To study the efficacy of manual therapy in the treatment of tension-type headache (TTH) by assessing the quality of randomised control trials (RCTs) published from the year 2000 to April 2013.
MethodsA search was performed in the following databases: MEDLINE, EBSCO, CINAHL, SCOPUS, PEDRO and OVID. An analysis was made of RCT including patients with TTH receiving any manual therapy, and assessing outcome measures including the intensity, and frequency or duration of the headache. Two independent referees reviewed the methodological quality of RCTs using the Jadad scale. Data from the studies were extracted by two different reviewers.
ResultsA total of fourteen RCTs were selected. Twelve studies showed acceptable quality (Jadad scale ≥3), and the remaining 2 had low quality (Jadad=2). The studies showed positive results, including reduction in headache intensity and/or frequency, reduction of medication consumption, and improvement in quality of life.
ConclusionsThe effectiveness of manual therapy for TTH cannot be completely assessed due to the heterogeneity in study design, outcome measures, and different treatments. Nevertheless, the results suggest patients with TTH receiving manual therapies showed better progress than those receiving conventional treatment or placebo. Further studies of high quality using manual therapy protocols, and also including standardised outcome measures, are now needed to clarify the efficacy of manual therapy in the management of TTH.
Estudiar la eficacia de la terapia manual en el tratamiento de la cefalea tensional (CT) valorando los estudios controlados aleatorizados (ECA) publicados desde el año 2000 hasta abril del 2013.
MétodosSe realizó la búsqueda en las bases de datos MEDLINE, EBSCO, CINAHL, SCOPUS, PEDRO y OVID. Se incluyeron ECA que analizasen a pacientes con CT tratados con terapia manual y que recogiesen como variable de resultado la intensidad, frecuencia, duración del dolor de cabeza. La calidad metodológica fue valorada por 2 revisores independientes mediante la escala Jadad. Los datos de los ECA fueron extraídos por 2 revisores.
ResultadosSe seleccionaron 14 ECA. Doce de ellos se consideraron de calidad aceptable (Jadad≥3) y 2 de baja (Jadad=2). Los estudios mostraron resultados positivos obteniendo disminución de la intensidad y/o frecuencia de cefaleas, reducción del consumo de medicamentos y mejora de la calidad de vida en pacientes con CT.
ConclusionesDebido a la heterogeneidad en diseños, instrumentos de medida y tratamientos de los estudios, no es posible obtener conclusiones definitivas sobre la eficacia de la terapia manual en pacientes con CT aunque se aprecien efectos beneficiosos. No obstante, el análisis de los estudios indica que, al recibir tratamiento con terapia manual, los pacientes con CT evolucionaron de forma más favorable respecto a aquellos que recibieron tratamiento habitual o un tratamiento placebo. Se requiere un mayor número de estudios con mayor calidad metodológica, así como mayor homogeneidad de los tratamientos y de los métodos de valoración de los resultados, para determinar la eficacia de la terapia manual en la CT.
Tension-type headache (TTH) is considered a major public health problem by the World Health Organization due to its high prevalence and great socioeconomic impact.1,2 The prevalence of TTH, which seems to be higher in Europe (80%) than in Asia or America (20%-30%), is estimated at approximately 40% globally.3 It is more frequent among women (woman-to-man ratio 5:4) and peak prevalence occurs at ages 30 to 39.4
TTH is the most frequent type of primary headache; the International Headache Society further classifies it into infrequent episodic, frequent episodic, and chronic TTH.5 According to the diagnostic criteria established by the International Headache Society, TTH is characterised by at least 10 episodes per year on less than 1 day per month on average, each lasting between 30minutes and 7 days, and the pain should include at least 2 of the following characteristics: bilateral location, non-pulsating quality, mild to moderate intensity, and not aggravated by routine physical activity. In addition to the previously described symptoms, TTH does not present with nausea or vomiting; phonophobia or photophobia may occur in some cases but they do not present simultaneously during the same episode.5
Despite advances in the knowledge of TTH pathophysiology, its origin is not yet fully understood. For some authors, peripheral nociceptive mechanisms seem to be the main cause of episodic TTH, whereas chronic TTH may be caused by central sensitisation.6,7 Sohn et al.8 found that patients with TTH presented greater sensitivity in pericranial tissues. Pericranial pain sensitivity, along with other exacerbating factors (stress, caffeine abuse, unhealthy eating habits, or sleep disorders) may lead to excitation of the central nervous system. Prolonged nociceptive stimulation of myofascial tissues may be the cause of progression from episodic TTH to chronic TTH.7,9,10
The hypothesis that myofascial tissue may be a source of nociception in TTH is based on numerous studies showing that referred pain originating in myofascial trigger points (MTP) reproduces headache in patients with TTH.11–15 According to all these studies, MTP were associated with TTH and led to greater symptom severity (increased intensity, frequency, and/or duration).9–15 Harden et al.16 demonstrated that patients with TTH presenting more active MTP in the head and neck experienced greater pain intensity and frequency and were partially relieved by botulinum toxin injections into those MTP.
