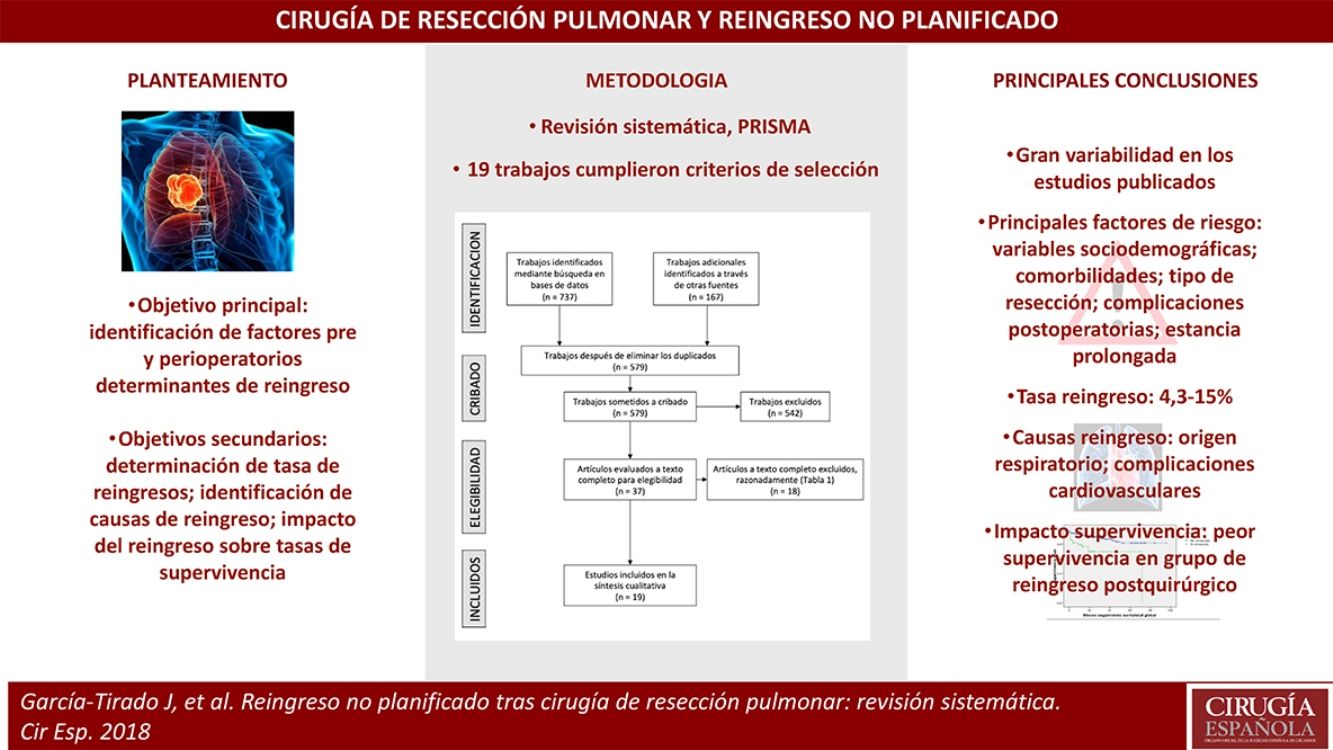
Urgent readmissions have a major impact on outcomes in patient health and healthcare costs. The associated risk factors have generally been infrequently studied. The main objective of the present work is to identify pre- and perioperative determinants of readmission; the secondary aim was to determine readmission rate, identification of readmission diagnoses, and impact of readmissions on survival rates in related analytical studies.
The review was performed through a systematic search in the main bibliographic databases. In the end, 19 papers met the selection criteria.
The main risk factors were: sociodemographic patient variables; comorbidities; type of resection; postoperative complications; long stay.
Despite the great variability in the published studies, all highlight the importance of reducing readmission rates because of the significant impact on patients and the healthcare system.
Los reingresos urgentes suponen un impacto importante sobre los resultados en la salud de los pacientes y los costes sanitarios. Los factores de riesgo asociados a reingreso tras cirugía de resección pulmonar han sido poco estudiados. El principal objetivo del presente trabajo es la identificación de factores pre- y perioperatorios determinantes de reingreso; secundariamente, determinación de tasa de reingresos, identificación de diagnósticos de reingreso, e impacto de los reingresos sobre las tasas de supervivencia en los estudios que lo analizaban.
