Non-pharmacological treatments help control tension-type headache (TTH); however, evidence about their effectiveness is still limited. This study evaluates the effectiveness of physical therapy based on cervical spine kinesiotherapy and posture correction exercises compared to a programme of relaxation techniques only (Schultz's Autogenic Training, AT).
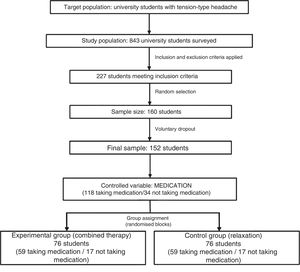
MethodsTTH is very common among university students. We randomly selected 152 university students with a diagnosis of TTH according to the criteria of the International Headache Society. Eighty-four were women (55.3%) and 68 were men (44.7%). Mean age was 20.42±2.36 years. The study design is a randomised controlled trial of a non-pharmacological intervention with a blinded evaluation of response variables. We compared the results of two independent samples: AT was used in one of the groups while the other group received AT plus cervical spine kinesiotherapy and posture correction training. Patients recorded any changes in the parameters of pain (frequency, intensity, and duration) and drug consumption in a headache diary before treatment, at 4 weeks, and at 3 months.
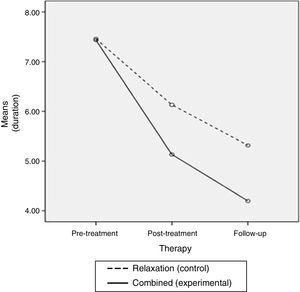
ResultsBoth interventions achieved a decrease in all the parameters of pain; however, decreases in frequency and intensity were more significant in the combined treatment group (P<0.01) (d=0.4).
ConclusionsSuch active, non-invasive therapies as AT and cervical spine kinesiotherapy, and especially the combination of both, effectively reduce TTH by preventing and managing the potential psychophysical causes of this disorder. Future research should aim to assess the long-term effects of these interventions.
Los tratamientos no farmacológicos consiguen controlar la cefalea tensional, sin embargo, la evidencia es todavía limitada. Esta investigación estudia la eficacia de una intervención fisioterápica, basada en cinesiterapia cervical y pautas de higiene postural, que pretende mejorar los resultados obtenidos únicamente con técnicas de relajación (Entrenamiento Autógeno de Schultz [EA]).
MétodosSe seleccionó a 152 estudiantes universitarios (sector poblacional entre quienes esta patología es muy frecuente), 84 mujeres (55,3%) y 68 hombres (44,7%), con edad media de 20,42 años (DT = 2,36), diagnosticados de cefalea tensional, según criterios de la International Headache Society. Se diseñó un ensayo clínico, no farmacológico, controlado y aleatorizado, con evaluación ciega de las variables respuesta. Se compararon los resultados de 2 muestras paralelas e independientes, aplicando a una el EA y a la otra la combinación de este con un programa de cinesiterapia cervical y educación postural. Se cuantificaron la mejoría en los parámetros dolorosos (frecuencia, intensidad y duración) y la reducción del consumo de fármacos, en diarios de cefaleas, antes de los tratamientos y después, a las 4 semanas y a los 3 meses.
ResultadosLos 2 grupos de intervención evolucionaron positivamente, consiguiéndose una reducción más significativa en la frecuencia e intensidad de las cefaleas con el tratamiento combinado (p < 0,01) (d = 0,4).
ConclusionesLas terapias activas, no invasivas, como el EA y la cinesiterapia cervical, y especialmente la combinación de ambos, consiguen reducir la cefalea tensional, al prevenir y controlar las posibles causas psicofísicas de este trastorno. Como futuras líneas de investigación, sería interesante evaluar el mantenimiento de los beneficios a largo plazo.
Headache is a very frequent and disabling condition and one of the leading reasons for outpatient and neurological consultation; it represents a significant healthcare problem worldwide.1–3
The most widely used criteria for classifying types of headache are those established by the International Headache Society (IHS), included in the International Classification of Headache Disorders-II (ICHD-II, 2004).4 At the time of drafting this study, the third edition of this classification (ICHD-III) was in the process of being published and use of its beta version (ICHD-III beta),5 published in 2013, was already recommended.
Tension-type headache (TTH) is the most frequent type of headache. According to the 2010 systematic review by Stovner and Andree,6 prevalence of TTH in Europe amounts to 62.2%. Incidence reaches approximately 14.2 per 1000 person-years.7 TTH affects 70% of the Spanish population.8 In recent years, TTH has become a significant problem among young people, who are increasingly developing headache.7,9
The aetiology and pathophysiology of TTH are currently still being investigated. Among its trigger factors, we should emphasise psychosocial stress and/or muscular overstrain caused by non-physiological posture. Regarding muscular factors, it has been demonstrated that the most consistent symptom is increased pain sensitivity linked to increased head and neck muscle tension. Such authors as Fernández-de-las-Peñas et al.10,11 or Bendtsen et al.12,13 have stated that referred pain at active myofascial trigger points in the head and neck cause the release of several algogenic substances which sensitise peripheral nociceptors, originating radiating pain in the head. Some factors promote and stimulate the activity of myofascial trigger points; these include sustained inadequate postures, which may favour dysfunction of the neck muscles, reduce neck mobility, and overload the vertebral segments. Central pain control mechanisms may also be altered in TTH, leading to a decreased threshold for pain, which may be linked to the condition becoming chronic.14
The most frequently used type of treatment is drug therapy. Conservative treatments are also used, including relaxation techniques, biofeedback, specific physiotherapy techniques (electrotherapy, manual therapy, exercise programmes, and posture correction guidelines), and acupuncture. However, these therapies are still little-known among patients and even healthcare professionals.15
Regarding psychological treatments, some studies have obtained positive results in controlling TTH with autogenic training (AT), a relaxation technique based on simple exercises designed to elicit physiological changes and voluntary control of the autonomic nervous system.16 AT enables control of the overall level of activation, closely related to the appearance of this type of headache, and can reduce the intensity and frequency of pain in the short and medium term, as well as improving patients’ subjective well-being and quality of life.17–21
In terms of physical therapy, some techniques improving cervical neuromuscular control have been successful in treating TTH; however, these findings are inconclusive due to methodological issues in the majority of these studies.22,23 Furthermore, although these conservative treatments seem to have beneficial effects, the precise physiopathology of TTH is still unknown; therefore, some authors point to a controversy regarding the degree of involvement of musculoskeletal factors in TTH and the effectiveness of physiotherapy for the condition. This is reflected in some recent meta-analyses and reviews.24,25
Furthermore, most previous studies using non-invasive therapies combined these with manual therapy; however, some studies do demonstrate the effects of active psycho-physical training in controlling TTH without the patient constantly depending on specialist care.
Therefore, we aimed to determine whether physiotherapy, based on a physical training programme and postural hygiene guidelines (aimed at reprogramming correct head, neck, and shoulder muscle activity), may enhance the positive results of other such methods as AT in reducing TTH in university students.