There is controversy regarding therapeutic management of patients with TTH, which can be either pharmacological or non-pharmacological. Patients with infrequent episodic TTH can be successfully treated with non-steroidal anti-inflammatory drugs, while those with frequent episodic or chronic TTH usually receive tricyclic antidepressants such as amitriptyline.17 However, self-medication is very frequent and may lead to medication overuse headache.4 Non-pharmacological treatment includes psychological techniques (relaxation exercises, cognitive-behavioural therapy) and physiotherapy.17 One of the most frequent approaches in physiotherapy is manual therapy. In fact, this type of therapy is considered a satisfactory method for reducing excitability and sensitivity of the central nervous system as it decreases overall sensitivity to pain.18 Manual therapy, which in many cases focuses on the vertebral column, has been shown to improve headache symptoms that frequently arise from the soft tissues of the head and neck.19 Mechanical impulses in manual therapy are believed to initiate a cascade of neurophysiological changes in the central and peripheral nervous systems, which in turn provokes clinical changes.20 Mechanical impulses therefore stimulate mechanical receptors and inhibit nociceptors, resulting in decreased levels of pain.21
In the past few years, several systematic reviews addressing manual therapy for TTH have been published.19,22–25 All of them agree on the benefits of manual therapy for TTH; however, they also agree on the scarce clinical evidence available and the need for further studies on this topic. Some of these review articles have focused on only one manual technique: manipulation.22,25 Several studies on the effectiveness of different manual therapy techniques for TTH have been conducted in recent years; however, these have not been included in the already mentioned review studies. The present systematic review aims to evaluate the quality of the randomised clinical trials (RCT) on manual therapy for TTH management published in the past decade and assesses the effectiveness of these therapeutic interventions.
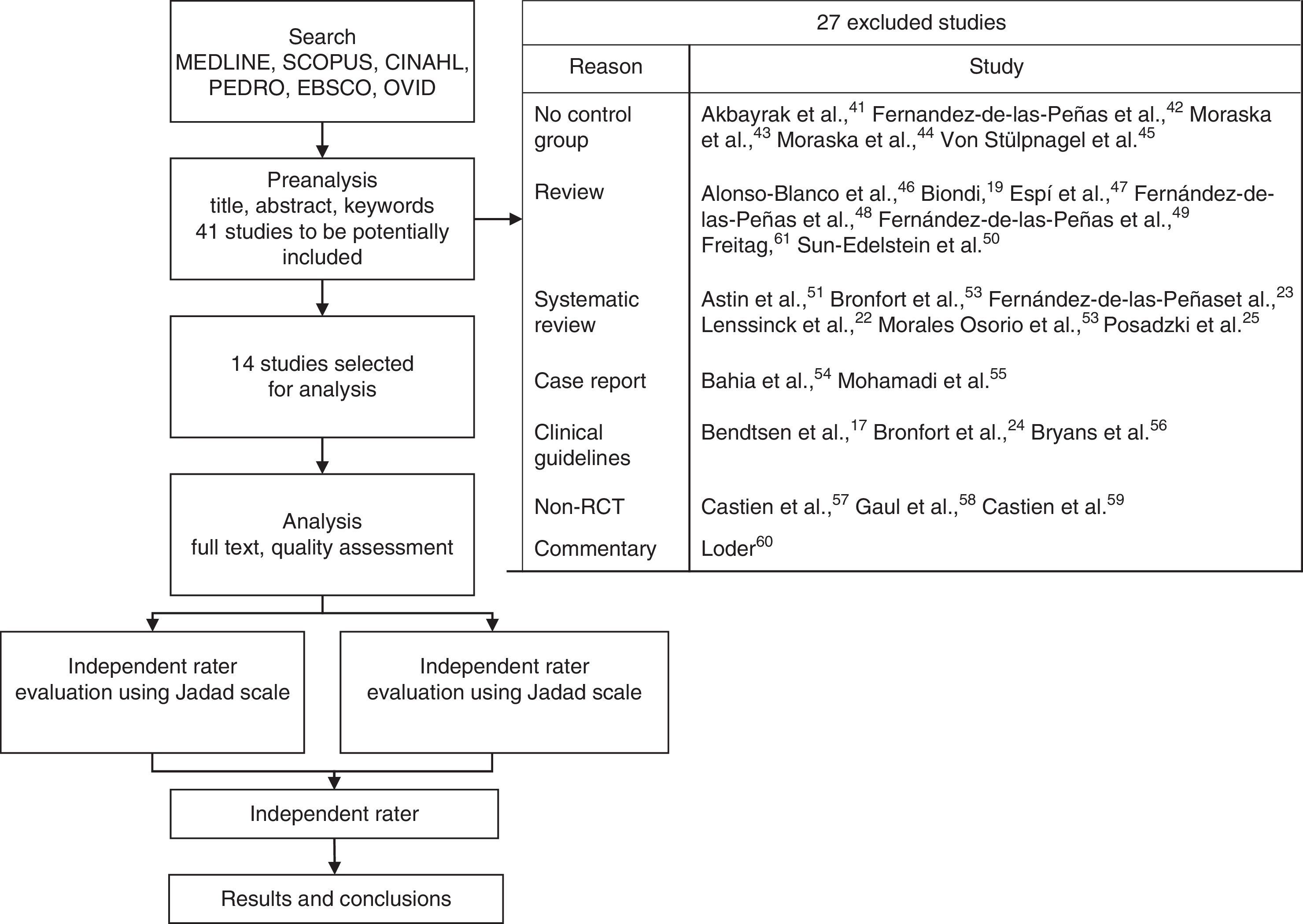
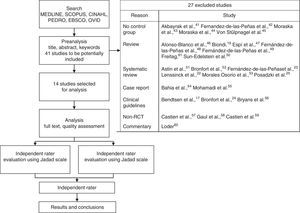
Material and methodsSearch methodologyWe conducted a bibliographical search on MEDLINE, EBSCO, Scopus, CINAHL, Ovid, and PEDro databases using the following keywords: ‘manual therapy’, ‘spinal manipulation’, ‘soft tissue technique’, ‘chiropractic’, and ‘osteopathy’, combined with ‘tension-type headache’. We obtained a total of 41 studies, which were assessed by 2 independent reviewers. The assessment was based on the information provided in the abstract, title, and keywords. Fourteen studies were finally included; these were accessed in full-text format and thoroughly evaluated. The last day of search was 5 April 2013.
