for some cases due to intolerance to other drugs, pharmacophobia of non-oral routes, etc.). A total of six patients required treatment with MITX in the last 2 years of the study. We should mention that no stem cell studies or experimental treatment trials are being performed.
Most relevant motives for changing MS-modifying treatmentAmong these patients attended in La Rioja during this 10-year period, the main reasons for changing or even withdrawing medications were clinical exacerbation, adverse effects (cutaneous necrosis caused by injections, severe flu-like syndrome), and pregnancy. We only observed one case of acute hypertransaminasaemia caused by METX, severe thrombocytopenia caused by AZA, and a case of normocytic/normochromic anaemia in the context of treatment with IFN-β 1a 22μg SC that required multiple transfusions.
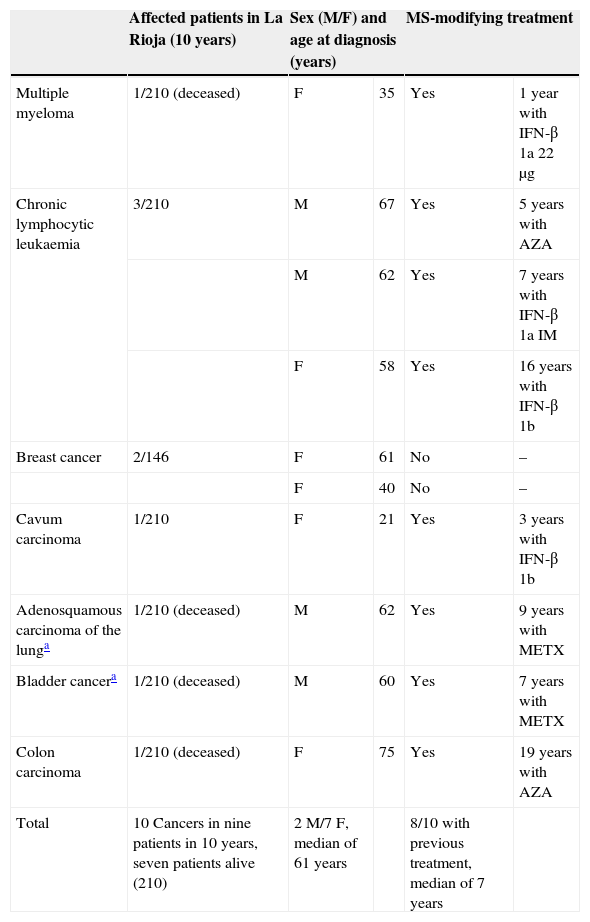
Cancer in MS patientsWe studied all tumours discovered during the 10-year study period. Four of our patients presented haematological cancer: one had very aggressive and eventually fatal multiple myeloma, and the remaining three developed chronic lymphocytic leukaemia. Other patients developed breast cancer (2), undifferentiated carcinoma (cavum lymphoepithelioma, 1), adenosquamous carcinoma of the lung (1), bladder cancer (1), and colon cancer (1) (Table 4). Cancer prevalence among our MS patients at the end of the study was 3.33% (with seven surviving oncology patients).
Cancer and MS.
| Affected patients in La Rioja (10 years) | Sex (M/F) and age at diagnosis (years) | MS-modifying treatment | |||
|---|---|---|---|---|---|
| Multiple myeloma | 1/210 (deceased) | F | 35 | Yes | 1 year with IFN-β 1a 22μg |
| Chronic lymphocytic leukaemia | 3/210 | M | 67 | Yes | 5 years with AZA |
| M | 62 | Yes | 7 years with IFN-β 1a IM | ||
| F | 58 | Yes | 16 years with IFN-β 1b | ||
| Breast cancer | 2/146 | F | 61 | No | – |
| F | 40 | No | – | ||
| Cavum carcinoma | 1/210 | F | 21 | Yes | 3 years with IFN-β 1b |
| Adenosquamous carcinoma of the lunga | 1/210 (deceased) | M | 62 | Yes | 9 years with METX |
| Bladder cancera | 1/210 (deceased) | M | 60 | Yes | 7 years with METX |
| Colon carcinoma | 1/210 (deceased) | F | 75 | Yes | 19 years with AZA |
| Total | 10 Cancers in nine patients in 10 years, seven patients alive (210) | 2 M/7 F, median of 61 years | 8/10 with previous treatment, median of 7 years | ||
We identified seven families in which multiple individuals were affected. Two families have three affected members, consisting of the mother and two children (two daughters in one case, and a son and a daughter in the other); progression was strikingly aggressive in both families. We found two affected siblings in three families (a family with two sons and two families with two daughters with MS). In another family, the affected members were a girl and a cousin on her father's side; and in the last family, a nephew and his aunt.