The general aim was to compare the efficacy of a training programme and posture correction guidelines combined with AT to the effects of AT exclusively. More specifically, we compared the results of both intervention groups in terms of headache intensity, frequency, and duration, and drug use in the short (after 4 weeks of treatment) and medium term (3 months after treatment completion).
Subjects, material, and methodsDesignWe performed a randomised, controlled, non-pharmacological clinical trial with masked assessment of the response variables. We compared the results of 2 parallel and independent samples. One of the groups underwent AT and the other group a combination of AT and neck physical therapy and posture training.
ParticipantsWe selected university students as this population presents a high prevalence of TTH, probably due to poor postural habits and stress factors, and because little research has addressed this sector to date.26–28 Specifically, the sample included students from the School of Education of the Universidad Complutense in Madrid (2010-2011 academic year) and diagnosed with TTH by their family doctor or neurologist. We included both men and women, aged between 18 and 25 years.
Many headache specialists report that some cases of mild migraine may be misdiagnosed as TTH in everyday clinical practice, especially in young women, among whom the prevalence of migraine is high.29 For this reason, before the interventions and despite students having a previous diagnosis of TTH, one of our researchers (specialised in headache) conducted an exhaustive selection of participants, using a survey to confirm that they strictly met the criteria established by the IHS for frequent episodic or chronic TTH. We used these criteria since they are clearly defined and universally accepted. In our study, we used the ICHD-II,4 since ICHD-III beta5 had not been published at the time of the study.
We excluded cases presenting other types of headache, excessive state-trait anxiety (percentile≥85 on the State-Trait Anxiety Inventory30) to obtain a more homogeneous psychological profile of participants,31,32 and subjects who had received treatment for TTH based on physical exercise or relaxation techniques in the preceding 6 months.
Sample size was calculated to identify a minimum difference of 2 units (2 days) in the main variable (frequency of headache), as recommended in the literature.31,32 We used the t test for independent samples with a significance level of 5%, statistical power of 80%, and assuming a shared standard deviation of 4.28 units.31,32 The number of patients was the same in both groups and the rate of participants lost to follow-up was estimated at 10%. Considering the data obtained and using the GRANMO software (version 5.2), we calculated a sample size of 160 subjects (80 in each group).
The study was approved by the Research Ethics Committee at the School of Nursing, Physiotherapy, and Podology, Universidad Complutense de Madrid (Code F [EFP]-003/2010), in accordance with the regulations regarding clinical trials, as stipulated by Royal Decree 223/2004, of 6 February. The study is registered on www.clinicaltrials.gov, with identification number NCT02264340.
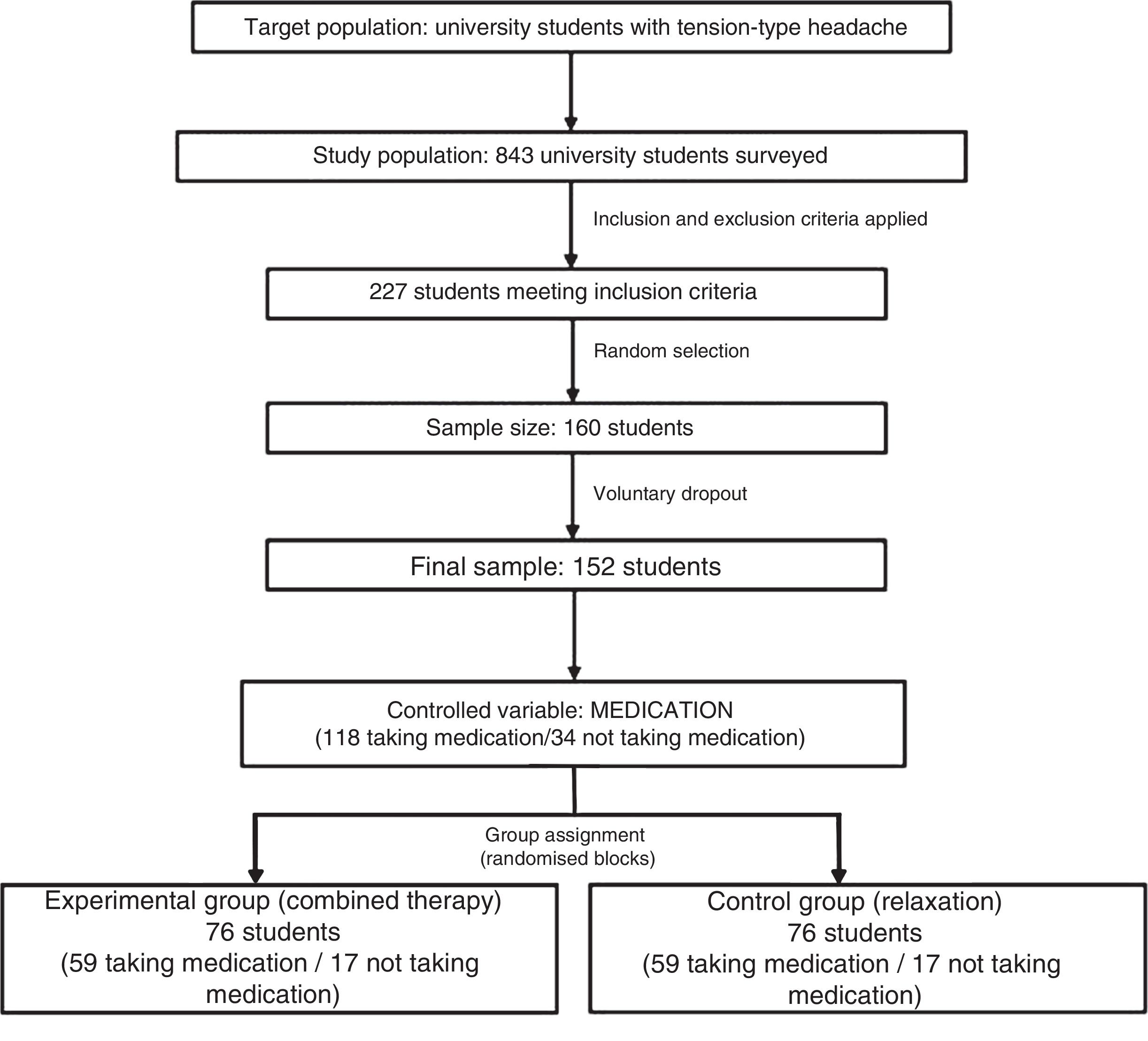
The survey was distributed to 843 students. Of the subjects fulfilling selection criteria, we randomly selected 160, using a random number table (obtained with the Epidat software, version 3.1). Eight subjects declined to participate in the study, and 152 completed the study. In an initial interview, students were informed of the objectives and characteristics of the study and provided with an informed consent form. Data confidentiality was ensured under the terms of Spanish Organic Law 15/1999, of 13 December, regarding personal data protection. Subsequently, all participants were assigned in a ratio of 1:1 to one of the 2 intervention groups, using randomised blocks to balance the number of students taking medications to control headache in each group. Thus, each group included 59 subjects who were taking medication and 17 who were not. This distribution enabled us to control for the possible effect of the concomitant drug treatment (Fig. 1).