Inclusion criteriaThe studies had to meet the following inclusion criteria: (1) being an RCT; (2) including adult patients diagnosed with TTH regardless of age and sex; (3) therapeutic intervention was based on manual therapy; (4) describing the therapeutic procedure; (5) the control group received a placebo treatment, standard treatment for TTH, or no therapy at all; (6) published in scientific journals between 2000 and 2013; and (7) published in either Spanish or English.
Data extractionTwo independent raters extracted data from each of the studies, as in the stage of study selection. From each study, the following data were gathered: participants (inclusion and exclusion criteria), study design, applied interventions, analysed measurements, type of blinding, and results.
Assessment of study qualityWe used the Jadad scale to assess methodological quality of the studies included in the present review. This tool, which is one of the scales most widely used by the healthcare community,26 assesses design quality in clinical trials and is scored on a 5-point scale based on the following questions: ‘Is the study described as randomised?’, ‘Is the method for randomisation described and is it appropriate?’, ‘Is the study described as double-blind?’, ‘Is the method of blinding described and is it appropriate?’, and ‘Is there a description of drop-outs and withdrawals?’.
Two independent raters used the same methodology to analyse the quality of all the articles selected. Interrater disagreement was solved by consensus; in some cases, a third reviewer was needed.
ResultsOf a total of 41 articles, 14 met the inclusion criteria and were therefore included in the systematic review.27–40Fig. 1 shows the stages of the systematic review and lists the excluded articles.17,19,22–25,41–61
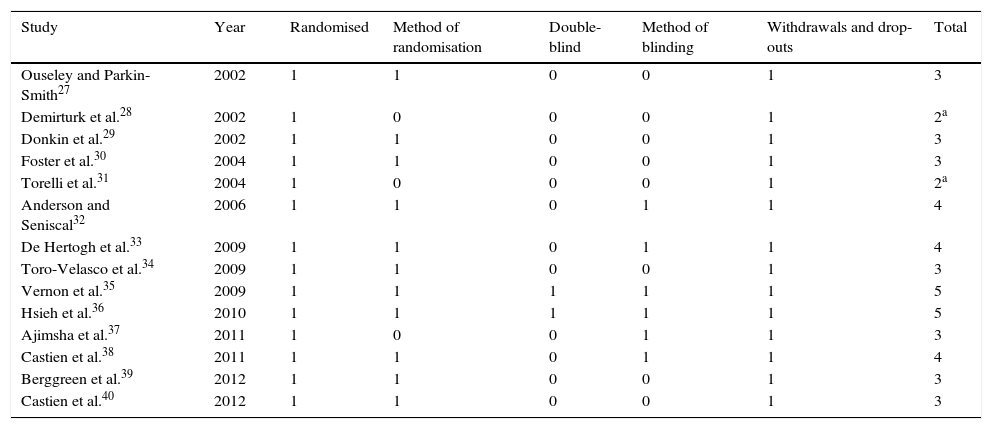
Methodological quality of the studiesMethodological quality was considered acceptable in 12 (85%) of the studies27,29,30,32–40 and poor in the remaining 2.28,31 Design quality was evaluated based on such parameters as randomisation, method of randomisation, double-blinding, method of blinding, and description of withdrawals and drop-outs (Table 1). Inter-rater agreement on methodological quality was high (Kappa coefficient: 0.8).
Analysis of the studies included in the review using the Jadad scale.
| Study | Year | Randomised | Method of randomisation | Double-blind | Method of blinding | Withdrawals and drop-outs | Total |
|---|---|---|---|---|---|---|---|
| Ouseley and Parkin-Smith27 | 2002 | 1 | 1 | 0 | 0 | 1 | 3 |
| Demirturk et al.28 | 2002 | 1 | 0 | 0 | 0 | 1 | 2a |
| Donkin et al.29 | 2002 | 1 | 1 | 0 | 0 | 1 | 3 |
| Foster et al.30 | 2004 | 1 | 1 | 0 | 0 | 1 | 3 |
| Torelli et al.31 | 2004 | 1 | 0 | 0 | 0 | 1 | 2a |
| Anderson and Seniscal32 | 2006 | 1 | 1 | 0 | 1 | 1 | 4 |
| De Hertogh et al.33 | 2009 | 1 | 1 | 0 | 1 | 1 | 4 |
| Toro-Velasco et al.34 | 2009 | 1 | 1 | 0 | 0 | 1 | 3 |
| Vernon et al.35 | 2009 | 1 | 1 | 1 | 1 | 1 | 5 |
| Hsieh et al.36 | 2010 | 1 | 1 | 1 | 1 | 1 | 5 |
| Ajimsha et al.37 | 2011 | 1 | 0 | 0 | 1 | 1 | 3 |
| Castien et al.38 | 2011 | 1 | 1 | 0 | 1 | 1 | 4 |
| Berggreen et al.39 | 2012 | 1 | 1 | 0 | 0 | 1 | 3 |
| Castien et al.40 | 2012 | 1 | 1 | 0 | 0 | 1 | 3 |
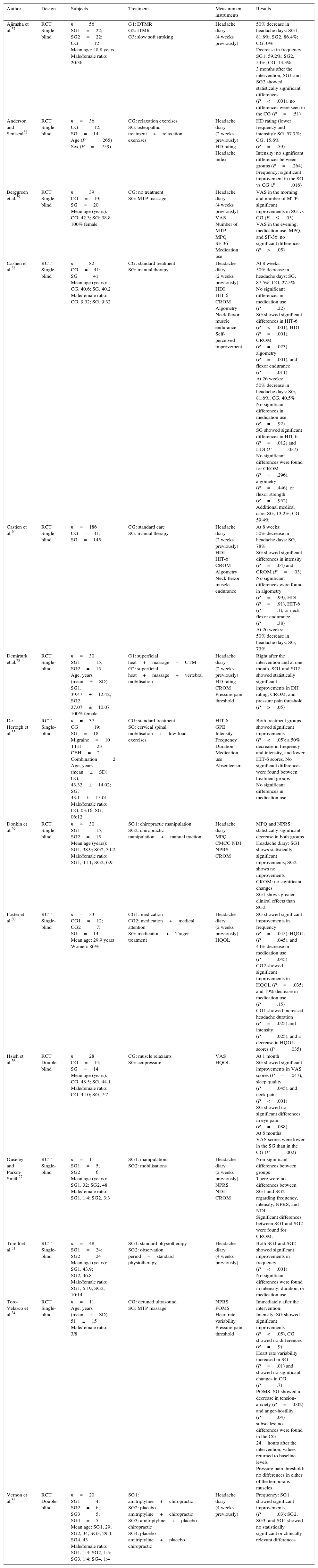
The studies included assessed effectiveness of physiotherapy (muscle and/or joint treatment) in patients diagnosed with frequent episodic or chronic TTH. The most frequent inclusion criterion27–36,38–40 among studies was diagnosis of TTH according to the classification of the International Headache Society. However, one of the studies37 did not describe the inclusion criteria and 6 studies only included patients with chronic TTH.27,28,34,38–40 Likewise, 3 studies30,33,36 included patients with chronic headache but did not specify whether it was TTH or some other type of chronic headache.
All the studies reported drop-outs during follow-up. Although most of the studies lost fewer than 7 patients during the entire follow-up period, 2 studies reported 13 and 18 drop-outs, respectively.31,40
