The first case of coronavirus disease 2019 (COVID-19) was detected in Wuhan (China) in December 2019; from then, it started to spread throughout the world. Confirmed cases and deaths shot up rapidly,1 taking an emotional toll on the population, with symptoms of anxiety, stress and depression.2
In Spain, schools shut down between 9 March and 13 March 2020. On 14 March, a state of alarm was declared, and on 16 March, the population was put in lockdown. On 5 April 2020, 130,759 cases of COVID-19 had been recorded in Spain, 1,200,000 cases had been confirmed worldwide and more than 68,000 people had died.1 Spain became the country with the third largest number of people affected by this pandemic in the world.
For many citizens, this was their first social and healthcare emergency, caused by a viral agent, giving rise to a great deal of uncertainty and adverse health consequences.1
The pandemic might have prompted a change in the type and number of referrals to different specialisations; therefore, we set out to determine whether there was a decrease or delay in referrals to paediatric endocrinology at a tertiary hospital, as well as their distribution. To this was added a subjective impression among paediatric endocrinology staff of an increase in the number of referrals for precocious puberty, which made it necessary to confirm whether the pandemic was influencing the time of onset of puberty, as a third objective.
We conducted a retrospective case–control study with non-probability consecutive sampling of children under 14 years of age first referred from primary and specialised care to the paediatric endocrinology department of a tertiary hospital between March 2019 and December 2019 or March 2020 to December 2020, recorded in the consultation software program.
Data were collected on all primary and secondary diagnoses from the first visit, as well as the month of referral.
The criteria used for patient selection were:
- •
Inclusion criteria: children under 14 years of age first referred to the paediatric endocrinology department at our hospital during an 18-month period.
- •
Exclusion criteria: age over 14 years, false first visits and duplicate referrals for a single patient.
Statistical analysis consisting of comparison of independent means was carried out using R software. The inferential test of normality using the Shapiro–Wilk test was applied in advance.
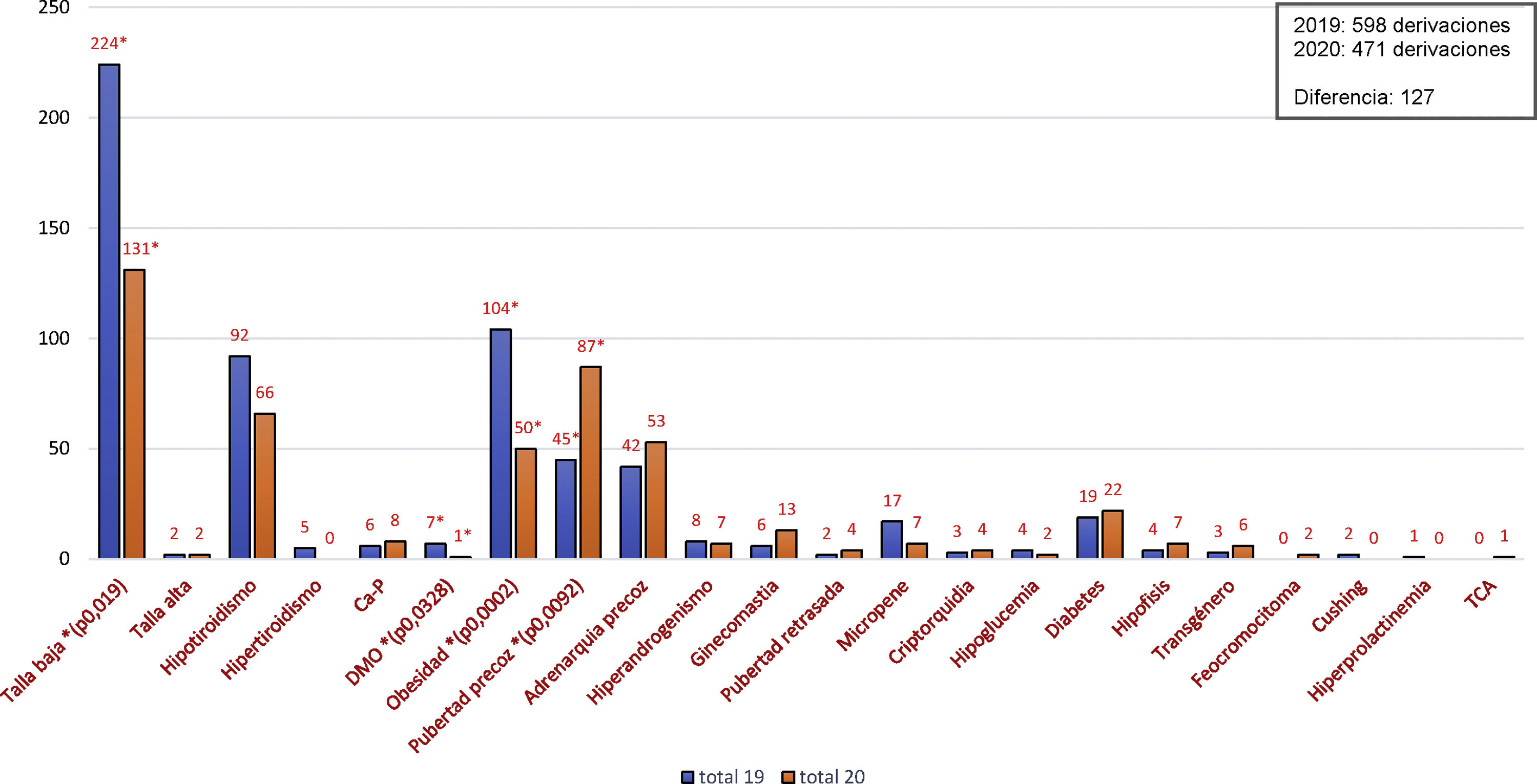
In 2019, there were a total of 598 referrals to the paediatric endocrinology department meeting the established criteria (control group), whereas in 2020, there were a total of 471 referrals in the same time period.
The most common reasons for referral during the control period were: short stature 37.5% (224/598), obesity 17.4% (104/598) and hypothyroidism 15.4% (92/598); the most common reasons for referral in the 2020 case group were: short stature 27.8% (131/471), precocious puberty 18.5% (87/471) and hypothyroidism 14% (66/471) (Fig. 1).