La revisión se realizó mediante búsqueda sistemática en las principales bases de datos bibliográficas. Finalmente, 19 trabajos cumplieron los criterios de selección.
Los principales factores de riesgo fueron: variables sociodemográficas de los pacientes; comorbilidades; tipo de resección; complicaciones postoperatorias; estancia prolongada.
A pesar de la gran variabilidad en los estudios publicados, todos destacan la importancia de reducir los índices de reingreso por su significativo impacto sobre pacientes y sistema sanitario.
The Quality Plan of our National Healthcare System contemplates the rate of readmission after surgical procedures as a relevant marker of care quality.1 The adjusted rates of potentially avoidable readmissions are sufficiently solid to justify their inclusion to monitor hospital quality2,3; a high rate of readmissions could indicate inadequate care, with poor care results and a loss of efficiency.4 Thus, avoidable readmissions are estimated as an indirect indicator of quality and are assumedly an opportunity for significant savings in potential costs for the healthcare system,5 while also recognizing their impact on patient health outcomes, both in terms of quality of life as well as survival.6
Several studies have been published about readmissions after various surgical procedures in general, trauma and cardiovascular surgery; meanwhile, other studies have grouped together different major surgeries from different specialties, including pulmonary lobectomy.6,7 However, the specific risk factors associated with readmission, the rate of readmissions and their correlating diagnoses after lung resection surgery have generally not been extensively studied. Recently, several papers have been published analyzing readmissions after lung resection surgery. The main objective of this study is to identify pre- and perioperative determinants for readmission. Secondary objectives were to analyze readmission rates, identify the diagnoses associated with readmission, and calculate the impact of readmissions on survival rates in the studies that analyzed this variable.
MethodsThe review was carried out following the guidelines of the Preferred Reporting Items For Systematic Reviews and Meta-Analyses (PRISMA)8 in order to answer the following questions: what is the readmission rate in lung resection surgery?; what are the diagnoses of the patients who are readmitted after a pulmonary resection?; and, is it possible to identify perioperative risk factors predicting readmission? The review protocol was registered in the International Prospective Register of Systematic Reviews (PROSPERO),9 under record number CRD42017059341.
Search StrategyThe search was carried out until March 2017 in five bibliographic databases (PubMed, US National Library of Medicine-National Institute of Health; Embase, Elsevier; The Cochrane Library and Cochrane Library Plus, Cochrane Collaboration; Spanish Bibliographic Index in the Health Sciences (IBECS); Virtual Health Library (BVS), Carlos III Health Institute), and an additional search was conducted in Tripdatabase and Google Scholar.
The search terms in Spanish were “readmisión” and “cirugía”, as well as “readmission” and “lung surgery” in English. The searches excluded “transplants” and were limited to studies in humans, with no time restriction.
Inclusion and Exclusion CriteriaThe scope of the study was readmission after lung resection surgery in human adults. Therefore, the inclusion criteria were studies conducted on unplanned readmissions in adult humans (18 and older) who had undergone pulmonary resection surgery (any technique). We excluded the studies about readmission in thoracic surgery focused on other types of surgical interventions other than lung resections, as well as studies in which readmission was not the main objective of the study but was used as an indicator of quality to evaluate certain programs or was used in the comparison of results between different hospital teams.
All article types were included, excluding editorials, letters to the editor or redundant papers.
Measurement of ResultsThe main result of interest was the identification of pre- and perioperative factors that led to readmission.
The secondary outcomes were the rate of unplanned readmissions after lung resection surgery and the readmission diagnoses. Another result assessed was the influence of readmissions on survival rates, although not all the studies analyzed this variable.
Study Selection; Data ExtractionStudy titles and/or abstracts were retrieved by applying the search strategy in the different bibliographic databases consulted; these were then examined independently by two authors of the review (GT and LO). The full texts of these potentially eligible studies were obtained and evaluated independently by two members of the review team (GT and LO). Any disagreement was resolved through discussion with a third reviewer (MB). A standardized form was used to extract the data from the included studies, and two reviewers extracted data independently (GT and JL); any discrepancies were resolved by discussion with a third author (MB).