Characteristics of the interventionsTherapeutic interventions using manual therapy showed a high variability among the 14 studies analysed. Articulatory techniques were used in 4 of them,27,29,30,32 soft tissue therapy in 5,31,34,36,37,39 and a combination of both types of interventions in the remaining 5.28,33,35,38,61
Regarding articulatory techniques, one study30 applied the Trager approach (slow rhythmic movements of joints and relaxation techniques). This study included 2 control groups: one of them was treated with medication exclusively while the other received medication and was also followed up by a doctor who performed physical examinations and recorded any findings on their clinical histories. Donkin et al.29 applied cervical manipulation to 2 groups, one of which also underwent manual cervical traction. These authors conducted 9 treatment sessions for 5 weeks (2 sessions per week). Ouseley and Parkin-Smith27 performed chiropractic spinal manipulations in one group and spinal mobilisation in flexion, extension, lateral flexion, and rotation in another group. In the study by Anderson and Seniscal,32 the study group performed relaxation techniques and received osteopathic treatment, whereas the control group only performed relaxation techniques. Patients in both groups were given an audiotape in order to be able to do relaxation exercises at home every day.
Regarding soft tissue therapy, one of the studies31 analysed the effect of massage therapy, relaxation techniques, mild muscle stretching, and daily training of pericranial, neck, and shoulder muscles. One group received physiotherapy while the other group underwent an 8-week observation period by a neurologist before receiving physiotherapy. Toro-Velasco et al.34 applied a massage protocol to inactivate muscle trigger points in the head and neck. The placebo administered to the control group consisted of detuned ultrasound in the head and neck for 40minutes, the same amount of time as the intervention in the treatment group. The experimental group in the study by Hsieh et al.36 was treated with acupressure and a placebo consisting of a vitamin B complex (15mg/day). The control group received muscle relaxants (mephenoxalone) for one month, which was the treatment period for both groups.
Ajimsha et al.37 studied myofascial release. These authors divided patients into 3 groups according to the treatment they received: direct technique myofascial release, indirect technique myofascial release, and placebo (slow soft stroking). Sessions lasted one hour and they were held twice a week for 12 weeks.
In the study by Berggreen et al.,39 patients received MTP massage once per week for 10 weeks, whereas controls received no treatment.
Lastly, the remaining studies combined both techniques (joint and soft tissue therapy). De Hertogh et al.33 analysed manual therapy consisting of joint mobilisations of the vertebral column (low- and/or high-velocity) and a programme of low-load endurance exercises (cranio-cervical flexion). Both the experimental and the control group received standard care following the Dutch General Practitioners Guideline for headache.
Vernon et al.35 combined manual therapy and normal pharmacological treatment (amitriptyline 10mg/day for 2 weeks and 25mg/day for 12 additional weeks). Chiropractic treatment consisted of gentle massaging and low-amplitude high-velocity manipulations of the affected joints from the occiput to the third thoracic vertebra. Sham chiropractic manipulation was performed on a drop table; these tables have drop pieces that make a noise when they move, thus preventing patients from hearing the cracking sound as joints adjust. The therapist placed controls in manipulation position. When applying a thrust on the patient, however, no cracking sound could be heard but rather the sound produced by the drop piece, which made controls think they had received manipulations (placebo effect). The control group received, in a manner indistinguishable from that used on the experimental group, a placebo consisting of tablets with identical characteristics and flavour to amitriptyline.
