Despite the favorable evidence available, our public health care system has no specific programs including therapeutic education for patients newly diagnosed with type 2 diabetes (T2DM), which would be crucial for the subsequent course of the disease.
ObjectivesTo assess the effectiveness of a “Health care and Therapeutic Education Program for newly diagnosed type 2 diabetes (PAET-Debut DM2)” agreed by the primary care centers and the reference hospital in a given geographical area.
MethodsA prospective pilot study in patients over 18 years of age diagnosed with T2DM between February 2012 and 2013. The PAET-DebutDM2 is planned and set up in four primary care centers in the area covered by Hospital Clínic in Barcelona. Reference persons (family doctor and nurse) are designated at each center and specific training is provided to standardize the clinical processes and therapeutic education methods. First results are assessed and compared at 6 and 12 months.
ResultsThe program was proposed to 345 patients, of which 191 (55.3%) were enrolled in it and 134 (70.2%) completed the program. At the end of the program, 84% achieved the control goal (HbA1c<7%) and 88% passed the screening of chronic complications. Improvements were seen in body weight, physical activity (p<0.001), and disease awareness (p<0.05), and there were less hospital emergencies due to DM as compared to patients not included in the program (p=0.023).
ConclusionThe PAET-DebutDM2 standardizes intervention and education and is effective in terms of clinical and educational results and patient satisfaction. The program emphasizes the importance of early education and intervention, reorganizing resources without increasing care pressure in the primary care centers, thus reducing hospital care.
A pesar de la evidencia favorable, existen pocas iniciativas en nuestro sistema público sobre programas específicos de educación terapéutica estructurada dirigidos a pacientes con diagnóstico reciente de diabetes tipo 2 (DM2), un momento de especial importancia en la evolución posterior de la enfermedad.
ObjetivosEvaluar la efectividad del Programa de Atención y educación Terapéutica en el debut de la DM2 (PAET-Debut DM2) de ámbito territorial y consensuado entre centros de Atención Primaria y Hospital de referencia.
MétodosEstudio piloto prospectivo en pacientes con edad>18 años diagnosticados de DM2 entre febrero 2012-2013. El PAET-DebutDM2 se planifica e implementa en 4 Centros de Atención Primaria del área de referencia del Hospital Clínic de Barcelona. Se identifican referentes (médico de familia y enfermera) en cada centro y se realiza formación específica para estandarización de procesos clínicos y metodología de educación terapéutica. Se evalúan resultados a los 6 y 12 meses.
ResultadosSe propone el programa a 345 pacientes, 191 (55,3%) son incluidos, finalizando 134 (70,2%). Al finalizar el programa el 84% de pacientes está en objetivos de control (HbA1c<7%) y 88% completa el cribado de complicaciones crónicas. Observamos una mejora del peso corporal, de la actividad física (p<0,001), del nivel de conocimientos (p<0,05), y constatamos menos urgencias hospitalarias por DM comparados con los no incluidos (p=0,023).
ConclusiónEl PAET-DebutDM2 estandariza la intervención, la educación y es efectivo en los resultados clínicos, educativos y de satisfacción del paciente. Enfatiza la importancia de la educación y de la intervención desde el debut, y reordena recursos, sin incrementar la presión asistencial en el centro de atención primaria, reduciendo la atención hospitalaria.
In Spain, the Di@bet.es Study has found the prevalence of type 2 diabetes (DM2) to be 13.8%, of which almost one-half (6%) corresponds to undiagnosed cases.1 Chronic complications of the disease have a significant impact on patient quality of life and a high human, social and economic cost.2–4 Cardiovascular disease is the leading cause of mortality among diabetics, with a coronary risk 2–4 times higher than in non-diabetics.5 Diabetes in general is the seventh most frequent cause of mortality among Spaniards.6 Fortunately, intensive management of the disease, particularly in its early stages, may not only help prevent microangiopathic complications, but also reduce the incidence of cardiovascular events, regardless of the degree of blood glucose control in more advanced stages of the disorder.7 However, it has been questioned whether intensive control in these more advanced stages offers benefit in terms of macrovascular complications and reduced mortality in general, particularly among elderly individuals and patients that already have chronic complications or significant comorbidity.8,9 Accordingly, in recent years intensive and multifactorial intervention has been advocated for disease control from the time of diagnosis of the disorder, as a basic preventive strategy.
Therapeutic education is an ongoing process that provides the knowledge, skills and capacities needed for self care among people with chronic diseases. According to the latest recommendations of the American Diabetes Association, anyone with diabetes should participate in education programs from the time of the diagnosis of the disease.10 The aim of therapeutic education is to help individuals in informed decision-making, facilitate adherence to self-management and contribute to problem-solving in collaboration with healthcare professionals in order to improve disease control and quality of life.11 Quality standards recommend that the objectives of the educational programs be clearly drafted, and that their structure and the process to be followed by the patient and/or family be well defined. Furthermore, there should be an evaluation of the outcome, regarding both the patient and the program in general, in order to facilitate the continuous improvement of quality care.12,13
Structured programs which focus on patient care at DM2 onset are available in other countries in Europe, such as the United Kingdom (the DESMOND Newly Diagnosed program).14,15 However, while preventive strategies16 and peer training initiatives are found in Spain,17 few initiatives focus on the onset of the disease. For this reason, and based on the favorable evidence available, we decided as a general objective to evaluate the effectiveness of the pilot “Healthcare and Therapeutic Education Program for newly diagnosed type 2 diabetes” (Programa de Atención y Educación Terapéutica en el debut de la DM2 [PAET-Debut DM2]), coordinated between primary and hospital care, in clinical, educational and care organizational terms.
Material and methodsA one-year longitudinal, prospective, pragmatic pilot study evaluating patients and interventions at baseline and after 6 and 12 months was carried out. The inclusion criteria were: patients newly diagnosed with DM2 between February 2012 and February 2013, aged>18 years, and attended to at four primary care centers (PCCs): Carles Riba (Institut Català de la Salut), Casanova, Comte Borrell and Les Corts (Consorci d’Atenció Primària de Salut Barcelona Esquerra), all within the reference area of Hospital Clínic de Barcelona, and covered by the Àrea de Atención Integral-Barcelona Esquerra (AISBE). The exclusion criteria included: patients participating in clinical trials, patients included in home care programs, frail patients (of advanced age, with complex or severe psychiatric multidisease, or with terminal conditions associated with a short life expectancy), or patients not interested in participating in the program. Informed consent was not required, since the pilot study retrospectively assessed implementation of the program in standard practice at the participating centers. The methodology used can be divided into two sections: (1) the identification of patients with newly diagnosed diabetes, emphasis being placed on the importance of this specific moment in the natural course of the disease; and (2) the standardization of the basic and quality therapeutic education which patients should receive in order to ensure their early enablement and active participation in treatment and decision-making, with a view to improving their self-care. The specific objective of the methodology used was to ensure an early improvement in disease control and to prevent chronic micro- and macrovascular complications.
Characteristics of the structured Healthcare and Therapeutic Education Program for newly diagnosed type 2 diabetesThe program was agreed within the AISBE group for chronic diabetes disease with the support of the management bodies of the PCCs and of Hospital Clínic de Barcelona. The program is a clinical-educational initiative which focuses on the onset of the disease in a group of patients who previously received care according to the non-standardized clinical practice of each primary care professional and team, and on providing therapeutic education on an individualized basis. The planning of the structured program involved the participation of primary care professionals and the Endocrinology department of the hospital, and was based on clinical practice18 and educational guides,19 although the required reorganization of the available resources was conditioned by the need not to increase them. The contents, educational methods and support materials were established by consensus, along with the visiting schedule, screening for chronic complications, laboratory tests, and the evaluation of the results. Each PCC identified a general practitioner and a nurse who acted as program references (GP-R and N-R), and who were in charge of the diffusion and support of the initiative among all the medical (GP) and nursing professionals (N) in their respective centers. The GP-R and N-R received specific training in the form of a three-day course for both professionals and a practical stay at Hospital Clínic de Barcelona (for the N-R), with active participation in the group dynamics of the structured basic patient and family education program that was implemented in the department some years ago.