Quality Assessment (Risk of Bias)The methodological quality of the studies was assessed independently by two researchers (JL and MB) using the Cochrane Collaboration10 bias risk assessment tool. Using this tool, we evaluated: selection bias (patient inclusion criteria, including losses and exclusions from the analysis, reporting the reasons for these losses and exclusions); detection bias (establishing the criteria for identifying the main event: readmission); attrition (identifying the sources for obtaining the data, with possible bias due to quantity, nature or incomplete data management); information bias (possible selectively reported results); and other biases (any important observation of possible unforeseen biases). Possible disagreements were resolved with the participation of a third review author (GT).
Data AnalysisGiven the heterogeneity in the data analysis, a narrative synthesis was undertaken of the results from the studies analyzed (data from heterogeneous studies grouped into a meta-analysis can produce erroneous results).11
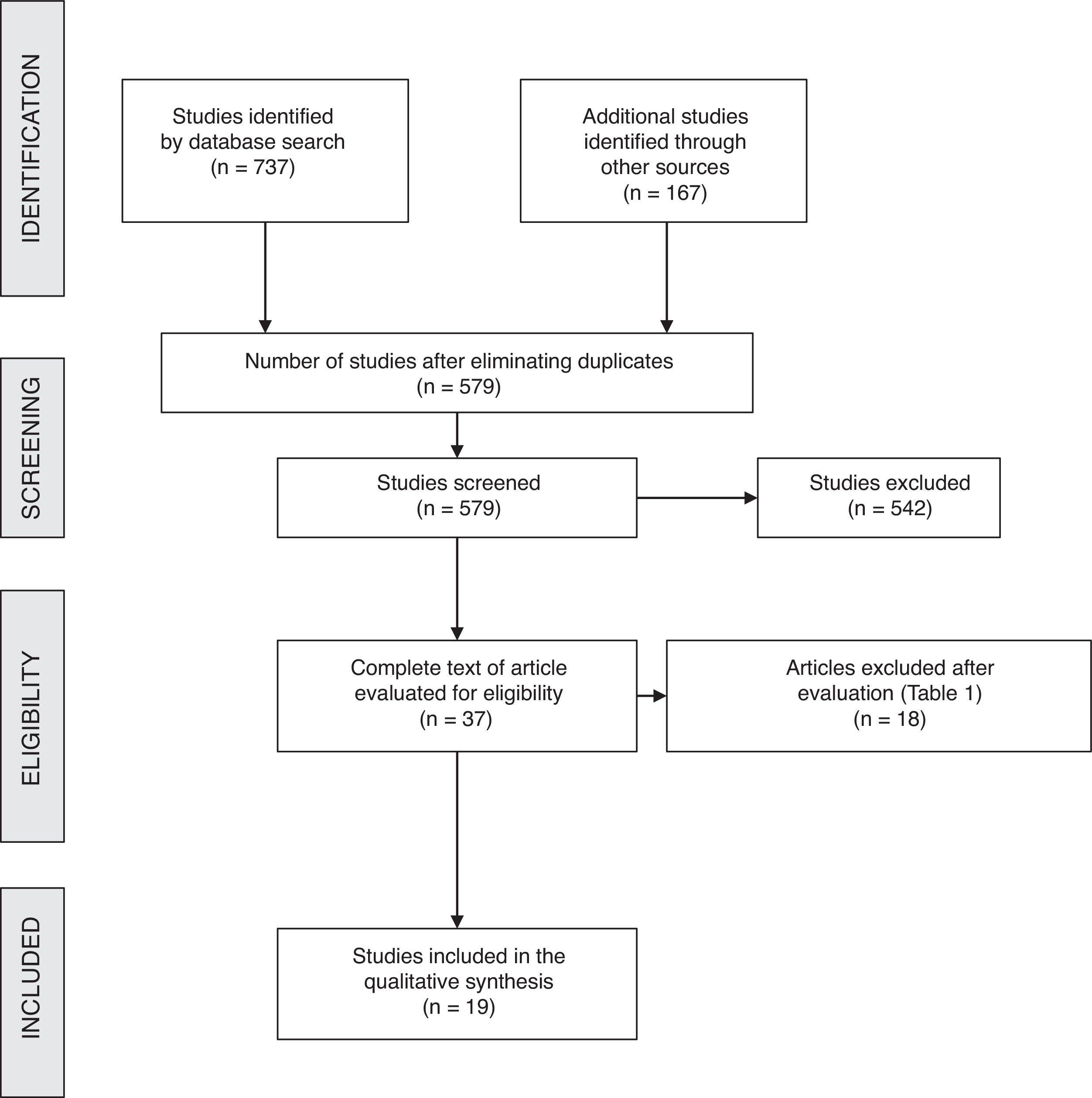
ResultsBibliographic SearchAfter filtering and eliminating duplicates of the 904 papers initially identified, 579 articles were obtained (Fig. 1). In the end, the full texts of 37 articles were reviewed, 18 of which were excluded for different reasons (Table 1). Thus, 19 studies met the selection criteria and were included in the review.5–7,12–27
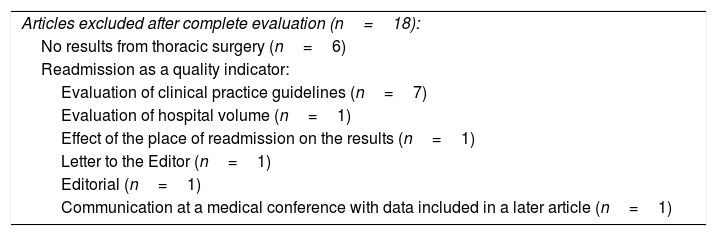
Reasons for exclusion of eligible articles after evaluation of the complete text.
