We present the case of a 4-year-old girl who, after suffering a severe head trauma in a domestic accident, presented signs compatible with right mesencephalic paramedian arterial involvement, as well as loss of function of the left lacrimal gland due to fracture of the left petrous bone; both are rare complications of head trauma.
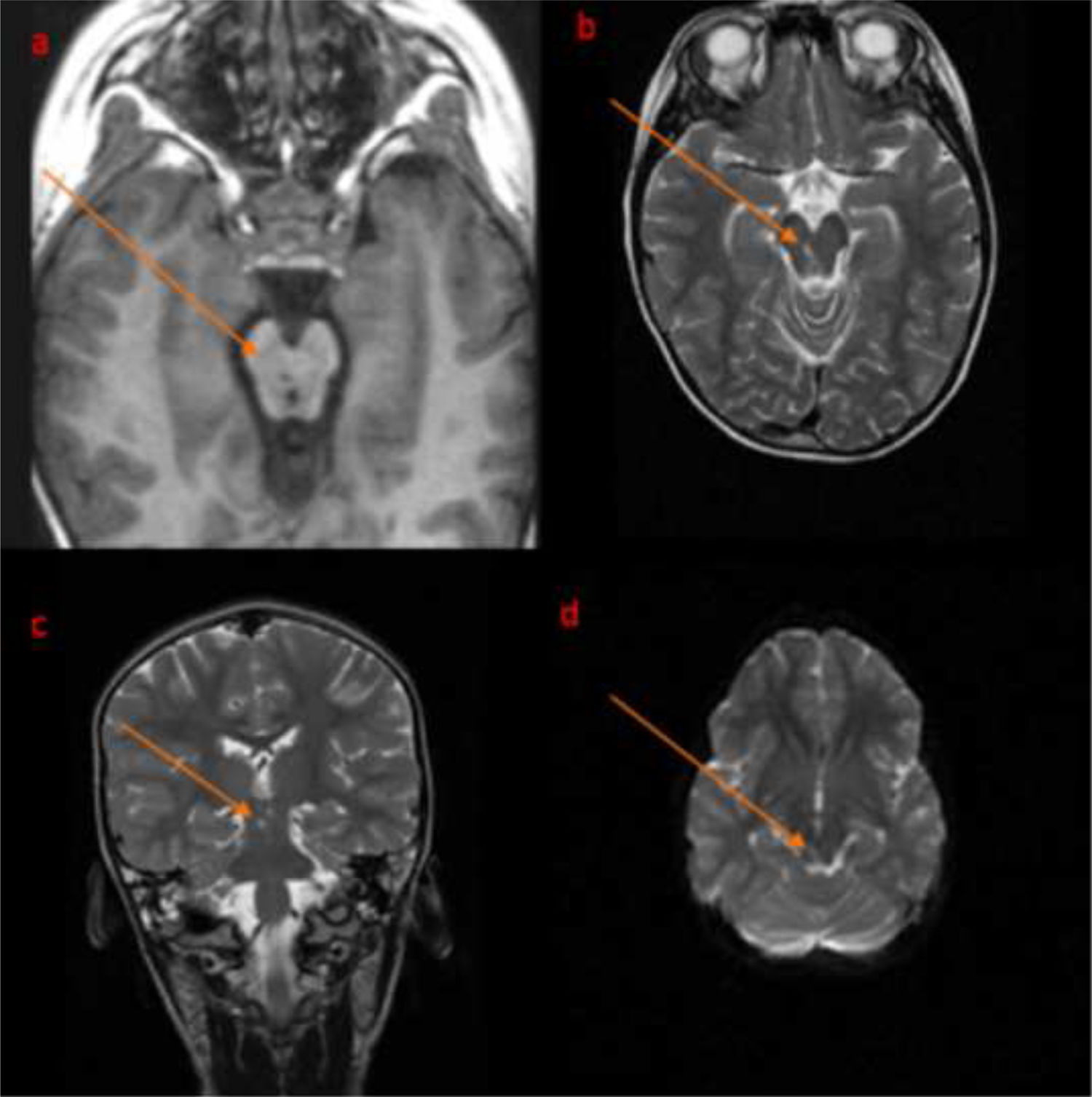
The patient was struck on the head by a falling television. Upon arrival at hospital, she presented a Glasgow Coma Scale (GCS) score of 7 and was intubated and admitted to the paediatric intensive care unit (PICU). A brain CT scan revealed a subarachnoid haemorrhage in the basal cisterns and fracture of the left occipital and temporal bones and both petrous bones; pneumocephalus was also observed. She was extubated 12 hours after admission to the paediatric intensive care unit with an initial GCS score of 11 and progressively improved with good oral tolerance on the third day and GCS score of 15 on the fifth; the patient was then transferred to an admission ward. Ptosis and impaired adduction of the right eye were observed, as well as absence of tearing in the left eye, difficulty maintaining a seated position, Romberg sign with a tendency to fall to the left, and inability to walk. An orbital CT scan found that the third cranial nerve was not impaired due to entrapment. A brain MRI scan showed T2-weighted hyperintensity, abnormal diffusion restriction, and T1-weighted hypointensity at the level of the dorsal region of the right mensencephalic tegmentum (Fig. 1). The patient progressively improved and was discharged 22 days after admission with only a small increase in the base of support, and persistent lack of tearing; ptosis and impaired adduction of the right eye resolved.