The study was approved by the Clinical Research Ethics Committee of Hospital Clínic de Barcelona (reference number: HCB/2012/8008).
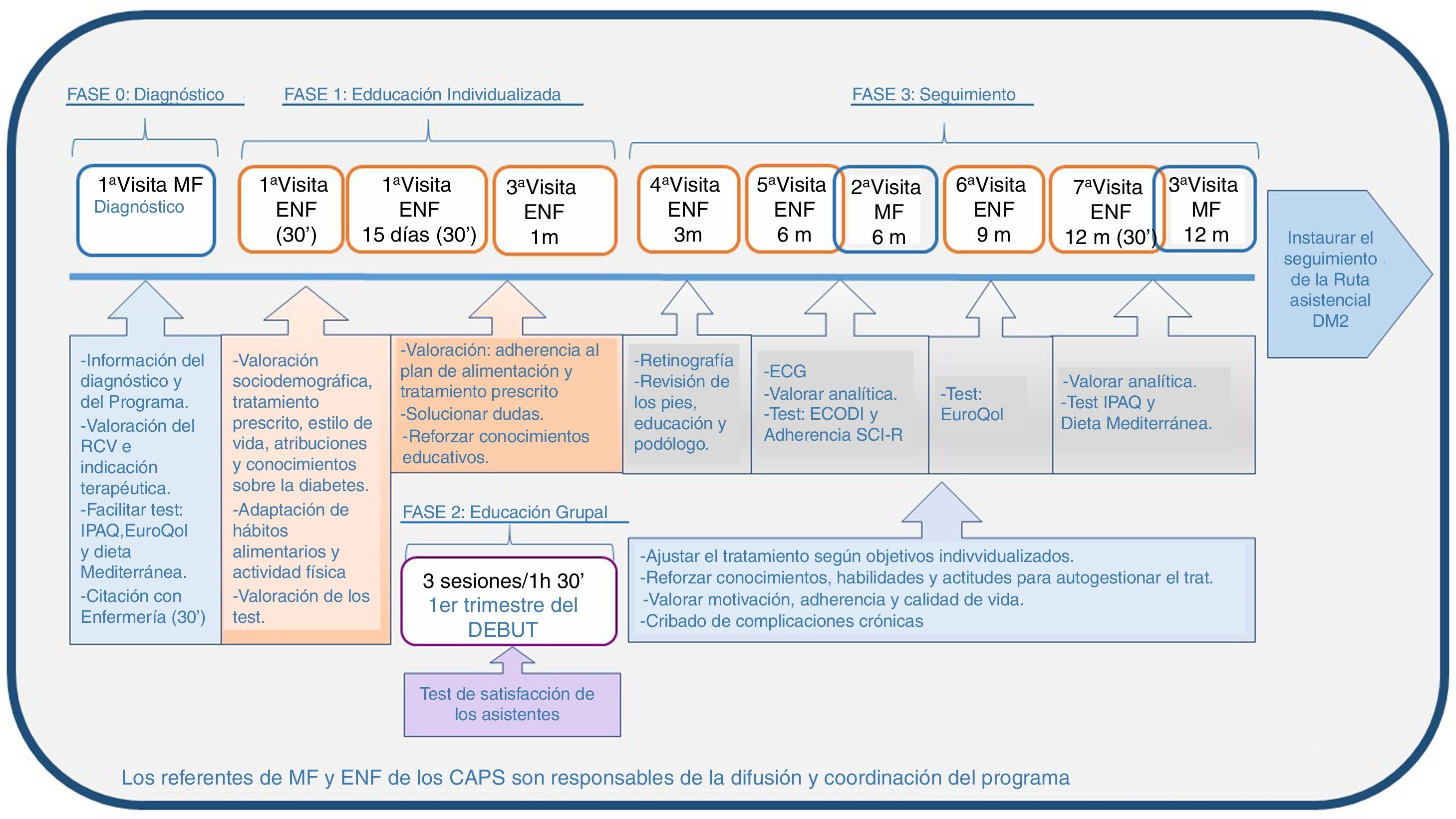
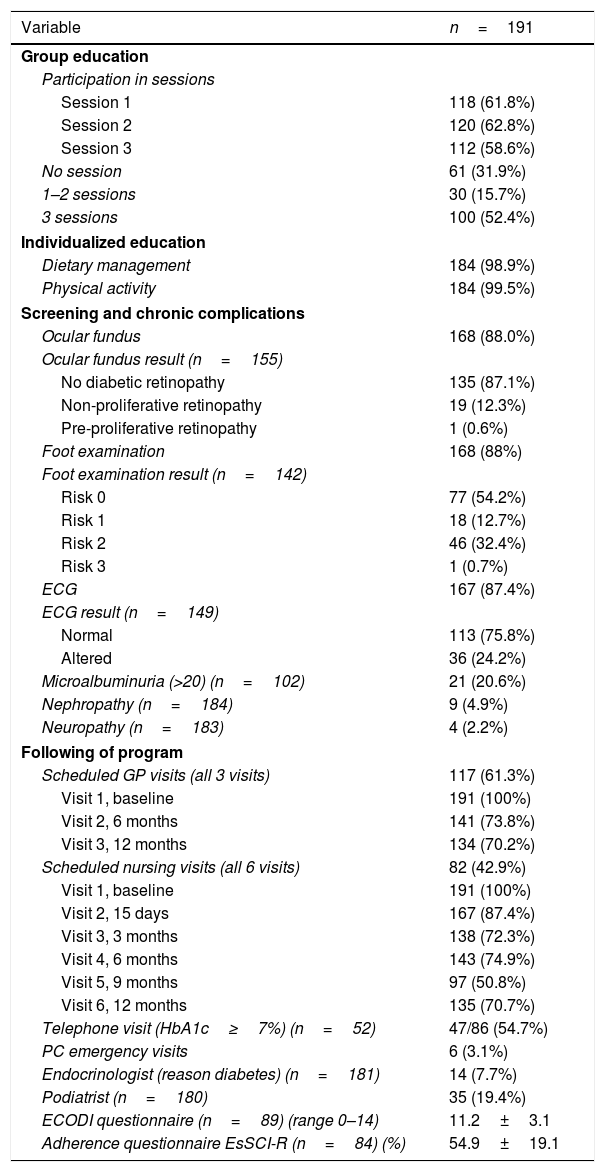
The program consists of four phases (Fig. 1).
Phase 0 (diagnosis). The GP responsible for each patient confirms and reports the diagnosis, assesses the patient on a multifactorial basis, and prescribes the required treatment. The GP offers participation in PAET-DebutDM2, provides the information sheet on the program detailing the course and type of intervention during that year, supplies the questionnaires assessing patient lifestyle (Mediterranean diet, IPAQ, EuroQoL), and refers the patient to his/her nurse to continue the program.
Phase 1 (individualized education visits). In the first month, three individual visits are made: two visits in person, each lasting 30min (one initial visit and another after 15 days), and a third telephone visit after 30 days. Socio-demographic data, prescribed treatment, lifestyle, and capacity to deal with and knowledge about diabetes are assessed on the first visit. A diet and physical activity plan is agreed based on the nutritional needs, metabolic requirements and habits of the patient. Training is also provided regarding both the measurement of and awareness of the significance of capillary blood glucose, if required. The second personal visit (+15 days) and the telephone visit serve to reinforce the educational concepts and adjust the blood glucose-lowering pharmacological and non-pharmacological treatment, if necessary.
Phase 2 (standardized group education). The patients are offered participation in three group sessions lasting 90min each during the first trimester, their educational content and materials being predefined, structured and homogeneous for all the participating centers.
First session: What is diabetes? Why is good diabetes control important?
Second session: How can blood glucose levels be controlled? Physical activity and healthy eating habits.
Third session: Acute and chronic complications of diabetes.
Phase 3 (follow-up). Nursing follow-up includes four additional individual visits after 3, 6, 9 and 12 months. The treatment is adjusted to the goals. Knowledge, skills and attitudes for the daily self-management of treatment are reinforced. Motivation, adherence and quality of life are assessed. Screening for chronic complications (neuropathy, peripheral arterial disease, retinopathy, referral for oral examination, electrocardiogram) and laboratory tests are performed after 6 and 12 months. During this period, the GP makes two visits after 6 and 12 months, with modification of the drug treatment if required, and a review of the requested tests and laboratory findings. The program ends after 12 months with patient discharge from the program and conventional follow-up according to the DM2 management protocol of the AISBE.