| Articles excluded after complete evaluation (n=18): |
| No results from thoracic surgery (n=6) |
| Readmission as a quality indicator: |
| Evaluation of clinical practice guidelines (n=7) |
| Evaluation of hospital volume (n=1) |
| Effect of the place of readmission on the results (n=1) |
| Letter to the Editor (n=1) |
| Editorial (n=1) |
| Communication at a medical conference with data included in a later article (n=1) |
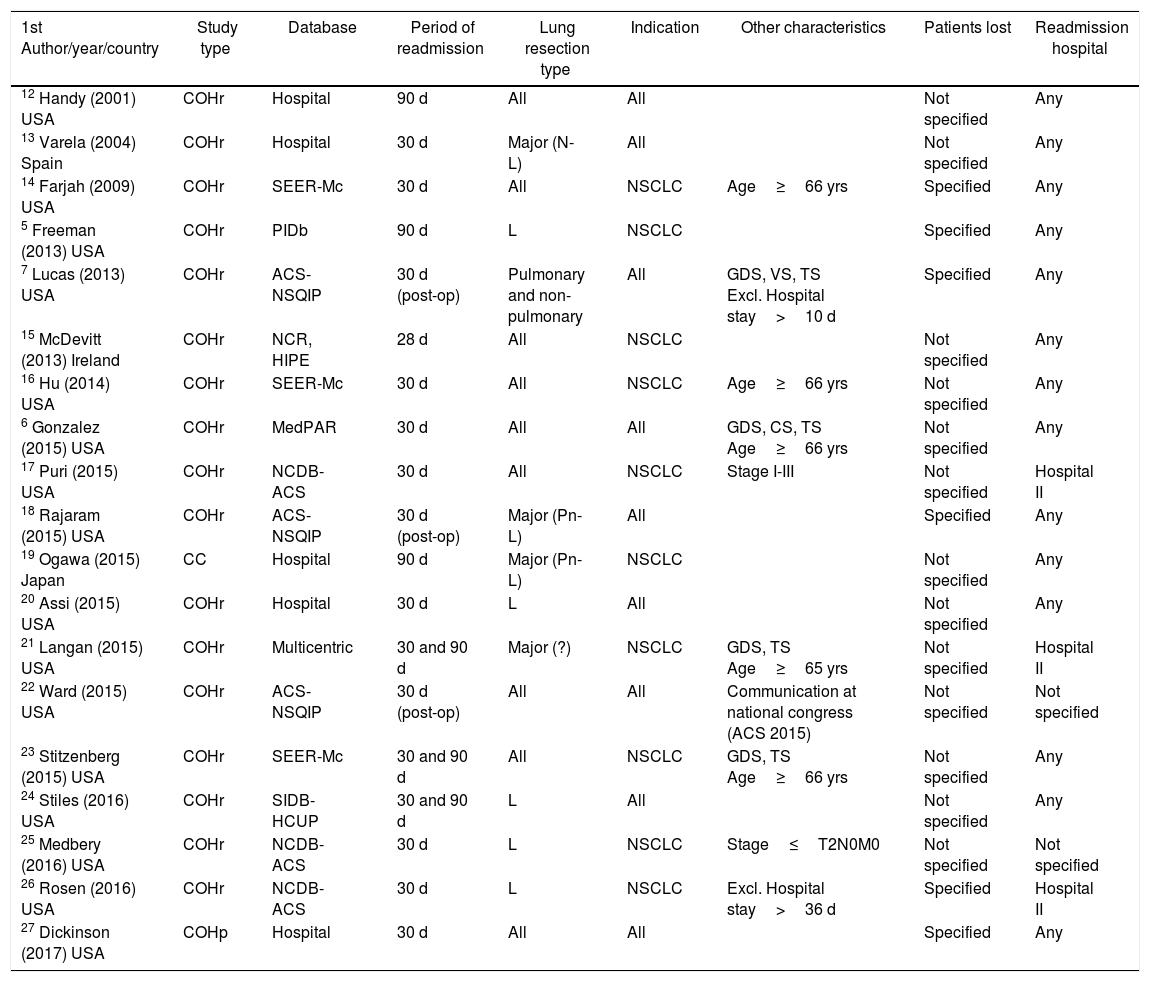
All the studies analyzed presented a retrospective cohort design, with the exception of one case–control study19 and one prospective cohort study with a one-year follow-up.27 One retrospective cohort study had been published as a communication at a national congress.22Table 2 shows the main characteristics of the study designs.
Main Characteristics Regarding the Design of the Studies.
| 1st Author/year/country | Study type | Database | Period of readmission | Lung resection type | Indication | Other characteristics | Patients lost | Readmission hospital |
|---|---|---|---|---|---|---|---|---|
| 12 Handy (2001) USA | COHr | Hospital | 90 d | All | All | Not specified | Any | |
| 13 Varela (2004) Spain | COHr | Hospital | 30 d | Major (N-L) | All | Not specified | Any | |
| 14 Farjah (2009) USA | COHr | SEER-Mc | 30 d | All | NSCLC | Age≥66 yrs | Specified | Any |
| 5 Freeman (2013) USA | COHr | PIDb | 90 d | L | NSCLC | Specified | Any | |
| 7 Lucas (2013) USA | COHr | ACS-NSQIP | 30 d (post-op) | Pulmonary and non-pulmonary | All | GDS, VS, TS Excl. Hospital stay>10 d | Specified | Any |