Demirturk et al.28 separated patients into 2 groups. One received connective tissue manipulation and the other, neck mobilisation. In addition, superficial heat and classical massage of neck and upper back were applied to all participants before the specific interventions. In the study by Castien et al.,38 the experimental group received neck and thoracic mobilisation and posture correction exercises, whereas the control group received standard care following the Dutch general practice guidelines for headache management. In a subsequent study by these authors,40 the control group received the same intervention as in the previous trial. The intervention included low- and/or high-velocity mobilisation of the cervical and upper thoracic spine, soft tissue techniques, home exercises, craniocervical muscle endurance exercises, and posture correction exercises. Table 2 summarises the general characteristics of the studies included in this review: study design, participants, treatment, measurement tools, and results.
General characteristics of the study.
| Author | Design | Subjects | Treatment | Measurement instruments | Results |
|---|---|---|---|---|---|
| Ajimsha et al.37 | RCT Single-blind | n=56 SG1=22; SG2=22; CG=12 Mean age: 48.8 years Male/female ratio: 20:36 | G1: DTMR G2: ITMR G3: slow soft stroking | Headache diary (4 weeks previously) | 50% decrease in headache days: SG1, 81.8%; SG2, 86.4%; CG, 0% Decrease in frequency: SG1, 59.2%; SG2, 54%; CG, 13.3% 3 months after the intervention, SG1 and SG2 showed statistically significant differences (P<.001), no differences were seen in the CG (P=.51) |
| Anderson and Seniscal32 | RCT Single-blind | n=36 CG=12; SG=14 Age (P=.265) Sex (P=.759) | CG: relaxation exercises SG: osteopathic treatment+relaxation exercises | Headache diary (2 weeks previously) HD rating Headache index | HD rating (lower frequency and intensity): SG, 57.7%; CG, 15.6% (P=.59) Intensity: no significant differences between groups (P=.264) Frequency: significant improvement in the SG vs CG (P=.016) |
| Berggreen et al.39 | RCT Single-blind | n=39 CG=19; SG=20 Mean age (years): CG: 42.3; SG: 38.8 100% female | CG: no treatment SG: MTP massage | Headache diary (4 weeks previously) VAS Number of MTP MPQ SF-36 Medication use | VAS in the morning and number of MTP: significant improvements in SG vs CG (P≤.05) VAS in the evening, medication use, MPQ, and SF-36: no significant differences (P>.05) |
| Castien et al.38 | RCT Single-blind | n=82 CG=41; SG=41 Mean age (years): CG, 40.6; SG, 40.2 Male/female ratio: CG, 9:32; SG, 9:32 | CG: standard treatment SG: manual therapy | Headache diary (2 weeks previously) HDI HIT-6 CROM Algometry Neck flexor muscle endurance Self-perceived improvement | At 8 weeks: 50% decrease in headache days: SG, 87.5%; CG, 27.5% No significant differences in medication use (P=.22) SG showed significant differences in HIT-6 (P<.001), HDI (P=.001), CROM (P=.023), algometry (P=.001), and flexor endurance (P=.011) At 26 weeks: 50% decrease in headache days: SG, 81.6%; CG, 40.5% No significant differences in medication use (P=.92) SG showed significant differences in HIT-6 (P=.012) and HDI (P=.037) No significant differences were found for CROM (P=.296), algometry (P=.446), or flexor strength (P=.952) Additional medical care: SG, 13.2%; CG, 59.4% |
| Castien et al.40 | RCT Single-blind | n=186 CG=41; SG=145 | CG: standard care SG: manual therapy | Headache diary (2 weeks previously) HDI HIT-6 CROM Algometry Neck flexor muscle endurance | At 8 weeks: 50% decrease in headache days: SG, 78% SG showed significant differences in intensity (P=.04) and CROM (P=.03) No significant differences were found in algometry (P=.99), HDI (P=.91), HIT-6 (P=.1), or neck flexor endurance (P=.38) At 26 weeks: 50% decrease in headache days: SG, 73% |
| Demirturk et al.28 | RCT Single-blind | n=30 SG1=15; SG2=15 Age, years (mean±SD): SG1, 39.47±12.42; SG2, 37.07±10.07 100% female | G1: superficial heat+massage+CTM G2: superficial heat+massage+vertebral mobilisation | Headache diary (2 weeks previously) HD rating CROM Pressure pain threshold | Right after the intervention and at one month, SG1 and SG2 showed statistically significant improvements in DH rating, CROM, and pressure pain threshold (P>.05) |
| De Hertogh et al.33 | RCT Single-blind | n=37 CG=19; SG=18 Migraine=10 TTH=23 CEH=2 Combination=2 Age, years (mean±SD): CG, 43.32±14.02; SG, 43.1±15.01 Male/female ratio: CG, 03:16; SG, 06:12 | CG: standard treatment SG: cervical spinal mobilisation+low-load exercises | HIT-6 GPE Intensity Frequency Duration Medication use Absenteeism | Both treatment groups showed significant improvements (P<.05): a 50% decrease in frequency and intensity, and lower HIT-6 scores. No significant differences were found between treatment groups No significant differences in medication use |
| Donkin et al.29 | RCT Single-blind | n=30 SG1=15; SG2=15 Mean age (years): SG1, 38.9; SG2, 34.2 Male/female ratio: SG1, 4:11; SG2, 6:9 | SG1: chiropractic manipulation SG2: chiropractic manipulation+manual traction | Headache diary MPQ CMCC NDI NPRS CROM | MPQ and NPRS: statistically significant decrease in both groups Headache diary: SG1 shows statistically significant improvements; SG2 shows no improvements CROM: no significant changes SG1 shows greater clinical effects than SG2 |