Variables analyzed and evaluation methodologyVariables analyzedSocio-demographic parameters: age, gender, social and cultural context (cohabitation, educational level, profession, ethnicity).
Clinical parameters: family history of diabetes, cardiovascular risk factors (blood pressure, weight, height, the body mass index [BMI], abdominal circumference), and metabolic control or complications/comorbidities (glycosylated hemoglobin [HA1c], the lipid profile, creatinine, microalbuminuria, the albumin/creatinine index). The type of pharmacological and non-pharmacological treatment for diabetes and cardiovascular risk factors was recorded. Chronic complications (retinopathy, nephropathy, vascular disease and peripheral neuropathy) were assessed.
Lifestyle and therapeutic education: lifestyle habits were assessed using validated questionnaires at baseline and after 12 months referring to diet (14-item Predimed Mediterranean Diet Questionnaire [0–14])20 and physical activity (IPAQ questionnaire),21 with classification into low/moderate/high categories, as well as alcohol consumption and smoking. Specific questionnaires were used to assess subjective perception of health at baseline and after 9 months (EuroQoL numerical scale [0–100]),22 while after 6 months treatment adherence in diabetes was assessed (SCR-I questionnaire),23 along with knowledge (ECODI questionnaire [0–14]).24 An ad hoc questionnaire evaluating satisfaction with the group activity of the program was administered at the end of the activity.
Organizational-management parameters: the program variables included the number of patients enrolled, those involved in group education, the number of medical and nursing visits (scheduled by the program or otherwise), telephone visits, hospital admissions and emergency room visits due to diabetes.
The clinical or management data were compiled from the primary care and hospital electronic databases. At the end of the program, the GP-R and N-R audited the clinical histories and compiled the data corresponding to the patients included and excluded from the program.
Data analysisCategorical variables were reported as absolute frequencies and percentages. Continuous variables were reported as the mean and standard deviation (SD) or median and interquartile range (IQR). The Wilcoxon signed rank test was used for the comparison of continuous variables between the baseline visit and after 4–6 months and the final visit. Categorical variables were compared between visits using the McNemar test. The Jonckheere trend test, equivalent to the Kruskal–Wallis test but applied to ordered categories, was used to explore possible trends between successive visits. All results were presented with the corresponding p-value and confidence interval estimation. A statistical significance level of 5% was considered, using the R version 3.2.3 statistical package for MS Windows.
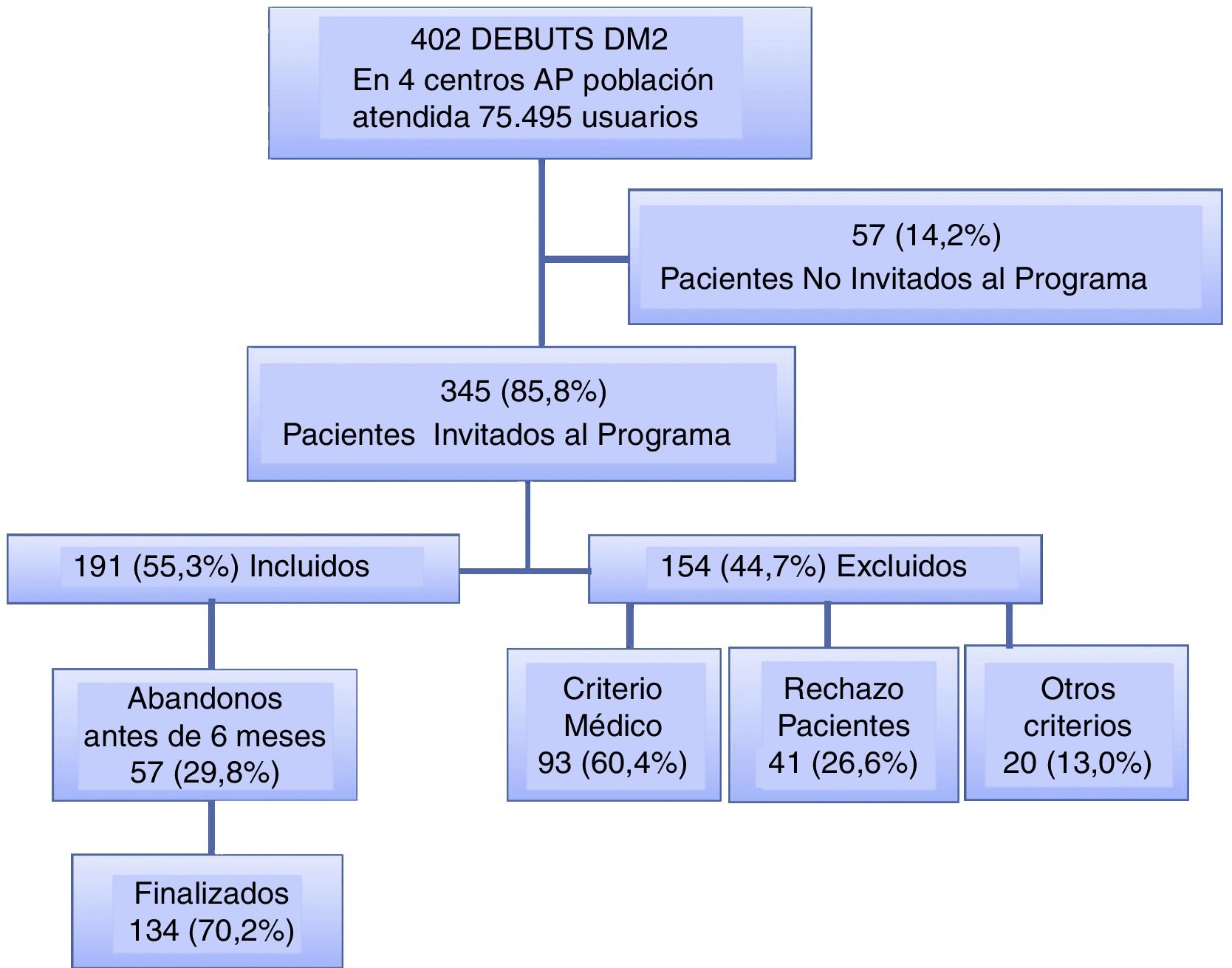
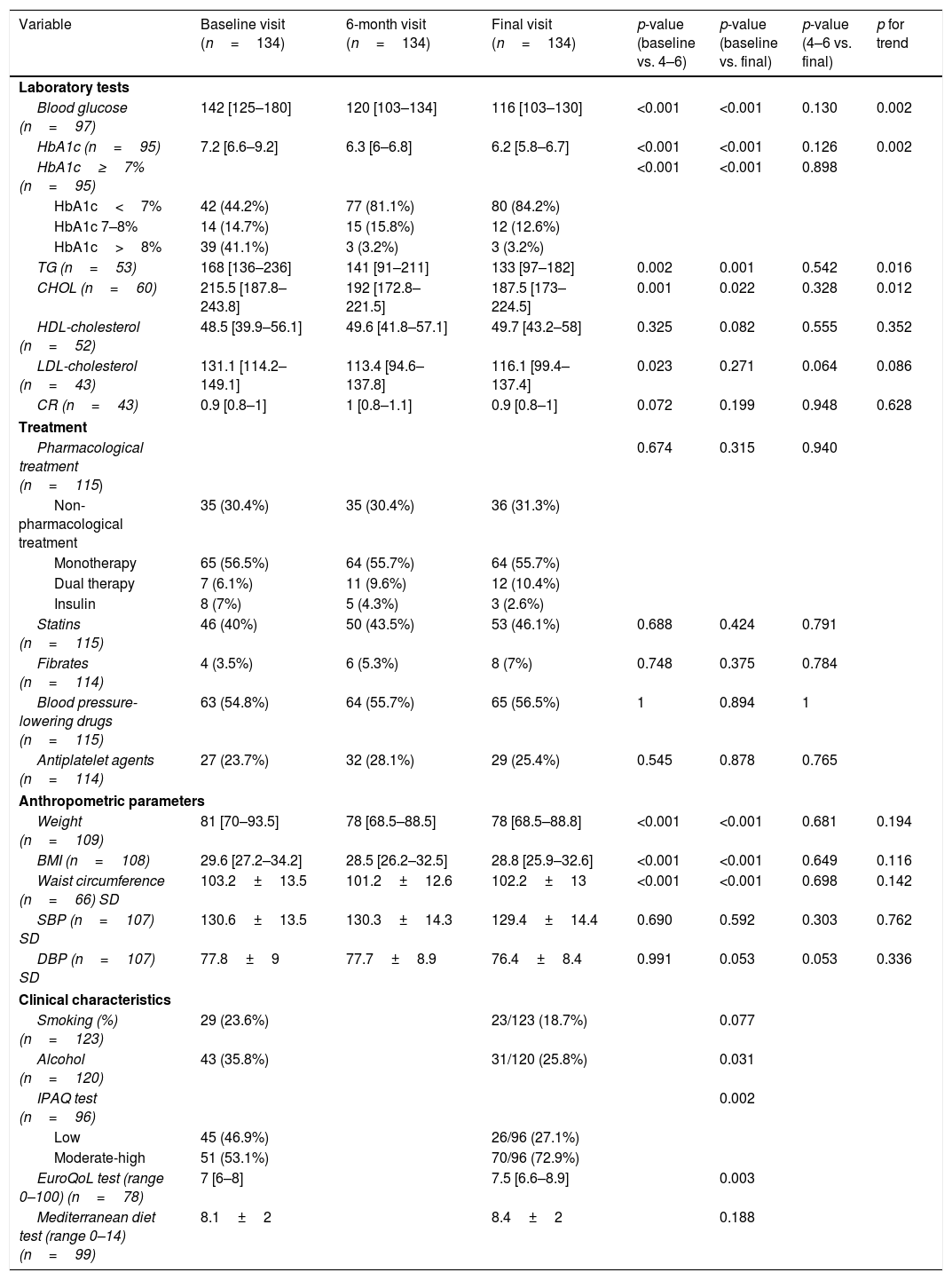
ResultsPatient characteristicsA total of 402 patients were diagnosed with DM2 in the four PCCs during the study period (incidence 5.3 cases/1000 patients/year). Of these, 345 patients (85.8%) were invited to enter the program by their primary care teams, and 191 of them (55.3%) were subsequently enrolled while 154 (44.7%) were not. The most common reason given for non-enrolment was medical (advanced age, multiple diseases, oncological disease, or psychiatric disorders) (60.4%), followed by patient reluctance to undergo structured follow-up (private or mutual follow-up) (26.6%) and other reasons (13.0%). Fig. 2 shows the patient flow. Of those enrolled in the program, 134 (70.2%) completed it, while 57 (29.8%) discontinued it before they had completed 6 months.