InterventionsSubjects in the control group were trained to practise a relaxation technique, the basic exercises of AT, which have been shown to be effective in treating these pathologies.16–21 These exercises consist in gradually inducing progressive feelings of heaviness and warmth throughout the body, regulating cardiac and respiratory rate, and focus on cooling the forehead.
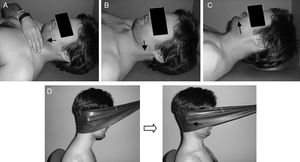
Students in the experimental group learnt the same relaxation technique, in addition to a series of exercises for the head, neck, and shoulders, and received some guidelines on ergonomics and postural hygiene. The referenced literature shows the importance of retraining the neck flexor-extensor synergy in patients with TTH. However, as we did not find any specific exercise protocols, we opted for a combination of those exercises supported by higher levels of scientific evidence, to assess their outcomes.33–39 Specifically, every exercise session consisted of:
- 1.
Initial warm-up exercises with slight movements of the neck and shoulders.
- 2.
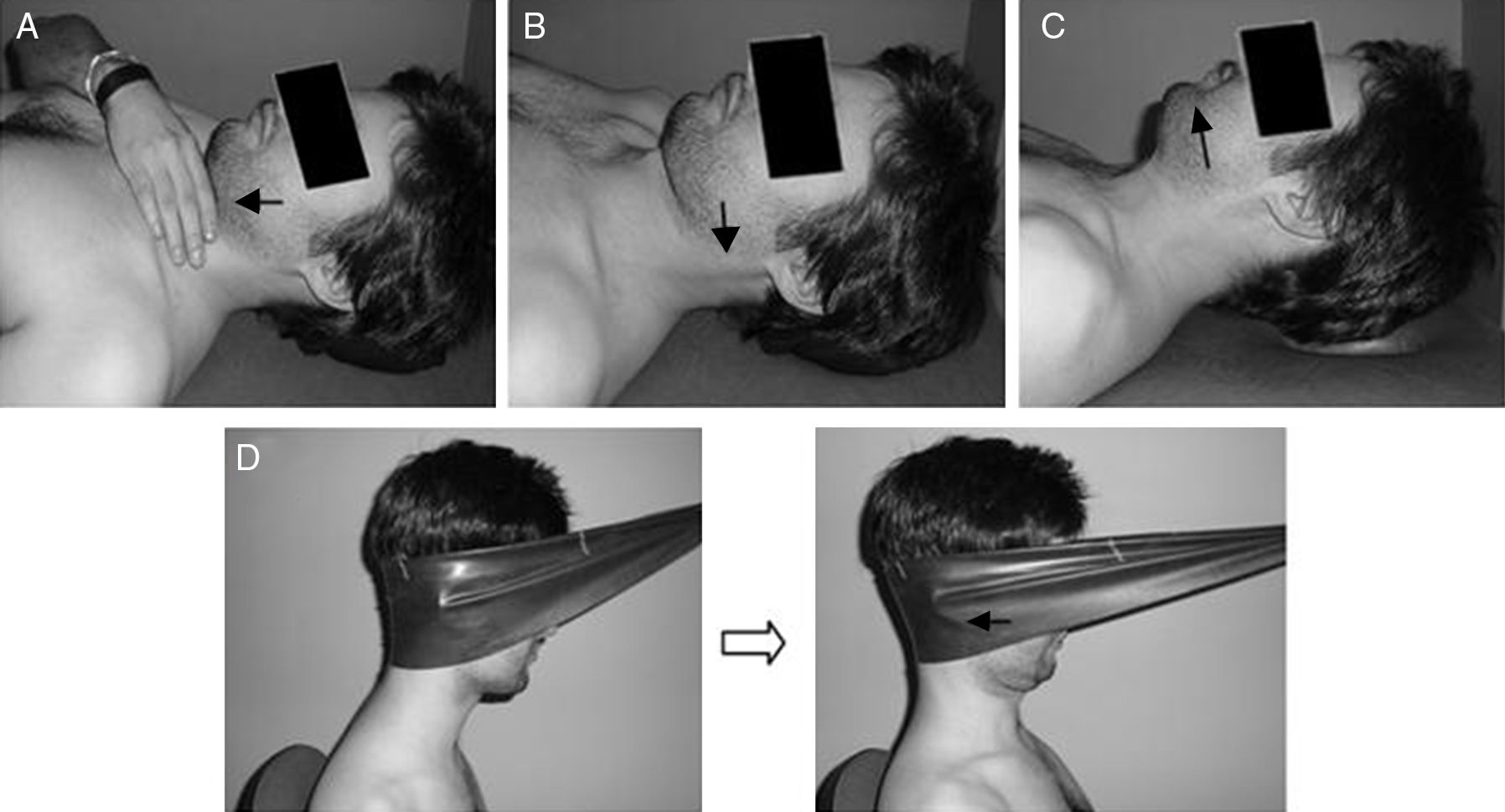
Specific exercises for reprogramming the neck flexor-extensor synergy, combining training of the deep craniocervical flexor muscles with extension of the middle or lower cervical segment; these exercises were subsequently used in more functional movements of dynamic neck retraction against resistance of an extra-heavy latex resistance band (Thera-Band, blue) (Fig. 2).
- 3.
Stretching of hypertonic muscles (trapezius, sternocleidomastoid, scalene, suboccipital, and pectoral muscles).
Participants were also taught postural hygiene guidelines while seating, standing up, and lying down, as well as other advice on ergonomics at home and while studying.
Both interventions were initially directed by 2 therapists, each of whom specialised in one type of treatment (psychological or physical). Measurements were recorded by a different researcher. The therapists provided both oral and written instructions in a single session for the participants to perform the exercises in their own homes. Participants in the control group (monotherapy) were told to perform the relaxation exercises once daily for 4 weeks; members of the experimental group (combined treatment) were instructed to perform one session of relaxation exercises and another of physiotherapy daily for 4 weeks, always following the postural correction guidelines. Weekly follow-up sessions were held with the corresponding therapist to maximise the benefits of the interventions. During the 3 months following the post-treatment evaluation, the frequency of home sessions was reduced to 3 times per week in order to maintain the results.
Evaluation procedureThe benefits of the therapy were quantified according to the improvements in the different variables, assessed with reliable and valid tools. The main response variable was the frequency of headache; the remaining pain parameters (intensity and duration) and the reduction in drug consumption were considered secondary.
Participants were provided with a headache diary to record the study variables at home for periods of 4 weeks, at 3 different moments: before therapy (pre-treatment evaluation) to establish a baseline, and after therapy in the short-term (post-treatment evaluation) and the medium-term (follow-up evaluation).31,32,40
Participants were instructed to record the data on the diary at the end of the day, establishing a record of the clinical history of pain, including frequency (days/4 weeks), duration (hours per day), headache intensity (visual analogue scale [VAS]: 0-10),41 and analgesic use (days/4 weeks).