| Foster et al.30 | RCT Single-blind | n=33 CG1=12; CG2=7; SG=14 Mean age: 29.9 years Women: 86% | CG1: medication CG2: medication+medical attention SG: medication+Trager treatment | Headache diary (2 weeks previously) HQOL | SG showed significant improvements in frequency (P=.045), HQOL (P=.045), and 44% decrease in medication use (P=.045) CG2 showed significant improvements in HQOL (P=.035) and 19% decrease in medication use (P=.15) CG1 showed increased headache duration (P=.025) and intensity (P=.025), and a decrease in HQOL scores (P=.035) |
| Hsieh et al.36 | RCT Double-blind | n=28 CG=14; SG=14 Mean age (years): CG, 48.5; SG, 44.1 Male/female ratio: CG, 4:10; SG, 7:7 | CG: muscle relaxants SG: acupressure | VAS HQOL | At 1 month SG showed significant improvements in VAS scores (P=.047), sleep quality (P=.045), and neck pain (P<.001) SG showed no significant differences in eye pain (P=.088) At 6 months VAS scores were lower in the SG than in the CG (P=.002) |
| Ouseley and Parkin-Smith27 | RCT Single-blind | n=11 SG1=5; SG2=6 Mean age (years): SG1, 32; SG2, 48 Male/female ratio: SG1, 1:4; SG2, 3:3 | SG1: manipulations SG2: mobilisations | Headache diary (2 weeks previously) NPRS NDI CROM | Non-significant differences between groups There were no differences between SG1 and SG2 regarding frequency, intensity, NPRS, and NDI Significant differences between SG1 and SG2 were found for CROM. |
| Torelli et al.31 | RCT Single-blind | n=48 SG1=24; SG2=24 Mean age (years): SG1, 43.9; SG2, 46.8 Male/female ratio: SG1, 5:19; SG2, 10:14 | SG1: standard physiotherapy SG2: observation period+standard physiotherapy | Headache diary (4 weeks previously) | Both SG1 and SG2 showed significant improvements in frequency (P<.001) No significant differences were found in intensity, duration, or medication use |
| Toro-Velasco et al.34 | RCT Single-blind | n=11 Age, years (mean±SD): 51±15 Male/female ratio: 3/8 | CG: detuned ultrasound SG: MTP massage | NPRS POMS Heart rate variability Pressure pain threshold | Immediately after the intervention: Intensity: SG showed significant improvements (P<.05), CG showed no differences (P=.9) Heart rate variability increased in SG (P=.01) and showed no significant changes in CG (P=.7) POMS: SG showed a decrease in tension-anxiety (P=.002) and anger-hostility (P=.04) subscales; no differences were found in the CG 24hours after the intervention, values returned to baseline levels Pressure pain threshold: no differences in either of the temporalis muscles |
| Vernon et al.35 | RCT Double-blind | n=20 SG1=4; SG2=6; SG3=5; SG4=5 Mean age: SG1, 29; SG2, 34; SG3, 29.4; SG4, 43 Male/female ratio: SG1, 1:3; SG2, 1:5; SG3, 1:4; SG4, 1:4 | SG1: amitriptyline+chiropractic SG2: placebo amitriptyline+chiropractic SG3: amitriptyline+placebo chiropractic SG4: placebo amitriptyline+placebo chiropractic | Headache diary (4 weeks previously) | Frequency: SG1 showed significant improvements (P=.03); SG2, SG3, and SG4 showed no statistically significant or clinically relevant differences |
TTH: tension-type headache; CEH: cervicogenic headache; CROM: cervical range of movement; SD: standard deviation; RCT: randomised controlled trial; VAS: visual analogue scale; CG: control group; SG: study group; GPE: global perceived effect; HD rating: index of headaches recorded in a headache diary; HDI: headache disability inventory; HIT-6: headache impact test-6; HQOL: headache quality of life; MPQ: McGill pain questionnaire; CTM: connective tissue manipulation; NDI: neck disability index; NPRS: numeric pain rating scale; MTP: myofascial trigger point; POMS: profile of mood states; SF-36: short form-36 health survey; DTMR: direct technique myofascial release; ITMR: indirect technique myofascial release.
All the studies including interventions based on manual therapy reported positive results for patients with TTH.
Eleven studies27–33,35,37,38,40 analysed changes in headache frequency after the intervention. All groups receiving manual therapy showed a statistically significant decrease in headache frequency. One of the studies33 reported improvements both in the control and the experimental groups, while another study35 reported positive results only in the group treated with chiropractic and amitriptyline.
Ten studies27–29,31–34,36,39,40 analysed changes in headache intensity. Eight of these27–29,32–34,36,40 reported a statistically significant reduction in the experimental group after manual therapy. However, in 2 studies31,39 intensity was not significantly reduced. Another 2 studies32,33 reported reductions in intensity for both the experimental and the control groups.
Reduction in analgesic use was assessed in 5 studies30,31,33,38,39; although all of them reported changes, these were not statistically significant in all cases. Only one study30 showed a significant reduction in the experimental group and in one of the controls who was followed up.