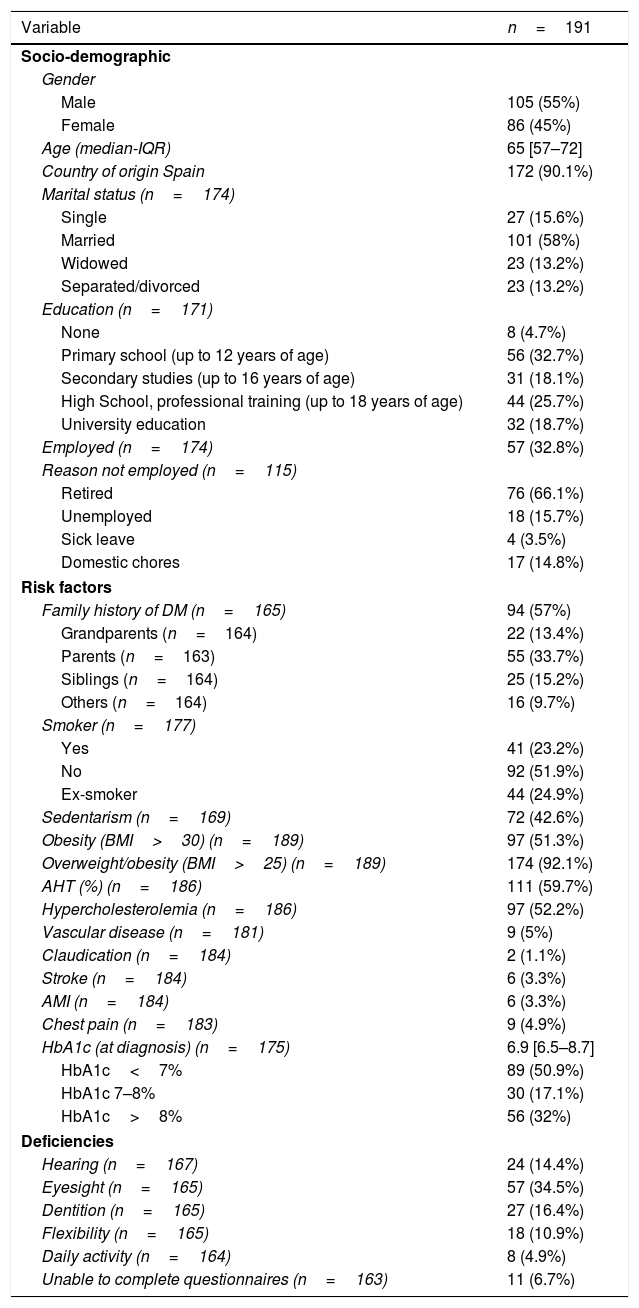
Table 1 describes the characteristics of the population included in the program. The median age was 65 years (IQR 57–72); 55% were men; and most of the subjects (67.2%) were not occupationally active. There was a high prevalence of a family history of diabetes (57%) and associated cardiovascular risk factors. At diagnosis of DM2, 51% of the patients presented HbA1c<7% and 32% HbA1c>8%.
Patient socio-demographic characteristics and risk factors at diagnosis.
| Variable | n=191 |
|---|---|
| Socio-demographic | |
| Gender | |
| Male | 105 (55%) |
| Female | 86 (45%) |
| Age (median-IQR) | 65 [57–72] |
| Country of origin Spain | 172 (90.1%) |
| Marital status (n=174) | |
| Single | 27 (15.6%) |
| Married | 101 (58%) |
| Widowed | 23 (13.2%) |
| Separated/divorced | 23 (13.2%) |
| Education (n=171) | |
| None | 8 (4.7%) |
| Primary school (up to 12 years of age) | 56 (32.7%) |
| Secondary studies (up to 16 years of age) | 31 (18.1%) |
| High School, professional training (up to 18 years of age) | 44 (25.7%) |
| University education | 32 (18.7%) |
| Employed (n=174) | 57 (32.8%) |
| Reason not employed (n=115) | |
| Retired | 76 (66.1%) |
| Unemployed | 18 (15.7%) |
| Sick leave | 4 (3.5%) |
| Domestic chores | 17 (14.8%) |
| Risk factors | |
| Family history of DM (n=165) | 94 (57%) |
| Grandparents (n=164) | 22 (13.4%) |
| Parents (n=163) | 55 (33.7%) |
| Siblings (n=164) | 25 (15.2%) |
| Others (n=164) | 16 (9.7%) |
| Smoker (n=177) | |
| Yes | 41 (23.2%) |
| No | 92 (51.9%) |
| Ex-smoker | 44 (24.9%) |
| Sedentarism (n=169) | 72 (42.6%) |
| Obesity (BMI>30) (n=189) | 97 (51.3%) |
| Overweight/obesity (BMI>25) (n=189) | 174 (92.1%) |
| AHT (%) (n=186) | 111 (59.7%) |
| Hypercholesterolemia (n=186) | 97 (52.2%) |
| Vascular disease (n=181) | 9 (5%) |
| Claudication (n=184) | 2 (1.1%) |
| Stroke (n=184) | 6 (3.3%) |
| AMI (n=184) | 6 (3.3%) |
| Chest pain (n=183) | 9 (4.9%) |
| HbA1c (at diagnosis) (n=175) | 6.9 [6.5–8.7] |
| HbA1c<7% | 89 (50.9%) |
| HbA1c 7–8% | 30 (17.1%) |
| HbA1c>8% | 56 (32%) |
| Deficiencies | |
| Hearing (n=167) | 24 (14.4%) |
| Eyesight (n=165) | 57 (34.5%) |
| Dentition (n=165) | 27 (16.4%) |
| Flexibility (n=165) | 18 (10.9%) |
| Daily activity (n=164) | 8 (4.9%) |
| Unable to complete questionnaires (n=163) | 11 (6.7%) |
As previously described (Fig. 1), the main part of the individualized, consensus-based and structured therapeutic educational intervention took place in the first trimester. Group education is an important part of therapeutic education in the program. The results were therefore reported based on full participation (52.4%), partial participation in the form of 1–2 sessions (15.7%), or no attendance (31.9%) (Table 2). The levels of acquired knowledge (ECODI) and adherence (SCR-I) were related to participation in the group education sessions. Those who did not receive group education but received individualized education yielded a mean ECODI score of 9.9; those who attended one or two sessions yielded a score of 10; and those who attended all sessions yielded a score of 11.9 (p=0.011). In the case of SCR-I, the mean score was higher in those who completed all three sessions (58.7 versus 51.3 in those with <3 sessions). The assessment of group education by the participants was considered to be very helpful in terms of the information (99%) and recommendations received (97%), and most participants (99%) would recommend it to other diabetic people.