DiscussionIf we compare our data to the recent review article by De Sá, “Epidemiology of multiple sclerosis in Portugal and Spain”,30 we observe that the prevalence in La Rioja (65 cases/100000 population) is similar to rates published in recent years. However, we should highlight the study by Fernández et al.19 showing a high prevalence rate of 125 cases/100000 population in Málaga province obtained by the capture-recapture method. This points to a need for further studies in other Spanish regions, using data collection methods other than those drawing from traditional databases. These studies would determine whether discrepancies between regions are due to faulty data collection or to the different characteristics that could affect MS (genetic basis, infections, etc.). Despite not having contacted primary care doctors or nursing home doctors, we were able to collect a significant number of cases using different databases (central hospital records, ARDEM, hospital pharmacy department, and neurologists’ records), resulting in a study with good reliability.
Our study revealed differences in MS progression times between patients listed in different databases. Most patients with long-term MS were obtained from the ARDEM database, while recently diagnosed patients with low levels of disability were recruited from hospital records. The absence of long-term patients in the hospital records could be due to lack of follow-up.
Incidence rate (3.5 cases/100000 population-years) and the mortality rate (0.26 cases/100000 population) are similar to those published in other articles.23
We also found relevant differences in age at onset, with mean ages in the 20-29 year range for RRMS vs the 40-49 year range for the primary (initially progressive) types. In our study, mean age of onset in this latter group is slightly higher than in other series. The percentage of children and adolescents affected (up to age 16) was 3.3%, which coincides with that reported by other articles.31
There is no predominant clinical pattern during the first relapse, although infratentorial impairment is slightly more frequent.
Regarding complementary tests, MRI studies are currently requested on a systematic basis, as is OCB screening in CSF. However, MS diagnosis was based on myelography findings, some years ago, and this explains why some patients did not undergo MRI studies.
The most frequently used treatments in La Rioja are interferons, in more than 70%. However, we should not overlook that almost half of the patients with MS remain untreated for different reasons, such as not needing treatment, being at a very advanced stage of the disease, or having a subtype for which there is no indicated treatment. We do not know the impact of immunomodulatory or immunosuppressant drugs on disability or survival, since, IFN, the first disease-modifying drug, was first marketed in 1993,32 which is a short time interval for a long-term disease. In fact, the degree of disability of MS patients today, as measured on the EDSS, remains very high (almost 17% of the patients are very disabled).
Regarding iatrogenic issues, first-line drugs present very few severe adverse effects, and their safety profile is therefore considered adequate. The studies published to date33 state that there is no relationship between taking immunomodulatory treatment and developing cancer. Although finding three cases of chronic lymphocytic leukaemia out of our 210 patients is surprising, and so is the fact that medication for MS was used by most patients with cancer, our limited number of patients does not enable us to obtain conclusive results. The French study by Lebrun et al.34,35 mentions finding both cancer and MS in 1.75% of their patients, while in La Rioja this rate reaches 3.33%. Furthermore, the French researchers report malignant leukaemia/lymphoma type tumours in 5.9%, compared to 42.86% in patients from La Rioja (considering current prevalence and the bias inherent to using a very reduced sample).
The contribution of a genetic component seems obvious given the number of families with multiple patients and the aggressiveness of the disease affecting some of them.
Our study limitations include being a retrospective study, the possibility of having missed patients who presented clinical signs during the study period but were not formally diagnosed until a later date, and not using the 2010 McDonald criteria, which would have resulted in a delayed diagnosis for some patients. Another limitation was the possibility of missing any severely ill patients who do not make scheduled visits to neurology departments.
Therefore, prevalence and incidence rates of MS in the region of La Rioja are in line with the mean values obtained by studies conducted in other Spanish regions. However, new studies in other Spanish provinces will be needed for a precise calculation of the prevalence rate in Spain. These studies should use a variety of data collection methods to reinforce the validity of results.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Bártulos Iglesias M, Marzo Sola ME, Estrella Ruiz LA, Bravo Anguiano Y. Estudio epidemiológico de la esclerosis múltiple en La Rioja. Neurología. 2015;30:552–560.