| 15 McDevitt (2013) Ireland | COHr | NCR, HIPE | 28 d | All | NSCLC | Not specified | Any | |
| 16 Hu (2014) USA | COHr | SEER-Mc | 30 d | All | NSCLC | Age≥66 yrs | Not specified | Any |
| 6 Gonzalez (2015) USA | COHr | MedPAR | 30 d | All | All | GDS, CS, TS Age≥66 yrs | Not specified | Any |
| 17 Puri (2015) USA | COHr | NCDB-ACS | 30 d | All | NSCLC | Stage I-III | Not specified | Hospital II |
| 18 Rajaram (2015) USA | COHr | ACS-NSQIP | 30 d (post-op) | Major (Pn-L) | All | Specified | Any | |
| 19 Ogawa (2015) Japan | CC | Hospital | 90 d | Major (Pn-L) | NSCLC | Not specified | Any | |
| 20 Assi (2015) USA | COHr | Hospital | 30 d | L | All | Not specified | Any | |
| 21 Langan (2015) USA | COHr | Multicentric | 30 and 90 d | Major (?) | NSCLC | GDS, TS Age≥65 yrs | Not specified | Hospital II |
| 22 Ward (2015) USA | COHr | ACS-NSQIP | 30 d (post-op) | All | All | Communication at national congress (ACS 2015) | Not specified | Not specified |
| 23 Stitzenberg (2015) USA | COHr | SEER-Mc | 30 and 90 d | All | NSCLC | GDS, TS Age≥66 yrs | Not specified | Any |
| 24 Stiles (2016) USA | COHr | SIDB-HCUP | 30 and 90 d | L | All | Not specified | Any | |
| 25 Medbery (2016) USA | COHr | NCDB-ACS | 30 d | L | NSCLC | Stage≤T2N0M0 | Not specified | Not specified |
| 26 Rosen (2016) USA | COHr | NCDB-ACS | 30 d | L | NSCLC | Excl. Hospital stay>36 d | Specified | Hospital II |
| 27 Dickinson (2017) USA | COHp | Hospital | 30 d | All | All | Specified | Any |
The corresponding bibliographic reference appears with each author.