Therapeutic education and follow-up.
| Variable | n=191 |
|---|---|
| Group education | |
| Participation in sessions | |
| Session 1 | 118 (61.8%) |
| Session 2 | 120 (62.8%) |
| Session 3 | 112 (58.6%) |
| No session | 61 (31.9%) |
| 1–2 sessions | 30 (15.7%) |
| 3 sessions | 100 (52.4%) |
| Individualized education | |
| Dietary management | 184 (98.9%) |
| Physical activity | 184 (99.5%) |
| Screening and chronic complications | |
| Ocular fundus | 168 (88.0%) |
| Ocular fundus result (n=155) | |
| No diabetic retinopathy | 135 (87.1%) |
| Non-proliferative retinopathy | 19 (12.3%) |
| Pre-proliferative retinopathy | 1 (0.6%) |
| Foot examination | 168 (88%) |
| Foot examination result (n=142) | |
| Risk 0 | 77 (54.2%) |
| Risk 1 | 18 (12.7%) |
| Risk 2 | 46 (32.4%) |
| Risk 3 | 1 (0.7%) |
| ECG | 167 (87.4%) |
| ECG result (n=149) | |
| Normal | 113 (75.8%) |
| Altered | 36 (24.2%) |
| Microalbuminuria (>20) (n=102) | 21 (20.6%) |
| Nephropathy (n=184) | 9 (4.9%) |
| Neuropathy (n=183) | 4 (2.2%) |
| Following of program | |
| Scheduled GP visits (all 3 visits) | 117 (61.3%) |
| Visit 1, baseline | 191 (100%) |
| Visit 2, 6 months | 141 (73.8%) |
| Visit 3, 12 months | 134 (70.2%) |
| Scheduled nursing visits (all 6 visits) | 82 (42.9%) |
| Visit 1, baseline | 191 (100%) |
| Visit 2, 15 days | 167 (87.4%) |
| Visit 3, 3 months | 138 (72.3%) |
| Visit 4, 6 months | 143 (74.9%) |
| Visit 5, 9 months | 97 (50.8%) |
| Visit 6, 12 months | 135 (70.7%) |
| Telephone visit (HbA1c≥7%) (n=52) | 47/86 (54.7%) |
| PC emergency visits | 6 (3.1%) |
| Endocrinologist (reason diabetes) (n=181) | 14 (7.7%) |
| Podiatrist (n=180) | 35 (19.4%) |
| ECODI questionnaire (n=89) (range 0–14) | 11.2±3.1 |
| Adherence questionnaire EsSCI-R (n=84) (%) | 54.9±19.1 |
With regard to follow-up of the program, the mean completion rate of the three scheduled visits with the GP was 81.3%, versus 76% for the 6 nursing visits. In addition to the scheduled visits, during follow-up 6 participants (3.1%) reported for unscheduled visits to primary care related to DM; 14 (7.7%) were referred to the endocrinologist; and 35 (19.4%) were referred to the podiatrist. Screening was made for chronic complications in the form of retinopathy (non-mydriatic chamber) in 88.0% of the participants, with the detection of retinopathy in 12.9% of them; neurovascular disease was assessed in 88%, with the identification of foot at risk (2/3 according to the RedGDPS scale) in 33.1%; electrocardiography was performed and assessed by the GP in 87.4% of the participants, with the identification of alterations in 24.2%; and microalbuminuria was assessed in 53.4%, with the observation of levels >20mg/l in 20.6% of the patients (Table 2).
Impact of the intervention upon the clinical, anthropometric and treatment parametersTable 3 shows the clinical and/or laboratory data of those participants (n=134) for which such information was available at three program time points: baseline+6 months+12 months. A mean decrease in HbA1c (baseline median 7.2%) of 0.9% (IQR 0.3–2.4) and 0.9% (IQR 0.4–2.5) was observed at 6 months and 12 months, respectively (p<0.001) (Table 3). At the end of the program, 84.2% of the participants presented HbA1c<7%, 12.6% 7–8% and, 3.2%>8% (41% at the time of diagnosis). Among the patients requiring blood glucose-lowering treatment at baseline, most (56.5%) received oral monotherapy, 6.1% received dual oral therapy (versus 10.4% at the end), and 7% started insulin therapy (3.2% at the end) (Table 3). There were improvements in triglyceride (p=0.016), cholesterol (p=0.012) and LDL-cholesterol levels, particularly between baseline and the 6-month visit.
Impact of the intervention upon clinical, anthropometric and treatment parameters.