Quality of life was evaluated using different questionnaires in 7 of the studies included in our review.29,30,33,36,38–40 One39 found no significant changes whereas the remaining 629,30,33,36,38,40 reported improvements in quality of life. In addition, 2 of these studies30,33 reported improvements in both the experimental and the control groups.
Improvements in neck mobility were assessed in 4 studies.27,28,38,40 All the groups receiving manual therapy showed increased neck mobility.
Lastly, 3 studies28,38,40 analysed changes in pressure pain threshold and reported positive changes for all study groups receiving manual therapy.
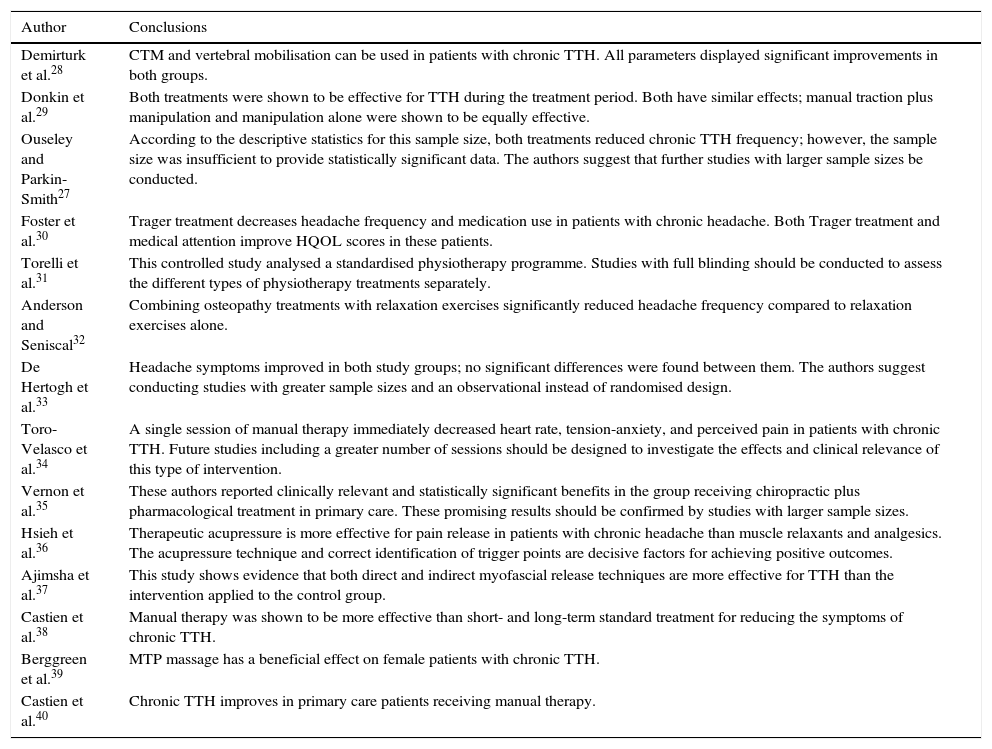
Table 2 shows the characteristics of the studies included in this review, subjects, treatments, measurement tools, and results. Table 3 shows the results of the randomised controlled trials.
Conclusions of the studies included in this systematic review.
| Author | Conclusions |
|---|---|
| Demirturk et al.28 | CTM and vertebral mobilisation can be used in patients with chronic TTH. All parameters displayed significant improvements in both groups. |
| Donkin et al.29 | Both treatments were shown to be effective for TTH during the treatment period. Both have similar effects; manual traction plus manipulation and manipulation alone were shown to be equally effective. |
| Ouseley and Parkin-Smith27 | According to the descriptive statistics for this sample size, both treatments reduced chronic TTH frequency; however, the sample size was insufficient to provide statistically significant data. The authors suggest that further studies with larger sample sizes be conducted. |
| Foster et al.30 | Trager treatment decreases headache frequency and medication use in patients with chronic headache. Both Trager treatment and medical attention improve HQOL scores in these patients. |
| Torelli et al.31 | This controlled study analysed a standardised physiotherapy programme. Studies with full blinding should be conducted to assess the different types of physiotherapy treatments separately. |
| Anderson and Seniscal32 | Combining osteopathy treatments with relaxation exercises significantly reduced headache frequency compared to relaxation exercises alone. |
| De Hertogh et al.33 | Headache symptoms improved in both study groups; no significant differences were found between them. The authors suggest conducting studies with greater sample sizes and an observational instead of randomised design. |
| Toro-Velasco et al.34 | A single session of manual therapy immediately decreased heart rate, tension-anxiety, and perceived pain in patients with chronic TTH. Future studies including a greater number of sessions should be designed to investigate the effects and clinical relevance of this type of intervention. |
| Vernon et al.35 | These authors reported clinically relevant and statistically significant benefits in the group receiving chiropractic plus pharmacological treatment in primary care. These promising results should be confirmed by studies with larger sample sizes. |
| Hsieh et al.36 | Therapeutic acupressure is more effective for pain release in patients with chronic headache than muscle relaxants and analgesics. The acupressure technique and correct identification of trigger points are decisive factors for achieving positive outcomes. |
| Ajimsha et al.37 | This study shows evidence that both direct and indirect myofascial release techniques are more effective for TTH than the intervention applied to the control group. |
| Castien et al.38 | Manual therapy was shown to be more effective than short- and long-term standard treatment for reducing the symptoms of chronic TTH. |
| Berggreen et al.39 | MTP massage has a beneficial effect on female patients with chronic TTH. |
| Castien et al.40 | Chronic TTH improves in primary care patients receiving manual therapy. |
According to the data extracted from these articles, patients with TTH receiving manual therapy seem to have more favourable outcomes than patients receiving standard treatment or placebo. However, this finding should be interpreted with caution due to the heterogeneity of the study designs, measurement tools, and treatments. Our study agrees with previous review articles22–25 concluding that spinal manipulation and soft tissue techniques improve symptoms in patients with TTH. However, further research is necessary to confirm the effectiveness of these therapies for TTH.