In comparison with other pain scales, the VAS is more sensitive to changes in pain intensity, and is the most widely used scale in experimental studies.42–44 Kelly45 established that the minimum clinically significant difference for the VAS was 10mm to 15mm.
Statistical analysisThe results of the study were recorded in a database using the SPSS v.19.0 software, enabling subsequent statistical analysis.
We first conducted a descriptive analysis, using measures of central tendency (means) and dispersion (standard deviations) for quantitative variables, and frequency distributions for qualitative variables.
We compared the results of quantitative variables using a repeated measures analysis of variance (ANOVA) to determine intragroup differences, and the t test for independent samples to determine intergroup differences.
We used the Chi-square test to compare qualitative variables before therapy.
Bilateral hypothesis tests were applied with an alpha level of significance of 0.05 (95% confidence interval) and a statistical power of 80%.
ResultsAll students (N=152, 76 in the experimental group and 76 in the control group) completed the therapy. No participants were lost to follow-up.
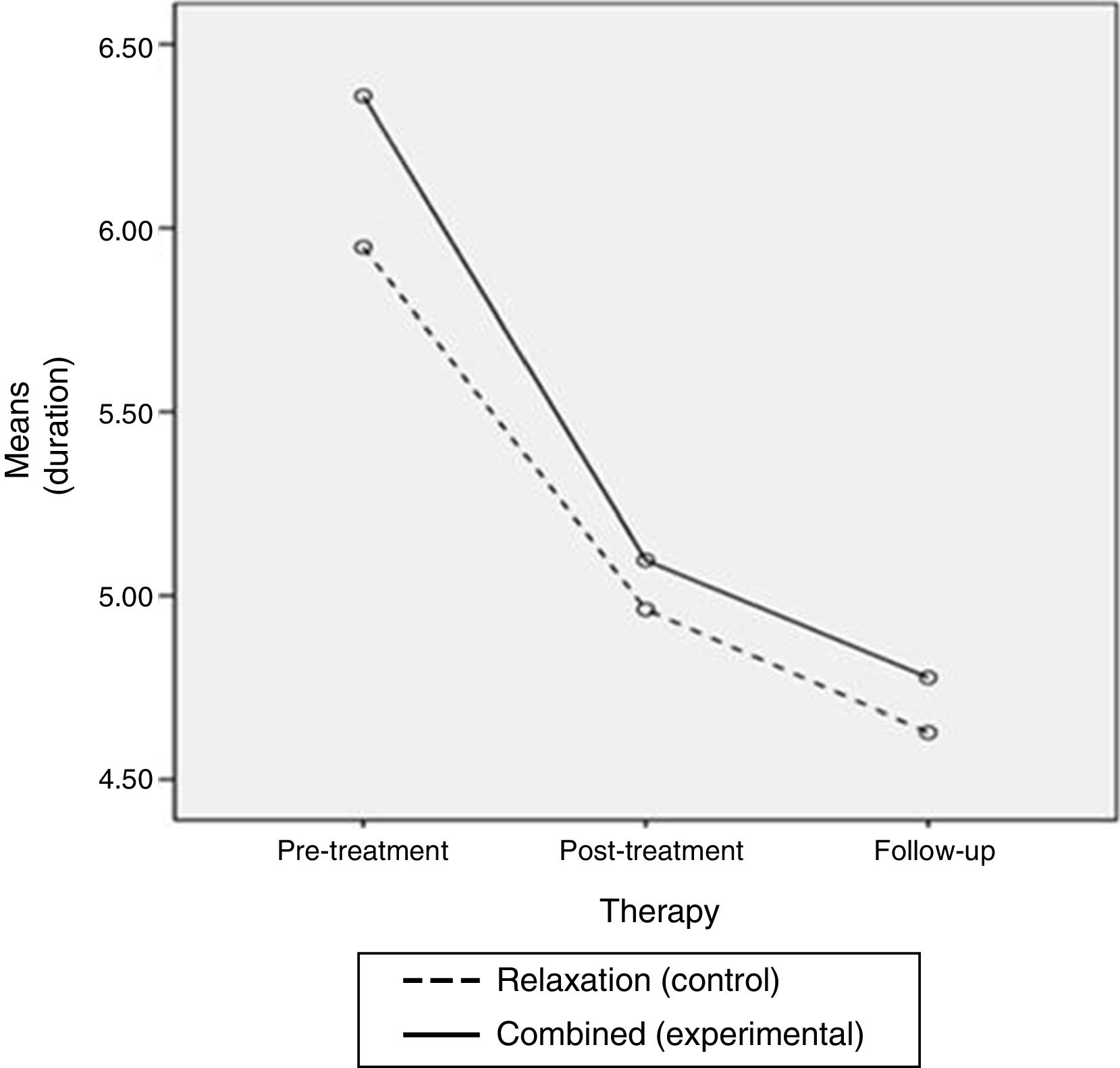
Baseline characteristics for both groups were similar (Table 1).
Comparison of intervention groups (baseline).
| Control group (n=76) | Experimental group (n=76) | t/χ2 | P-value | |
|---|---|---|---|---|
| Age (years) | 20.62 (2.21) | 20.23 (2.50) | 0.994 | 0.322 |
| Sex | 3.832 | 0.052 | ||
| Women | 34 | 50 | ||
| Men | 42 | 26 | ||
| Type of headache | 1.052 | 0.305 | ||
| ETTH | 53 | 47 | ||
| CTTH | 23 | 29 | ||
| Frequency (days in 4 weeks) | 12.71 (4.07) | 12.96 (4.75) | −0.348 | 0.728 |
| Intensity (VAS: 0-10) | 5.57 (1.32) | 5.82 (1.26) | −1.182 | 0.239 |
| Duration (h/day) | 5.94 (3.00) | 6.35 (3.04) | −0.837 | 0.549 |
| Analgesic use (days in 4 weeks) | 7.46 (5.01) | 7.43 (5.27) | 0.032 | 0.975 |
Data are expressed as frequencies or means (SD).
Comparisons were performed using the t test for independent samples and the Chi-square test.
CTTH: chronic tension-type headache; ETTH: episodic tension-type headache; VAS: visual analogue scale.