| Variable | Baseline visit (n=134) | 6-month visit (n=134) | Final visit (n=134) | p-value (baseline vs. 4–6) | p-value (baseline vs. final) | p-value (4–6 vs. final) | p for trend |
|---|---|---|---|---|---|---|---|
| Laboratory tests | |||||||
| Blood glucose (n=97) | 142 [125–180] | 120 [103–134] | 116 [103–130] | <0.001 | <0.001 | 0.130 | 0.002 |
| HbA1c (n=95) | 7.2 [6.6–9.2] | 6.3 [6–6.8] | 6.2 [5.8–6.7] | <0.001 | <0.001 | 0.126 | 0.002 |
| HbA1c≥7% (n=95) | <0.001 | <0.001 | 0.898 | ||||
| HbA1c<7% | 42 (44.2%) | 77 (81.1%) | 80 (84.2%) | ||||
| HbA1c 7–8% | 14 (14.7%) | 15 (15.8%) | 12 (12.6%) | ||||
| HbA1c>8% | 39 (41.1%) | 3 (3.2%) | 3 (3.2%) | ||||
| TG (n=53) | 168 [136–236] | 141 [91–211] | 133 [97–182] | 0.002 | 0.001 | 0.542 | 0.016 |
| CHOL (n=60) | 215.5 [187.8–243.8] | 192 [172.8–221.5] | 187.5 [173–224.5] | 0.001 | 0.022 | 0.328 | 0.012 |
| HDL-cholesterol (n=52) | 48.5 [39.9–56.1] | 49.6 [41.8–57.1] | 49.7 [43.2–58] | 0.325 | 0.082 | 0.555 | 0.352 |
| LDL-cholesterol (n=43) | 131.1 [114.2–149.1] | 113.4 [94.6–137.8] | 116.1 [99.4–137.4] | 0.023 | 0.271 | 0.064 | 0.086 |
| CR (n=43) | 0.9 [0.8–1] | 1 [0.8–1.1] | 0.9 [0.8–1] | 0.072 | 0.199 | 0.948 | 0.628 |
| Treatment | |||||||
| Pharmacological treatment (n=115) | 0.674 | 0.315 | 0.940 | ||||
| Non-pharmacological treatment | 35 (30.4%) | 35 (30.4%) | 36 (31.3%) | ||||
| Monotherapy | 65 (56.5%) | 64 (55.7%) | 64 (55.7%) | ||||
| Dual therapy | 7 (6.1%) | 11 (9.6%) | 12 (10.4%) | ||||
| Insulin | 8 (7%) | 5 (4.3%) | 3 (2.6%) | ||||
| Statins (n=115) | 46 (40%) | 50 (43.5%) | 53 (46.1%) | 0.688 | 0.424 | 0.791 | |
| Fibrates (n=114) | 4 (3.5%) | 6 (5.3%) | 8 (7%) | 0.748 | 0.375 | 0.784 | |
| Blood pressure-lowering drugs (n=115) | 63 (54.8%) | 64 (55.7%) | 65 (56.5%) | 1 | 0.894 | 1 | |
| Antiplatelet agents (n=114) | 27 (23.7%) | 32 (28.1%) | 29 (25.4%) | 0.545 | 0.878 | 0.765 | |
| Anthropometric parameters | |||||||
| Weight (n=109) | 81 [70–93.5] | 78 [68.5–88.5] | 78 [68.5–88.8] | <0.001 | <0.001 | 0.681 | 0.194 |
| BMI (n=108) | 29.6 [27.2–34.2] | 28.5 [26.2–32.5] | 28.8 [25.9–32.6] | <0.001 | <0.001 | 0.649 | 0.116 |
| Waist circumference (n=66) SD | 103.2±13.5 | 101.2±12.6 | 102.2±13 | <0.001 | <0.001 | 0.698 | 0.142 |
| SBP (n=107) SD | 130.6±13.5 | 130.3±14.3 | 129.4±14.4 | 0.690 | 0.592 | 0.303 | 0.762 |
| DBP (n=107) SD | 77.8±9 | 77.7±8.9 | 76.4±8.4 | 0.991 | 0.053 | 0.053 | 0.336 |
| Clinical characteristics | |||||||
| Smoking (%) (n=123) | 29 (23.6%) | 23/123 (18.7%) | 0.077 | ||||
| Alcohol (n=120) | 43 (35.8%) | 31/120 (25.8%) | 0.031 | ||||
| IPAQ test (n=96) | 0.002 | ||||||
| Low | 45 (46.9%) | 26/96 (27.1%) | |||||
| Moderate-high | 51 (53.1%) | 70/96 (72.9%) | |||||
| EuroQoL test (range 0–100) (n=78) | 7 [6–8] | 7.5 [6.6–8.9] | 0.003 | ||||
| Mediterranean diet test (range 0–14) (n=99) | 8.1±2 | 8.4±2 | 0.188 | ||||
SD: standard deviation; p for trend: trend analysis.
p-value <0.005.
There was also a moderate but significant reduction in weight and waist circumference (both p<0.001), as well as in alcohol consumption (p=0.031) and smoking (p=0.07), with increased physical activity (moderate-high: 53.1% at baseline versus 72.9% after 6 months; p=0.002) and improved subjective perception of health (70 at baseline versus 75 after 9 months; p=0.003) (Table 3).
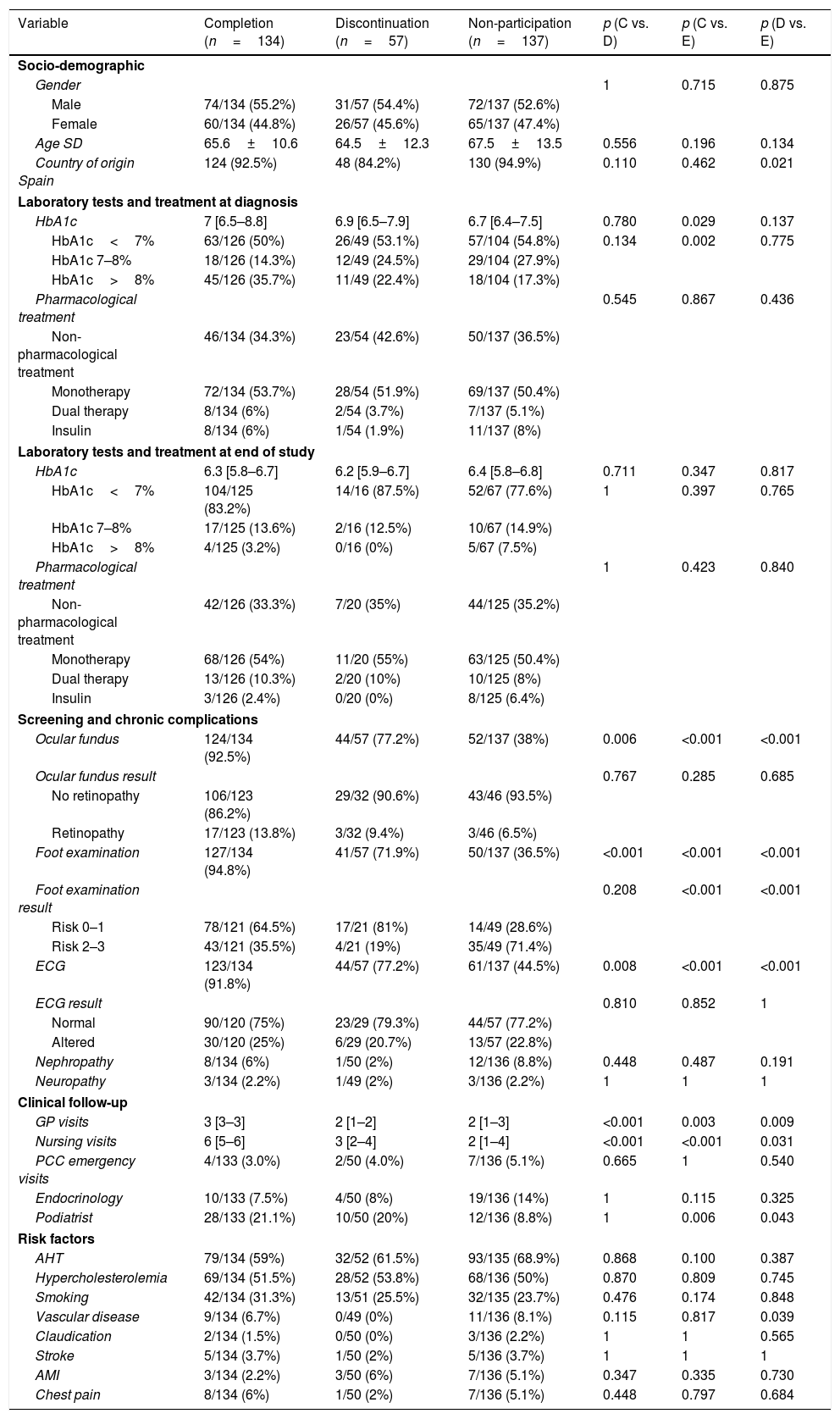
Comparison of patients who completed, who did not participate and who discontinued the programThe patients who discontinued the program once enrolled exhibited socio-demographic characteristics similar to those who completed the program or decided not to take part in it. The exception was country of origin, where a larger number of foreigners were found (15.8% discontinued the program, 7.5% completed it, and 5.1% did not participate) (Table 4). The non-participatory patients had lower HbA1c concentrations at diagnosis than those who completed the program (median 6.7% [IQR 6.4–7.5] versus 7% [IQR 6.5–8.8]; p=0.029).