yrs: years; ACS-NSQIP: American College of Surgeons-National Surgical Quality Improvement Program; NSCLC: non-small cell lung cancer; CC: case–control; GDS: general and digestive surgery; COHp: cohort, prospective; COHr: cohort, retrospective; TS: thoracic surgery; VS: vascular surgery; CS: cardiac surgery; d: days; Excl.: excluded; HIPE: Hospital In-Patient Enquiry; L: lobectomy; MedPAR: Medicare Provider Analysis and Review; Pn: pneumonectomy; NCDB-ACS: National Cancer Data Base- American College of Surgeons and American Cancer Society; NCR: National Cancer Registry; PIDb: Premier Inpatient Database; SEER-Mc: Surveillance, Epidemiology and End Results-Medicare; SIDB-HCUP: State Inpatient Database-Healthcare Cost and Utilization Project; ?: not defined; II: admission rate
In many studies, recruitment was from large databases, some from a hospital setting12,13,19,20,27 and one was a multicenter study.21 Significant variability was observed in the type of lung resection included in the studies, as well as in the indications for lung resection, being restricted to patients with bronchogenic carcinoma in many cases, or to all types of indications in many others. The criterion of readmission was established in the majority of the studies as that occurring during the 30 days following patient discharge after the initial admission, while in other studies a 90-day period was established5,12,19 and in some cases the 30-day period was established after surgery7,18,22; in yet another study, the limit was 28 days,15 and two authors carried out the study with 30- and 90-day periods after hospital discharge.21,23,24
The study design profiles reveal the main biases that could be derived from patient selection: several studies restricted patient age (including patients over 6521 or 666,14,16,23); others excluded patients who had prolonged hospital stays for a certain period after admission7,26; some articles were very large population studies that included different types of surgery, including abdominal,6,7,21,23 vascular7 or cardiac,6 although they provided detailed readmission information in thoracic surgery, fulfilling the criteria for inclusion in the review.