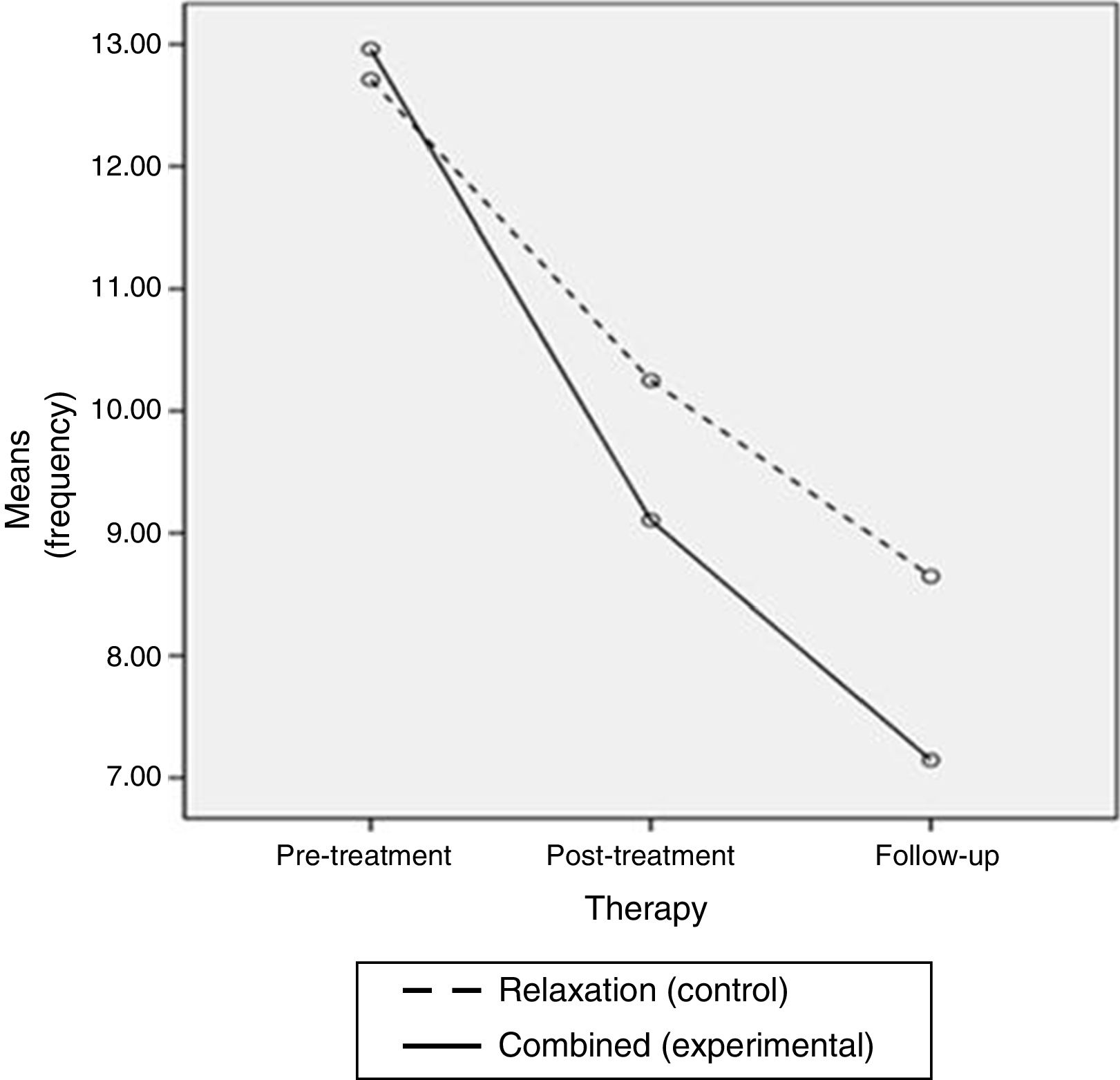
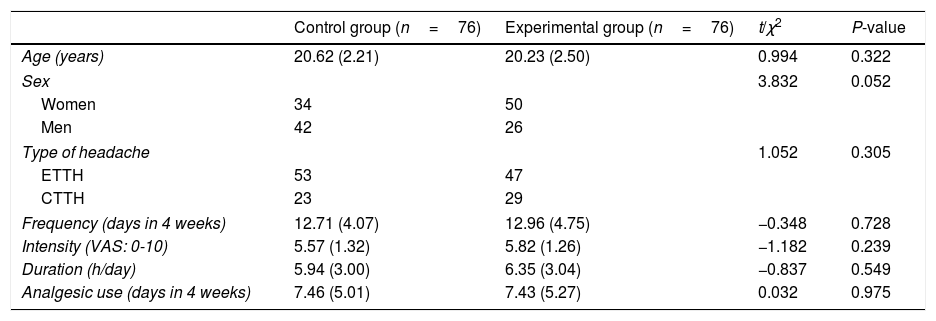
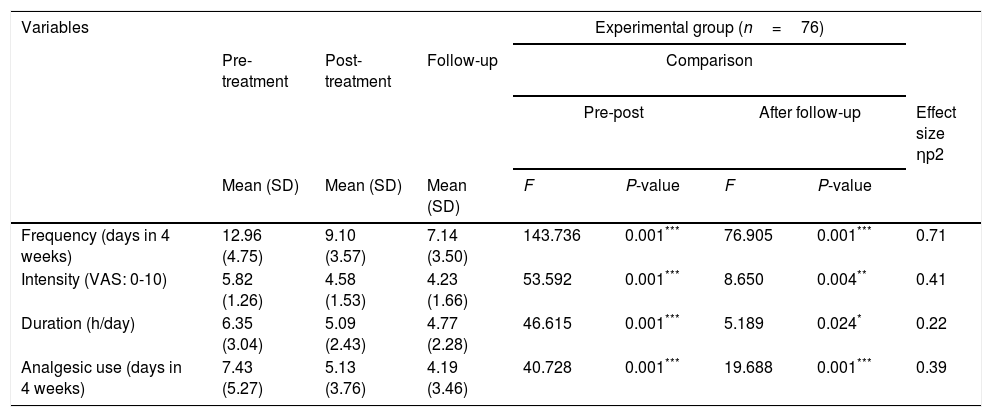
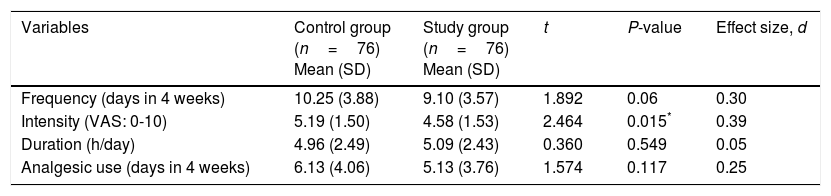
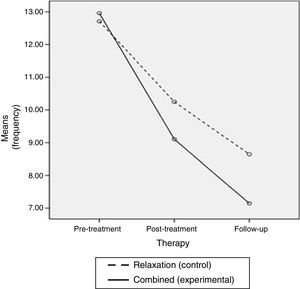
Four weeks after the intervention, post-treatment measurements showed a generally decreased frequency of headaches. Both groups showed statistically significant differences (P<.001) between the pre-treatment measurement and the evaluation at the end of therapy; this decrease was more pronounced in the experimental group, although the intergroup difference in the post-treatment measurement was not statistically significant (P=0.06) (d=0.30) (Tables 2–5 and Fig. 3).