Comparison of patients who completed the program, who discontinued the program, and who did not participate in the program.
| Variable | Completion (n=134) | Discontinuation (n=57) | Non-participation (n=137) | p (C vs. D) | p (C vs. E) | p (D vs. E) |
|---|---|---|---|---|---|---|
| Socio-demographic | ||||||
| Gender | 1 | 0.715 | 0.875 | |||
| Male | 74/134 (55.2%) | 31/57 (54.4%) | 72/137 (52.6%) | |||
| Female | 60/134 (44.8%) | 26/57 (45.6%) | 65/137 (47.4%) | |||
| Age SD | 65.6±10.6 | 64.5±12.3 | 67.5±13.5 | 0.556 | 0.196 | 0.134 |
| Country of origin Spain | 124 (92.5%) | 48 (84.2%) | 130 (94.9%) | 0.110 | 0.462 | 0.021 |
| Laboratory tests and treatment at diagnosis | ||||||
| HbA1c | 7 [6.5–8.8] | 6.9 [6.5–7.9] | 6.7 [6.4–7.5] | 0.780 | 0.029 | 0.137 |
| HbA1c<7% | 63/126 (50%) | 26/49 (53.1%) | 57/104 (54.8%) | 0.134 | 0.002 | 0.775 |
| HbA1c 7–8% | 18/126 (14.3%) | 12/49 (24.5%) | 29/104 (27.9%) | |||
| HbA1c>8% | 45/126 (35.7%) | 11/49 (22.4%) | 18/104 (17.3%) | |||
| Pharmacological treatment | 0.545 | 0.867 | 0.436 | |||
| Non-pharmacological treatment | 46/134 (34.3%) | 23/54 (42.6%) | 50/137 (36.5%) | |||
| Monotherapy | 72/134 (53.7%) | 28/54 (51.9%) | 69/137 (50.4%) | |||
| Dual therapy | 8/134 (6%) | 2/54 (3.7%) | 7/137 (5.1%) | |||
| Insulin | 8/134 (6%) | 1/54 (1.9%) | 11/137 (8%) | |||
| Laboratory tests and treatment at end of study | ||||||
| HbA1c | 6.3 [5.8–6.7] | 6.2 [5.9–6.7] | 6.4 [5.8–6.8] | 0.711 | 0.347 | 0.817 |
| HbA1c<7% | 104/125 (83.2%) | 14/16 (87.5%) | 52/67 (77.6%) | 1 | 0.397 | 0.765 |
| HbA1c 7–8% | 17/125 (13.6%) | 2/16 (12.5%) | 10/67 (14.9%) | |||
| HbA1c>8% | 4/125 (3.2%) | 0/16 (0%) | 5/67 (7.5%) | |||
| Pharmacological treatment | 1 | 0.423 | 0.840 | |||
| Non-pharmacological treatment | 42/126 (33.3%) | 7/20 (35%) | 44/125 (35.2%) | |||
| Monotherapy | 68/126 (54%) | 11/20 (55%) | 63/125 (50.4%) | |||
| Dual therapy | 13/126 (10.3%) | 2/20 (10%) | 10/125 (8%) | |||
| Insulin | 3/126 (2.4%) | 0/20 (0%) | 8/125 (6.4%) | |||
| Screening and chronic complications | ||||||
| Ocular fundus | 124/134 (92.5%) | 44/57 (77.2%) | 52/137 (38%) | 0.006 | <0.001 | <0.001 |
| Ocular fundus result | 0.767 | 0.285 | 0.685 | |||
| No retinopathy | 106/123 (86.2%) | 29/32 (90.6%) | 43/46 (93.5%) | |||
| Retinopathy | 17/123 (13.8%) | 3/32 (9.4%) | 3/46 (6.5%) | |||
| Foot examination | 127/134 (94.8%) | 41/57 (71.9%) | 50/137 (36.5%) | <0.001 | <0.001 | <0.001 |
| Foot examination result | 0.208 | <0.001 | <0.001 | |||
| Risk 0–1 | 78/121 (64.5%) | 17/21 (81%) | 14/49 (28.6%) | |||
| Risk 2–3 | 43/121 (35.5%) | 4/21 (19%) | 35/49 (71.4%) | |||
| ECG | 123/134 (91.8%) | 44/57 (77.2%) | 61/137 (44.5%) | 0.008 | <0.001 | <0.001 |
| ECG result | 0.810 | 0.852 | 1 | |||
| Normal | 90/120 (75%) | 23/29 (79.3%) | 44/57 (77.2%) | |||
| Altered | 30/120 (25%) | 6/29 (20.7%) | 13/57 (22.8%) | |||
| Nephropathy | 8/134 (6%) | 1/50 (2%) | 12/136 (8.8%) | 0.448 | 0.487 | 0.191 |
| Neuropathy | 3/134 (2.2%) | 1/49 (2%) | 3/136 (2.2%) | 1 | 1 | 1 |
| Clinical follow-up | ||||||
| GP visits | 3 [3–3] | 2 [1–2] | 2 [1–3] | <0.001 | 0.003 | 0.009 |
| Nursing visits | 6 [5–6] | 3 [2–4] | 2 [1–4] | <0.001 | <0.001 | 0.031 |
| PCC emergency visits | 4/133 (3.0%) | 2/50 (4.0%) | 7/136 (5.1%) | 0.665 | 1 | 0.540 |
| Endocrinology | 10/133 (7.5%) | 4/50 (8%) | 19/136 (14%) | 1 | 0.115 | 0.325 |
| Podiatrist | 28/133 (21.1%) | 10/50 (20%) | 12/136 (8.8%) | 1 | 0.006 | 0.043 |
| Risk factors | ||||||
| AHT | 79/134 (59%) | 32/52 (61.5%) | 93/135 (68.9%) | 0.868 | 0.100 | 0.387 |
| Hypercholesterolemia | 69/134 (51.5%) | 28/52 (53.8%) | 68/136 (50%) | 0.870 | 0.809 | 0.745 |
| Smoking | 42/134 (31.3%) | 13/51 (25.5%) | 32/135 (23.7%) | 0.476 | 0.174 | 0.848 |
| Vascular disease | 9/134 (6.7%) | 0/49 (0%) | 11/136 (8.1%) | 0.115 | 0.817 | 0.039 |
| Claudication | 2/134 (1.5%) | 0/50 (0%) | 3/136 (2.2%) | 1 | 1 | 0.565 |
| Stroke | 5/134 (3.7%) | 1/50 (2%) | 5/136 (3.7%) | 1 | 1 | 1 |
| AMI | 3/134 (2.2%) | 3/50 (6%) | 7/136 (5.1%) | 0.347 | 0.335 | 0.730 |
| Chest pain | 8/134 (6%) | 1/50 (2%) | 7/136 (5.1%) | 0.448 | 0.797 | 0.684 |
D: discontinuation, SD: standard deviation; E: excluded; C: completed.
p-value<0.005.
Screening for chronic complications was made in most patients who completed the program (retinopathy 92.5%, foot examination 94.8% and electrocardiogram 91.8%) and in a large proportion (approximately 75%) of those who discontinued the program before 6 months. However, screening was significantly less prevalent among those who did not take part in the program (retinopathy 38%, foot examination 36.5% and electrocardiogram in 44.5%). There were fewer podiatrist referrals (8.8%) among these patients as compared to those who completed (21.1%) or left the program (20.0%). As regards the cardiovascular risk factors, no differences were seen among the three groups, except for a larger number of patients with vascular disease in the non-participatory group (Table 4).
Visits to hospital emergency departments because of diabetes were more common in patients not in the program (4.4% versus 1.1% in the included patients; p=0.023), and these required more hospital admissions due to diabetes (4.5% versus 0% in the included patients).
DiscussionThe present study describes the results of one of the few structured initiatives conducted in Spain aimed at the care and education of patients with diabetes at a moment in time of the disease that may condition its future course. Clinical implementation and the educational methodology used are supported by previous high-evidence studies such as the DESMOND Newly Diagnosed program or the Romeo study,14,25 where group therapeutic education constitutes the central element. Scientific evidence has shown that therapeutic education programs with group interventions effectively favor patient capacity for action and are more likely to positively modify health behavior as the ultimate goal of such education.11,13,26 The training methodology allows the primary care professionals to optimize the program and group education in the different centers. Their participation has contributed to the continuity of this project, establishing functional dynamics among the professionals.
The program standardizes educational content, thereby promoting equity in health. Furthermore, it does not consume additional resources, but only rearranges those already available in the public health system. The patients have a very positive impression of the project, and the results obtained are favorable from the clinical and educational viewpoints.
