Optimization of treatment of diabetes mellitus involves an increased risk of hypoglycemia,1–3 which may be asymptomatic.4 On the other hand, seizures may be triggered by hypoglycemia,5,6 and the monitoring of patients with both diabetes and epilepsy therefore requires special attention.
We report a female patient with type 1 diabetes mellitus (T1DM) and epilepsy with generalized tonic-clonic and complex partial seizures and photosensitive absences who experienced a seizure while carrying a continuous glucose monitoring (CGM) device. The patient was 35 years old at the time of the episode and had been diagnosed with T1DM at 7 years and with epilepsy at 16 years. Her seizures were usually triggered by stress, sleep deprivation, and hypoglycemia. The patient's DM had been treated with an insulin pump since 2003, before her pregnancy. This treatment had been discontinued after delivery and restarted in 2006 due to poor glycemic control treated with multiple doses of insulin analogues. Glycosylated hemoglobin (HbA1c) level was 7.2% in the months preceding admission, but since the patient was being monitored for pregnancy, intermittent CGM was decided upon to improve glycemic control. The patient had been treated for epilepsy since 2002 with lamotrigine (current dose, 500mg/day) and experienced 1–2 seizures per year, most of them coinciding with one of the abovementioned triggering factors.
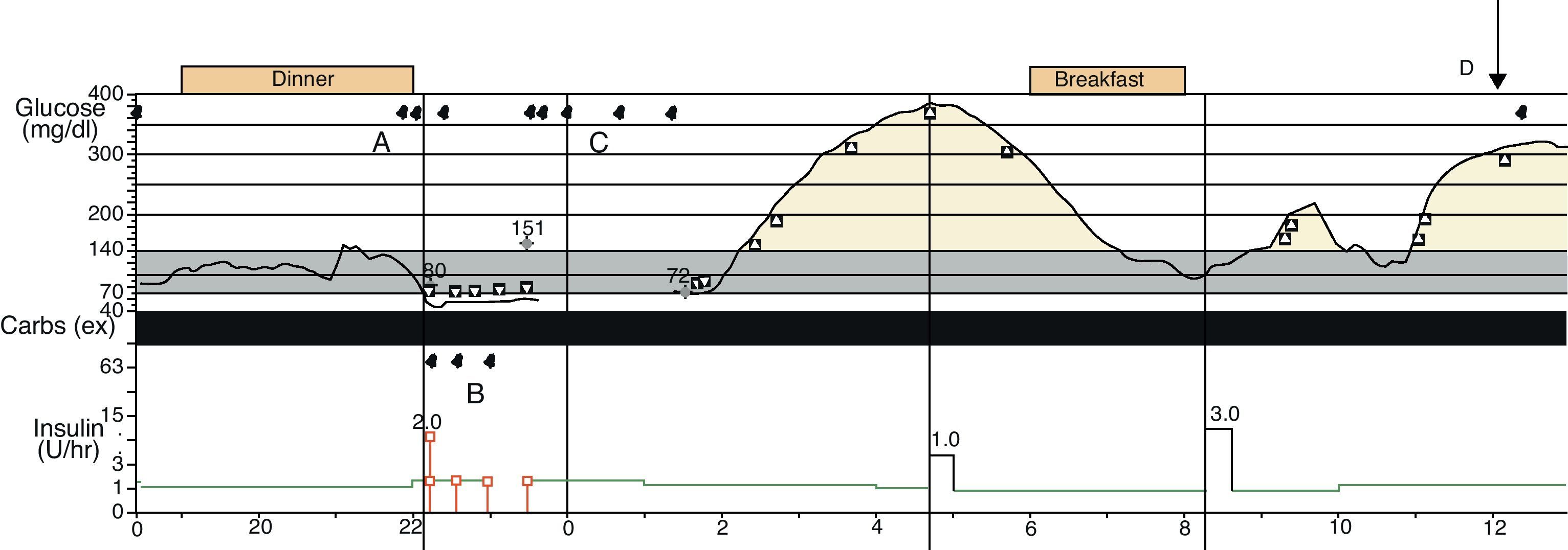
In July 2010, she was brought by ambulance to the casualty ward of the hospital after suffering a tonic-clonic seizure at midday in her workplace. Blood glucose on arrival was 147mg/dL. The patient showed bradypsychia, but no focal neurological signs or other abnormalities on examination. She had had a continuous glucose infusion pump implanted and a glucosensor inserted 2 days before. Thirty minutes after arrival, the patient experienced two episodes of the same characteristics that were treated with clonazepam. The concomitant blood glucose level was 140mg/dL. Impregnation was started with valproic acid, continuous subcutaneous insulin infusion was replaced by intravenous infusion and the glucosensor was removed for reading. When the patient could be questioned, she denied missing any doses of antiepileptic medication or any recent occurrence of hypoglycemia. On the previous night, monitoring and infusion systems had set off 11 alarms in a 4-h period (Fig. 1) for low glucose, pump stop, discrepancy between calibration values, and glucosensor reading. Capillary blood glucose readings did not confirm hypoglycemia in any of these cases.
Continuous glucose monitoring record. Blood glucose recording, pump activity, and alarms of the continuous glucose monitoring system are shown: (A) Alarms for low glucose readings. (B) Alarms for pump stop. (C) Alarms for discrepancy between the sensor-recorded and manual calibration values. (D) Time of seizure.
Work-up at the neurology department included sleep disturbances caused by alarms on the previous night. The patient responded to most alarms by measuring capillary blood glucose with the reflectometer and/or restarting the pump, which meant that she woke up several times and so did not achieve a refreshing sleep. For this reason, sleep deprivation was considered to act as the trigger of the seizure. The patient was discharged on treatment with her usual insulin and lamotrigine scheme, in addition to valproic acid in a decreasing dose because of her wish to become pregnant. Record assessment (Fig. 1) revealed multiple alarms during the previous night and a period when the glucosensor did not provide readings, from around midnight to 2:30 in the morning. At the time of the first seizure, blood glucose measured by the sensor was markedly high.
We can state that the seizure experienced by our patient was not caused by hypoglycemia, because even if hypoglycemia existed when the sensor alarms sounded, the seizure occurred more than 4h later, which is the period during which hypoglycemia has been reported to act as a trigger.7 It is impossible to know if the episode would have occurred if there had been no sleep deprivation, but since most seizures occurred in the patient concomitantly with a trigger and the most common factors triggering seizures are sleep deprivation and stress,8 it seems plausible that this acted as the triggering factor. On the other hand, sleep disturbances are not uncommon in patients with an implanted glucosensor, an event which was first reported in 2007.9,10 For this patient to benefit from CGM safely and with no risk of seizures, it was considered appropriate to set the hypoglycemia alarm at a blood glucose level of 50mg/dL.
We thank Sandra Iglesias, from Medtronic, for her assistance in interpretation of recording results.
Please, cite this article as: Alcántara V, et al. Crisis comicial en paciente diabética. ¿Hipoglucemia o efecto secundario de la monitorización continua de glucosa? Endocrinol Nutr. 2012;59:144–6.