Given that these were normal samples, the differences between all the reasons for referral were analysed using Student’s t test, yielding statistical significance for short stature (p=0.0019), obesity (p=0.0002), precocious puberty (p=0.0092) and bone mineral density abnormalities (p=0.0328).
A homogeneous distribution in referrals in 2019 was seen, with a decrease during the holiday months, whereas in 2020 there was a predominance of referrals in the final three months of the year.
Lockdowns, school closures and the need for social distancing led to less exercise, less healthy eating and longer periods of time at home and in front of screens.3 In addition, anxiety and financial concerns among parents, along with fears of becoming ill, might have caused stress in children.4 These psychological and environmental factors stimulate insulin-like growth factor, glucose and leptin, and inhibit melatonin, which can stimulate gonadotropin-releasing hormone (GnRH), a hormone released by hypothalamic neurons.5,6 In addition, increased sedentary behaviours are correlated with elevated body mass index, which in turn induces puberty.7,8 In our case, although referrals for obesity decreased, there was a subjective sense of an increase in weight of the patients seen.
Backing this theory was the finding in our practice of an increase in referrals for precocious puberty, as in Italian groups.9,10 Verzani et al. presented a sample of both sexes larger than our own (n=224), but arrived at the same conclusions,9 while Stagi et al. had a smaller sample than ours (n=37) consisting of females only10. However, Stagi et al. found that the new cases of precocious puberty occurred at a younger age with a higher luteinising hormone and oestradiol peak, a higher ovarian volume, a larger uterus and a more advanced Tanner stage at diagnosis than in the control group. They also reported a more rapid course of puberty in cases that were premature, already known and diagnosed prior to the pandemic.9 Finally, they indicated an increased body mass index and greater use of technological devices in the control group; this would support our hypothesis on the impact of these things during the pandemic as a trigger of puberty.10 This was part of one of the limitations of our study, since we were unable to verify an increase in body mass index in the entirety of our control group due to information bias.
In conclusion, our sample showed a significant increase in new cases of precocious puberty during the COVID-19 pandemic. In addition, referrals for short stature, obesity and osteoporosis decreased in our department in 2020, and the distribution of referrals during 2020 varied, with an increase in the final months of the year.
AuthorshipAna B. Ariza Jimenez designed and drafted the article. Francisco J. Aguilar Gomez Cardenas helped with data collection. Carmen de la Camara Moraño supervised the article. All the authors reviewed this manuscript, assume full responsibility for it and approve its publication.
Conflicts of interestThe authors declare that they have no conflicts of interest.