The data obtained demonstrate the reality of a late clinical diagnosis of the disease (HbA1c>8% in 32% of the patients) and the presence of chronic complications at this time (13% retinopathy, 20% microalbuminuria 20mg/l). Strategies for identifying subjects at risk based on clinical scales27; a shortening of the time elapsed before diagnostic values are confirmed; or the adoption of the oral glucose tolerance test (used in only one of the participants in this study) as a diagnostic tool, could reduce the presence of chronic complications from the time of the clinical diagnosis of the disease. In addition, an early diagnosis could facilitate the start of patient self-care through programs such as that described herein. The screening of complications in the patients included in the program was more prevalent than the average among the population with diabetes in Catalonia during the study period (retinography in 87.4% versus 49%, foot examination in 88% versus 64.2%), this representing an advance in quality objectives in diabetes control.28–30
The program has demonstrated that the protocols of the clinical information compilation systems we have worked with do not allow us to record the variables of the diabetes education process required at the initial and subsequent evaluation of the patient, i.e., diet, physical activity, adherence, knowledge. However, all of them were collected for adequate evaluation of the program, and allowed the professionals to identify and improve shortcomings in a more efficient manner. In addition, given the importance of the early stages of the disease, we feel that these systems should consider certain variables that need to be assessed in a standardized manner (family history of diabetes or cardiovascular disease, dietary or activity habits, initial screening of complications, etc.). This would help in planning preventive strategies, facilitate information and therapeutic education in newly diagnosed cases, and encourage professionals to implement the program, thereby avoiding the weak impact of simple advice on its own.
Our study has some limitations. There were differences among the different centers in terms of the inclusion, number, and type of patients, responding to different healthcare, social, work dynamics and team involvement circumstances. The program promotes a change in standard care warranted by the solid evidence supporting its application within the target population (the onset of diabetes) and based on the methodology used (the standardization of processes and individual and group therapeutic education). It does not therefore represent a study in itself. The data collected retrospectively in our article seek to report the outcomes of this change in healthcare practice on the one hand, and to improve the quality of the program through the analysis of results on the other. In the same way as in other clinical programs conducted in our public health system, the fact that the patients may or may not follow the program shows that the program has not been implemented in a high percentage of subjects (67% of the total taking into consideration those patients not invited, as well as those who chose not to participate and those who dropped out). We do not know what these figures may be in prior care practice. This does not imply that such patients do not receive care, but indicates that care is provided as it was before the program was introduced.
It should also be noted that the results of the educational program cannot be extrapolated to probably more frail patients (advanced age, dependence, comorbidity) or individuals undergoing home follow-up or who are less adherent to public health monitoring.
The collection of information referring to certain variables was not complete in all individuals, as is seen in the different tables, since this is a program implemented on a pragmatic basis by primary care professionals in the context of routine clinical practice.
In sum, in clinical terms a high percentage of the professionals applied the recommendations established by treatment algorithms in DM2. The trajectory of the program has facilitated the screening of chronic complications in most patients. The results obtained are also in line with those recently published by the DESMOND Newly Diagnosed program,31 with a statistically significant improvement of metabolic control (HbA1c decrease of 0.9%) after 6 months. Likewise, the intervention has led to lifestyle changes such as increased physical activity, and decreased smoking and alcohol consumption. However, we have not seen significant changes in adherence to the Mediterranean diet, with figures remaining in the middle upper range. This may have been because adherence to the Mediterranean diet is already common among the population of this age, and because the efforts led by the nursing professionals to promote further changes in adherence to this diet was only strengthened following publication of the PREDIMED study in April 2013, when this program had already been launched.
As commented above, the present program implies a change in healthcare practice. Before implementation of the program we were unaware of the level of knowledge acquired by patients at disease onset. We therefore aimed to determine whether knowledge about diabetes (already acquired by the patient or obtained during the educational program) was adequate for coping with this chronic disease. In this way, we could evaluate whether certain aspects of the program needed to be reinforced. We believe that the educational outcomes of the program are optimal in the sense that we standardize education and thus control quality content. In addition, the level of knowledge and therapeutic adherence of the patients at the end of the initiative proved adequate, and better than among the patients who only received the individualized measures. The patients were highly satisfied with the most important part of the educational program: group education.
The care burden in the PCCs did not increase, and the visits contemplated by the program were met, thus probably helping to reduce the need for hospital based care. By contrast, the patients who did not participate were associated with greater hospital based care requirements (emergencies, admissions) both in general and related to diabetes.
ConclusionBased on the results obtained, it may be concluded that patients enrolled in the PAET-Debut DM2 achieve improved metabolic control and control of cardiovascular risk factors, including the lipid profile, with a likewise significant decrease in the BMI and waist circumference. In addition, the program induces lifestyle changes, leading patients to increase their physical activity, and improves their perceived quality of life. The percentage of patients systematically screened for chronic complications was also improved. In addition, the patients that underwent group therapeutic education within the program obtained a better level of knowledge about diabetes, with improved treatment adherence, compared with those who only received the intervention at an individual level. The implementation of the program required no increased use of healthcare resources, but did require modification of the healthcare model.
Practical implications: given the overall good results obtained in patients who completed the PAET-Debut DM2, and considering a population-based public health approach, work is needed to promote patient inclusion or to determine which alternative follow-up should be performed beyond the existing routine clinical practice and inertia at this stage of the disease.
The implementation of new strategies to consolidate the program, and confidence among the professionals in the results obtained, has made it possible to modify practices in the different centers. At the time of writing our document, this initial effort has allowed the PAET-DebutDM2 program to become standard practice in the first four participating sites. The initiative moreover has been extended to over 9 centers within the AISBE, and represents the new model for unifying and standardizing care and therapeutic education in patients with newly diagnosed type 2 diabetes.
Financial supportThis project received funding from the Catalan Diabetes Association (Asociación Catalana de Diabetes [ACD]), with the awarding of Aid to Research in Therapeutic Education in Diabetes (call of 2013).
Conflicts of interestThe authors declare that they have no conflicts of interest.
Thanks are due to the institutional members who have supported the project: Dr. Belén Enfedaque, Care Director of the Ámbito de Atención Primaria Barcelona Ciudad of the Instituto Catalán de la Salud; Dr. Jaume Benavent, Manager of the Primary Care Center Salud Barcelona Esquerra; Dr. Josep Vidal, Director of the ICMDM of the Hospital Clínico; the strategic management of the Área Integral de Salud «Barcelona Esquerra»; the team Directors of the primary care centers; the program reference professionals; the professionals of the primary care centers participating in the project; and Belchin Kostov, for support in the statistical analysis of the project.
We also thank the company Ascensia Diabetes Care for its collaboration in providing the primary care centers with educational material, and Laboratorios Esteve for supplying educational material from the Fundación Alicia. Both types of material served as support in therapeutic education referring to the diet plan.
Please cite this article as: Colungo C, Liroz M, Jansà M, Blat E, Herranz MC, Vidal M, et al. Programa de atención y educación terapéutica en el debut de la diabetes tipo 2: un nuevo modelo de abordaje en atención primaria. Endocrinol Diabetes Nutr. 2018;65:486–499.





![Trajectory of the Healthcare and Therapeutic Education Program for newly diagnosed type 2 diabetes (Programa de Atención y Educación Terapéutica en el debut de la DM2 [PAET-Debut DM2]). Trajectory of the Healthcare and Therapeutic Education Program for newly diagnosed type 2 diabetes (Programa de Atención y Educación Terapéutica en el debut de la DM2 [PAET-Debut DM2]).](https://static.elsevier.es/multimedia/25300180/0000006500000009/v1_201811240700/S2530018018301379/v1_201811240700/en/main.assets/thumbnail/gr1.jpeg?xkr=ue/ImdikoIMrsJoerZ+w96p5LBcBpyJTqfwgorxm+Ow=)
![Flow of participants in the pilot Healthcare and Therapeutic Education Program for newly diagnosed type 2 diabetes (Programa de Atención y Educación Terapéutica en el debut de la DM2 [PAET-Debut DM2]). Flow of participants in the pilot Healthcare and Therapeutic Education Program for newly diagnosed type 2 diabetes (Programa de Atención y Educación Terapéutica en el debut de la DM2 [PAET-Debut DM2]).](https://static.elsevier.es/multimedia/25300180/0000006500000009/v1_201811240700/S2530018018301379/v1_201811240700/en/main.assets/thumbnail/gr2.jpeg?xkr=ue/ImdikoIMrsJoerZ+w96p5LBcBpyJTqfwgorxm+Ow=)