The lack of tearing in the left eye (contralateral to the midbrain infarction) is explained by the fracture of the left petrous bone. The greater petrosal nerve, which innervates the lacrimal gland through parasympathetic fibres, exits the temporal bone through the Fallopian hiatus, joining the deep petrosal nerve to form the vidian nerve at the pterygopalatine ganglion, projecting postganglonic fibres to the lacrimal gland. Injury to the petrous bone may damage the greater petrosal nerve along its trajectory through the canal passing through the bone; this would explain the loss of function of the lacrimal gland ipsilateral to the injury.1
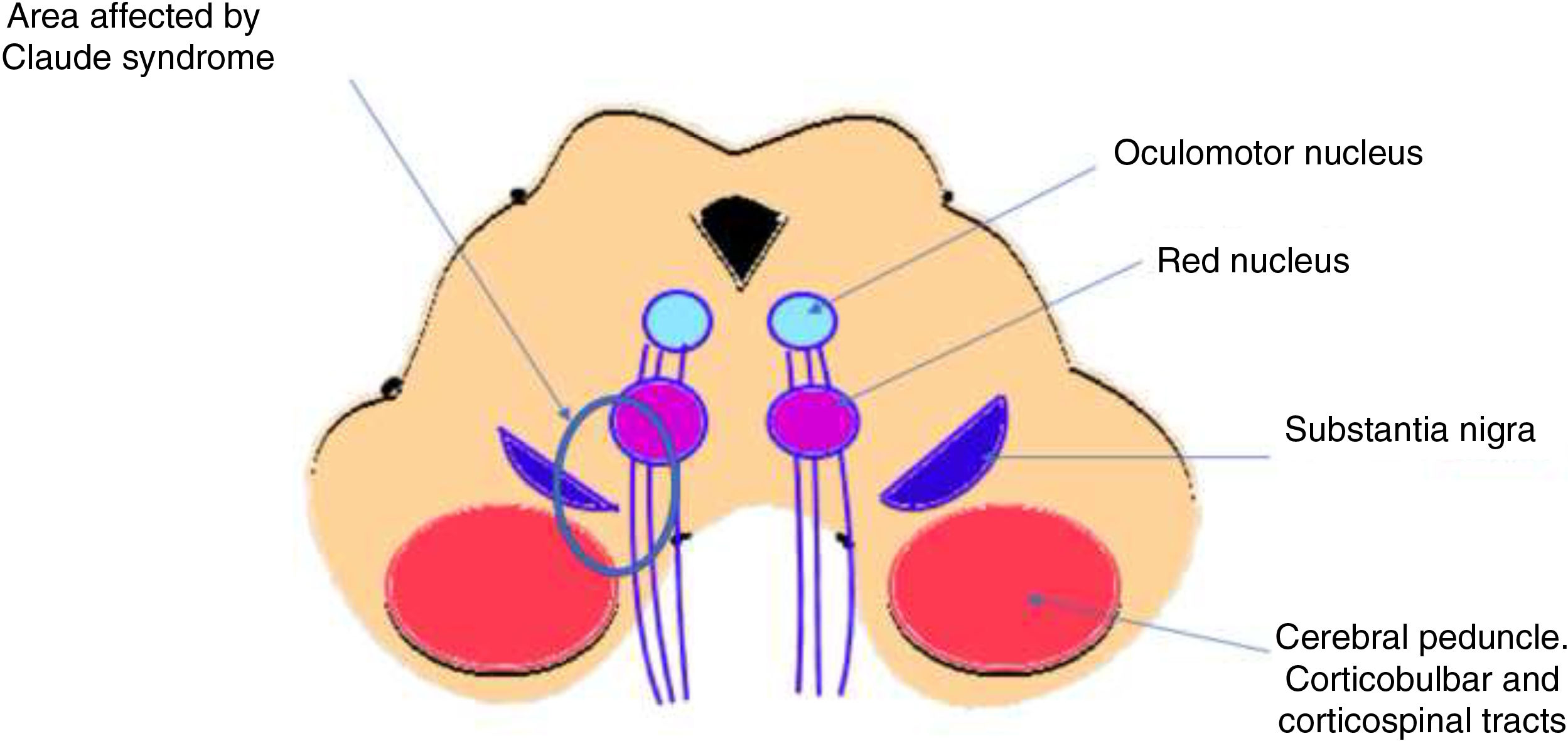
The patient presented ischaemic midbrain infarction as a result of trauma; findings were compatible with involvement of the interpeduncular arteries fed by the posterior cerebral artery and basilar artery.2 The literature includes reports of midbrain syndromes of vascular aetiology presenting ipsilateral third cranial nerve palsy, with contralateral cerebellar signs (Fig. 2). Benedikt syndrome (paramedian midbrain syndrome) is characterised by varying levels of ipsilateral third cranial nerve palsy, hemiparesis, and contralateral tremor. Claude syndrome (lesion to the dorsal midbrain tegmentum) is characterised by partial third cranial nerve palsy with contralateral tremor and/or ataxia. Cases of Benedikt3,4 syndrome secondary to trauma are very rare. The proposed mechanism is that rotational forces and acceleration involved in head trauma exert pressure on the diencephalic-mesencephalic junction, damaging the perforating arteries, in addition to compression of the midbrain by the tentorium.3 To our knowledge, ours is the first case of post-traumatic Claude syndrome.
Please cite this article as: Garrido-Fernández A., Monge-Galindo L., García-Íñiguez J.P., López-Pisón J. Síndrome de Claude secundario a traumatismo craneoencefálico. Neurología. 2020;35:350–352.