Of all the assessed articles, we included 14 in our review. We analysed their methodological quality and classified 2 of them28,31 as having low quality. Future randomised controlled trials should be double blind in order to have higher methodological quality. This criterion was only met by 2 of the studies35,36 included in our review. However, double blinding in manual therapy is extremely difficult since finding a placebo similar to manual therapy is nearly impossible given the characteristics of intervention itself.
All the analysed studies reported positive results for manual therapy compared to conventional therapies except for one,33 which reported similar outcomes for all participants. This study included people diagnosed with different types of headache, including TTH, cervicogenic headache, and migraine.33 Each type of headache should be analysed separately since they have different pathophysiological mechanisms that may affect therapy results in different ways. Likewise, chronicity of headache may also play a crucial role. In fact, in the study by Torelli et al.,31 patients with chronic TTH showed a better response to treatment than those with episodic TTH. These authors also found that women responded better to physiotherapy than men; therefore, it would be interesting to analyse the results of manual therapy by sex. Some authors have even suggested that patients with the same type of headache may respond differently to a specific manual therapy depending on their clinical characteristics.42,59
Only 3 articles37,38,40 had an adequate sample size (≥50). The remaining studies had smaller sample sizes and the effect of therapy cannot be extrapolated to the general population due to this bias. In fact, sample sizes in future studies should be calculated based on the results from previous studies. It should be noted that the study with the greatest sample size (n=186)40 randomly assigned participants into 2 groups but then included 104 additional subjects in the manual therapy group since they preferred this type of intervention and refused randomisation. This may have biased results since the patients who preferred manual therapy may have reported more positive results due to their own expectations.
We should also highlight that the reviewed studies included very different measurement tools. Except for the headache diary, which was used in most of the studies,27–32,35,37–40 measurement instruments were quite heterogeneous. Interestingly, neither of the studies analysing reductions in analgesic use30,31,33,38,39 showed positive results. Manual therapy on its own may not be able to reduce TTH symptoms to the point that patients significantly reduce analgesic use; rather, it may be the combination of both that has a beneficial effect.
The number, duration, and frequency of sessions vary greatly; therefore, we cannot draw conclusions regarding these parameters. In fact, this heterogeneity does not allow us to reach a consensus on the optimal frequency and duration of manual therapy sessions. Based on the data provided by the studies included in this review and our own clinical experience, we recommend that patients with TTH take a session lasting 30-45minutes every 7-10 days.
The type of manual therapy intervention also varies across studies. Manual therapy includes techniques for muscle and/or joint treatment; results are therefore difficult to analyse as a whole. Of the studies included in the present review article, 4 applied techniques for joints (joint mobilisations, manipulations, and manual traction),27,29,30,32 5 addressed muscle treatment (acupressure, MTP massage, stretching, and myofascial release),31,34,36,37,39 and the remaining 5 applied mixed treatment consisting of mobilisations, craniocervical exercises, posture control exercises, massage, manipulation, and soft tissue techniques.28,33,35,38,40 The results of the reviewed studies show the benefits of different manual therapy techniques; however, it is difficult to determine which technique or combination of techniques is most effective. In our clinical experience, the combination of both muscle and joint manual therapy techniques is the most beneficial for patients with TTH. Future studies could confirm this.
The control group is another aspect to be analysed. Depending on the study, controls received either standard treatment, no treatment, or a placebo. Vernon et al.35 applied sham chiropractic manipulation to patients on a drop table in order to simulate the sound of joints cracking, which had a placebo effect on patients. Ajimsha et al.37 applied slow soft strokes to controls’ heads, whereas Hsieh et al.36 administered a vitamin B complex for a month (the same treatment period as for the patient group). Again, the heterogeneity of placebo treatments does not allow us to draw conclusions about the effectiveness of manual therapy.
Lastly, the shortest follow-up period was 24hours34 since the purpose of that study was to analyse physiological changes in patients immediately after treatment. The remaining studies included follow-up periods lasting between 4 weeks and 6 months. We cannot draw objective conclusions about the effectiveness of manual therapy due to these disparities. In fact, to implement manual therapy as a treatment for TTH in the Spanish healthcare system we would first need to be able to compose standards regarding the aspects addressed in this review: treatment protocol, session duration and frequency, and medium- and long-term effectiveness.
ConclusionsAccording to our review, patients with TTH receiving manual therapy show more favourable outcomes than patients receiving standard treatment or a placebo. Manual therapy seems to reduce headache frequency and intensity and improve patients’ quality of life but does not lead to a decrease in analgesic use. However, our conclusions must be interpreted with caution due to the heterogeneity of study designs, measurement tools, and treatments.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Lozano López C, Mesa Jiménez J, de la Hoz Aizpurúa JL, Pareja Grande J, Fernández de las Peñas C. Eficacia de la terapia manual en el tratamiento de la cefalea tensional. Una revisión sistemática desde el año 2000 hasta el 2013. Neurología. 2016;31:357–369.