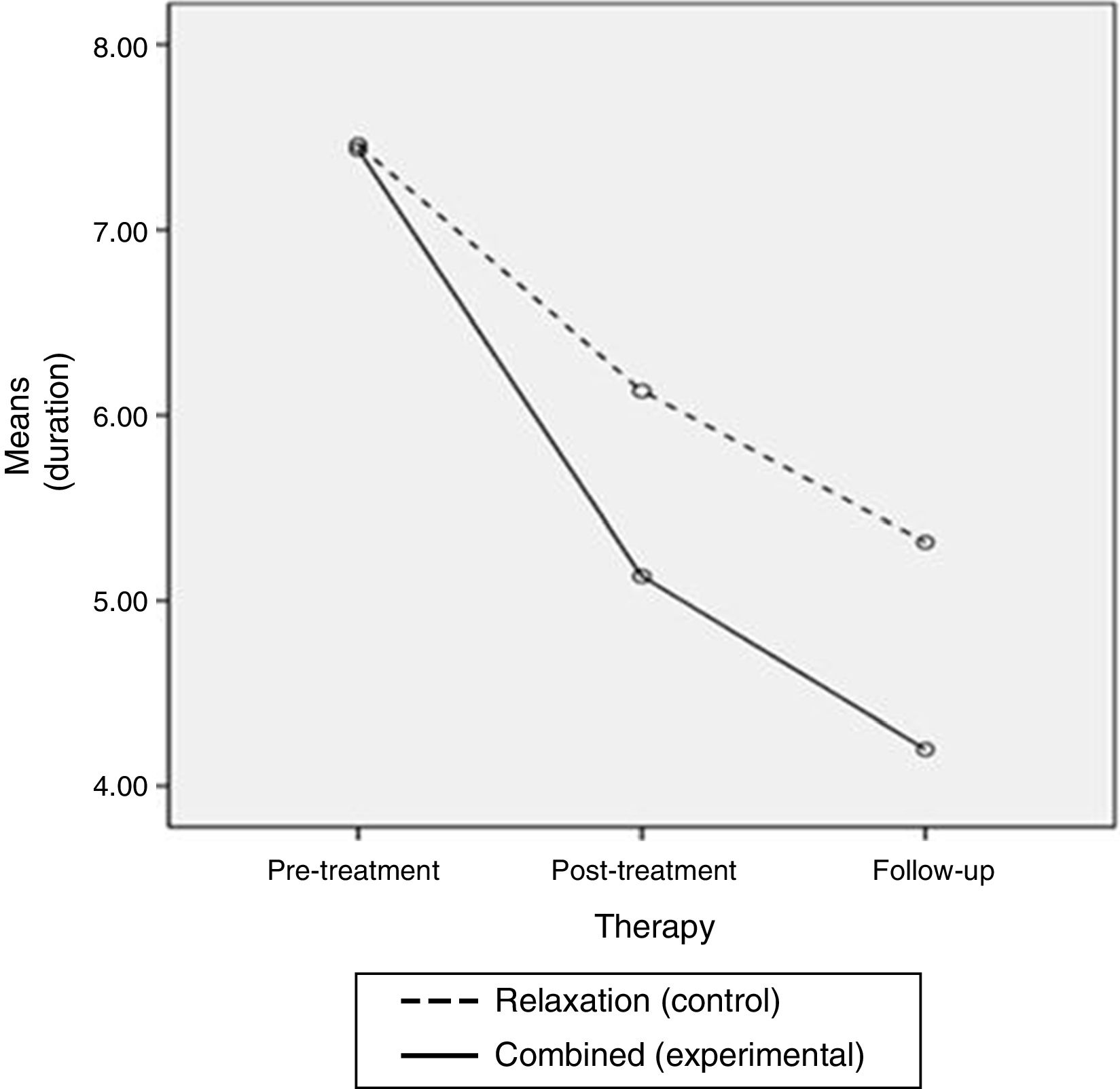
Progression of the control group (relaxation techniques). Intragroup differences.
| Variables | Control group (n=76) | |||||||
|---|---|---|---|---|---|---|---|---|
| Pre-treatment | Post-treatment | Follow-up | Comparison | |||||
| Pre-post | After follow-up | Effect size ηp2 | ||||||
| Mean (SD) | Mean (SD) | Mean (SD) | F | P-value | F | P-value | ||
| Frequency (days in 4 weeks) | 12.71 (4.07) | 10.25 (3.88) | 8.64 (3.59) | 61.746 | 0.001*** | 26.410 | 0.001*** | 0.50 |
| Intensity (VAS: 0-10) | 5.57 (1.32) | 5.19 (1.50) | 4.96 (1.59) | 6.226 | 0.015* | 3.619 | 0.061 | 0.11 |
| Duration (h/day) | 5.94 (3.00) | 4.96 (2.49) | 4.62 (2.50) | 46.615 | 0.001*** | 5.189 | 0.024* | 0.22 |
| Analgesic use (days in 4 weeks) | 7.46 (5.01) | 6.13 (4.06) | 5.31 (3.77) | 21.943 | 0.001*** | 13.291 | 0.001*** | 0.28 |
ANOVA: one-factor repeated measures analysis of variance.
SD: standard deviation; VAS: visual analogue scale.
Progression of the experimental group (combined therapy). Intragroup differences.
| Variables | Experimental group (n=76) | |||||||
|---|---|---|---|---|---|---|---|---|
| Pre-treatment | Post-treatment | Follow-up | Comparison | |||||
| Pre-post | After follow-up | Effect size ηp2 | ||||||
| Mean (SD) | Mean (SD) | Mean (SD) | F | P-value | F | P-value | ||
| Frequency (days in 4 weeks) | 12.96 (4.75) | 9.10 (3.57) | 7.14 (3.50) | 143.736 | 0.001*** | 76.905 | 0.001*** | 0.71 |
| Intensity (VAS: 0-10) | 5.82 (1.26) | 4.58 (1.53) | 4.23 (1.66) | 53.592 | 0.001*** | 8.650 | 0.004** | 0.41 |
| Duration (h/day) | 6.35 (3.04) | 5.09 (2.43) | 4.77 (2.28) | 46.615 | 0.001*** | 5.189 | 0.024* | 0.22 |
| Analgesic use (days in 4 weeks) | 7.43 (5.27) | 5.13 (3.76) | 4.19 (3.46) | 40.728 | 0.001*** | 19.688 | 0.001*** | 0.39 |
ANOVA: one-factor repeated measures analysis of variance.
SD: standard deviation; VAS: visual analogue scale.
Intergroup post-treatment differences.
| Variables | Control group (n=76) Mean (SD) | Study group (n=76) Mean (SD) | t | P-value | Effect size, d |
|---|---|---|---|---|---|
| Frequency (days in 4 weeks) | 10.25 (3.88) | 9.10 (3.57) | 1.892 | 0.06 | 0.30 |
| Intensity (VAS: 0-10) | 5.19 (1.50) | 4.58 (1.53) | 2.464 | 0.015* | 0.39 |
| Duration (h/day) | 4.96 (2.49) | 5.09 (2.43) | 0.360 | 0.549 | 0.05 |
| Analgesic use (days in 4 weeks) | 6.13 (4.06) | 5.13 (3.76) | 1.574 | 0.117 | 0.25 |
t test for independent samples.
SD: standard deviation; VAS: visual analogue scale.
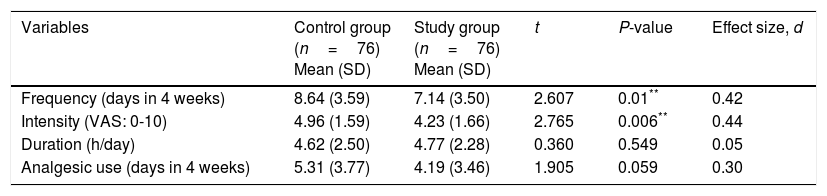
Intergroup differences during follow-up.
| Variables | Control group (n=76) Mean (SD) | Study group (n=76) Mean (SD) | t | P-value | Effect size, d |
|---|---|---|---|---|---|
| Frequency (days in 4 weeks) | 8.64 (3.59) | 7.14 (3.50) | 2.607 | 0.01** | 0.42 |
| Intensity (VAS: 0-10) | 4.96 (1.59) | 4.23 (1.66) | 2.765 | 0.006** | 0.44 |
| Duration (h/day) | 4.62 (2.50) | 4.77 (2.28) | 0.360 | 0.549 | 0.05 |
| Analgesic use (days in 4 weeks) | 5.31 (3.77) | 4.19 (3.46) | 1.905 | 0.059 | 0.30 |
t test for independent samples.
SD: standard deviation; VAS: visual analogue scale.
Frequency of headache subsequently continued to decrease over the follow-up period, as shown by the measurements obtained 3 months after the interventions finished. Follow-up results were significantly lower than those obtained in the pre-treatment and post-treatment evaluations in both groups (P<.001) (ηp2=0.50 in the control group vs 0.71 in the experimental group). As in the post-treatment measurement, the decrease was greater in the experimental group; in this case, the intergroup difference was statistically significant (P=.01) (d=0.42) (Tables 2–5 and Fig. 3).
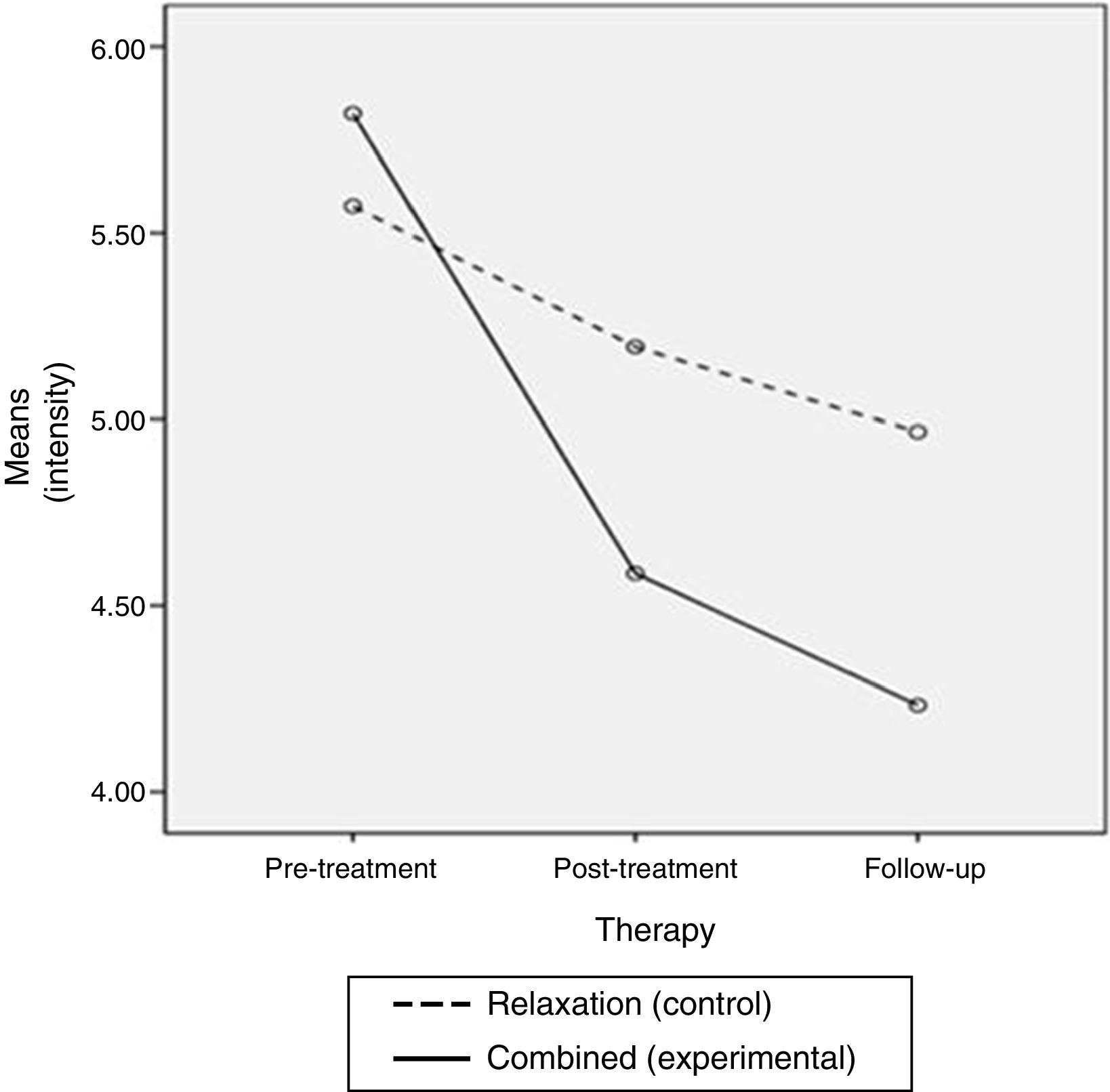
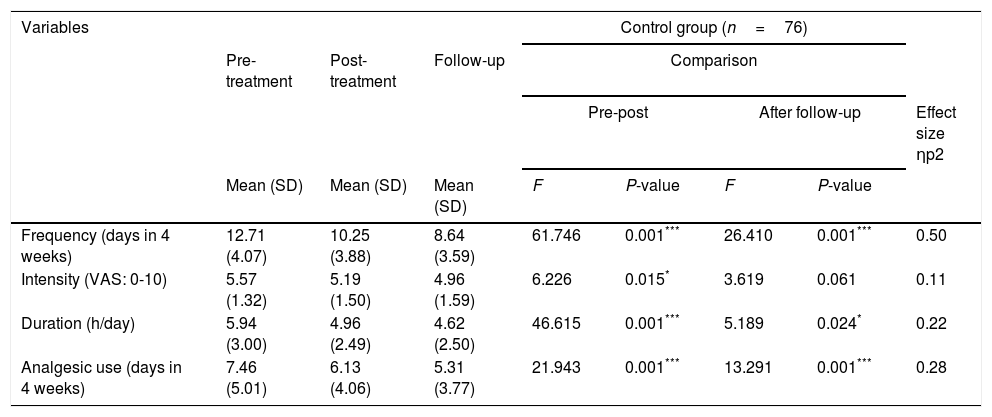
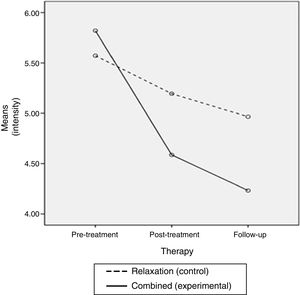
Regarding pain intensity, intragroup comparisons after therapy showed that the decrease was statistically significant in both groups: P=.015 in subjects treated with relaxation only and P<.001 in those receiving combined therapy. Regarding intergroup differences in the post-treatment evaluation, we should highlight that a more significant improvement was observed in the experimental group (P=.015) (d=0.39) (Tables 2–5 and Fig. 4).
The follow-up measurement shows a greater decrease in the frequency of headaches than that observed in the post-treatment evaluation. This decrease was statistically significant in the experimental group (P=.004) (ηp2=0.41) but not in the control group (P=.061) (ηp2=0.41). Intergroup differences, as in the second measurement, were also statistically significant (P=.006) (d=0.44), with the combined therapy group showing better results (Tables 2–5 and Fig. 4).
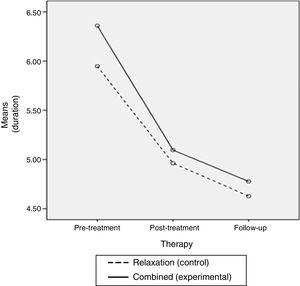
Regarding headache duration, the overall intragroup differences were statistically significant between the pre- and post-treatment measurements (P<.001), as well as between post-treatment and follow-up (P=.024) (ηp2=0.22); however, no overall significant differences were observed between interventions (P=.549) (d=0.05) (Tables 2–5 and Fig. 5).
A decrease in analgesic consumption was also achieved. These intragroup differences were statistically significant in both intervention groups in all evaluations (P<.001) (ηp2=0.28 in the control group vs 0.39 in the experimental group); however, differences between interventions were not statistically significant in the post-treatment evaluation (P=.117) (d=0.25) or at 3 months (P=.059) (d=0.30) (Tables 2–5 and Fig. 6).
DiscussionIntragroup and intergroup comparisons revealed that both groups obtained good short- and medium-term results in many of the variables assessed. Nevertheless, the experimental group displayed more significant improvements in headache frequency and intensity (P<.01). Therefore, our initial hypothesis is confirmed for these variables.
After the therapies were administered, the final measurements showed that the frequency of headache was decreased by a 32% in the control group (4.07 days/months) and by 45% in the experimental group (5.82 days/month). Intensity was decreased by 0.61 points on the VAS in the control group, and 1.59 in the experimental group; the latter decrease is clinically significant.41,45 Duration of pain was reduced by 22% (1.32h/day) with relaxation techniques only and 25% (1.58h/day) with combined treatment. Drug consumption also decreased: 29% (2.15 days/month) in the control group, and 44% (3.24 days/month) in the experimental group.
We have not found clear references in the literature to what percentage of reduction in headache frequency or duration is considered clinically relevant. Some studies report that a total reduction of 50% is a very positive result; however, this value is arbitrary.31,32
Our study shows significant differences in the main parameters analysed, with combined therapy (exercise programme, postural hygiene, and AT) yielding better results than training in relaxation techniques only.
Regarding frequency of headache, this intergroup difference was statistically significant and clinically relevant (moderate effect size) in the evaluation at 3 months. In our opinion, this may be due to the fact that the effects of exercise and postural correction, which aim to re-balance the affected neck muscles, could be more easily observed in the medium to long term.
Regarding intensity, an interesting finding was the statistically significant and clinically relevant improvement (moderate effect size) observed in the experimental group, in both the short and the medium term. The decrease in excessive tension in the superficial neck muscles, achieved with combined treatment especially, may influence the reduction in pericranial hypersensitivity. In line with other authors, such as Carlsson et al.,46 we believe that this improved sensitivity would in turn be related to the decrease in headache intensity.
Headache duration and analgesic consumption decreased similarly after both interventions; no significant differences were observed between the 2 groups.
Comparing our results with those of previous studies,33,47,48 we may corroborate that such conservative, non-invasive treatments as physiotherapy (exercises and postural correction guidelines) and/or relaxation techniques are effective in reducing pain parameters in TTH. Those studies also found significant improvements in reducing pain parameters in TTH; however, most of these included manual therapy as one of the interventions. Our study shows that a significant reduction in these parameters may be achieved by using only group treatments, which teach patients how to identify and control the possible causes and factors that maintain their headaches. This way, participants do not need to depend continuously on manual therapy performed by qualified staff, such as massage therapy or joint mobilisation therapy.
Furthermore, we wish to underscore the relatively short duration of our study (4 weeks), in comparison with other studies, where a longer intervention period was needed before positive results were observed.
Soderberg et al.19 report one of the few studies using exercise or relaxation as the only therapy, not combined with manual therapy. The authors conclude that, considering that TTH has a multifactorial origin, further clinical trials demonstrating the efficacy of combined therapies (physical and psychological) are necessary, as they will probably obtain better results. Our study reveals, as reported by Soderberg et al., that combined therapy achieves even better results that those seen for treatment with relaxation techniques exclusively.
We may consider that the positive results obtained in both intervention groups, and especially in the experimental group, are due to the combined approach addressing the psychological and physical alterations involved in the aetiology of TTH. On the one hand, exercises and postural hygiene guidelines decrease peripheral muscle tension in the head and neck; on the other, relaxation techniques also reduce muscle tension and excessive overall level of activation, improving central pain control mechanisms.
However, there may be individual differences in the success of these therapies. Some authors have proposed certain clinical characteristics which, when present in patients with TTH, may improve the benefits of physical therapy.49 The majority of participants in our study met the criteria described, which may also explain the results. Work into this line of research is ongoing; new data may, therefore, come to light.
Regarding the limitations of the study, we should mention that blinding of participants was not possible due to the characteristics of the intervention. Also, in the case of such active treatments as those used in our study, participants’ motivation and commitment is important. Although guaranteeing the constant performance of the exercises at home is difficult, we conducted periodic follow-up sessions to maximise the benefits of the interventions.
Among the possible future lines of research, it would be interesting to assess to what extent the benefits are maintained over a longer period, such as 6 months or one year after therapy.
FundingThis study has received no public or private funding.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Álvarez-Melcón AC, Valero-Alcaide R, Atín-Arratibel MA, Melcón-Álvarez A, Beneit-Montesinos JV. Efectos de entrenamiento físico específico y técnicas de relajación sobre los parámetros dolorosos de la cefalea tensional en estudiantes universitarios: un ensayo clínico controlado y aleatorizado. Neurología. 2018;33:233–243.