Another potential source of bias was the possible incomplete collection of data and their selective reporting: only six of the studies made specific mention of the loss of patients5,7,14,18,26,27; and, regarding the readmitting hospital, two studies did not specify whether the possibility of readmission at a different hospital had been considered,22,25 and three papers collected only the readmissions at the hospital where the initial admission had occurred.17,21,26
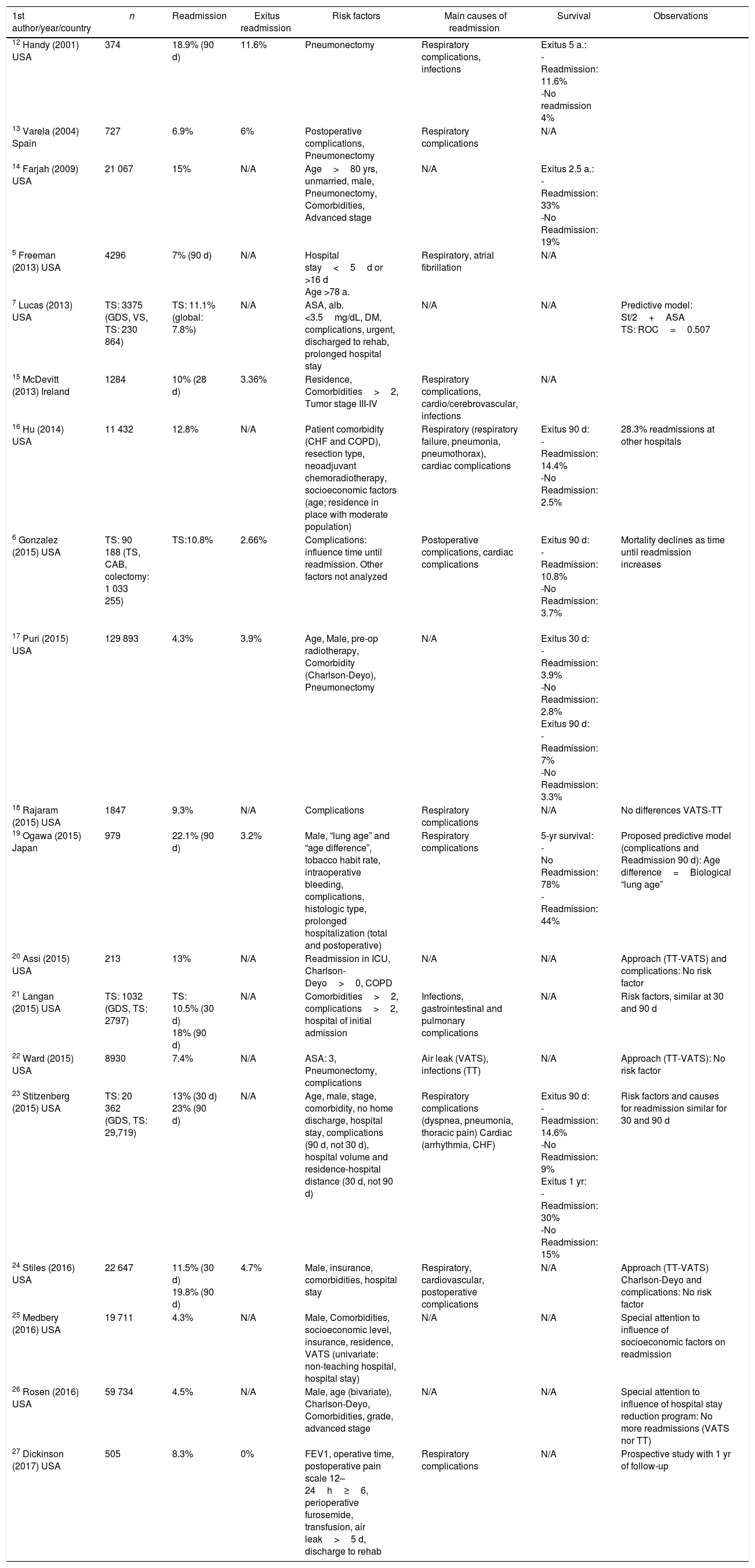
Readmission RatesThe rate of readmissions within 30 days ranged between 4.3%17,25 and 15%,14 including the studies that established a criterion of 28 days after discharge15 and 30 days after surgery.7,18,22 The articles that analyzed readmission within 90 days obtained a rate that ranged between 7%5 and 23%23; excluding the study at the lower end of the range,5 all the other 90-day studies placed the readmission rate above 18%. The only study done in Spain that met the inclusion criteria of this study (Varela et al.,13 2004) reported a readmission rate of 6.9%.
Risk Factors Associated With ReadmissionTable 3 provides a synopsis of the main results found by the different authors; Table 4 demonstrates the complete list of variables analyzed in the different studies, providing details about those that were significant for the different authors with their statistical result, and Table 5 schematically reflects the risk factors leading to readmission.
Studies about readmission after lung resection surgery, with a synopsis of the main results presented.
| 1st author/year/country | n | Readmission | Exitus readmission | Risk factors | Main causes of readmission | Survival | Observations |
|---|---|---|---|---|---|---|---|
| 12 Handy (2001) USA | 374 | 18.9% (90 d) | 11.6% | Pneumonectomy | Respiratory complications, infections | Exitus 5 a.: -Readmission: 11.6% -No readmission 4% | |
| 13 Varela (2004) Spain | 727 | 6.9% | 6% | Postoperative complications, Pneumonectomy | Respiratory complications | N/A | |
| 14 Farjah (2009) USA | 21 067 | 15% | N/A | Age>80 yrs, unmarried, male, Pneumonectomy, Comorbidities, Advanced stage | N/A | Exitus 2.5 a.: -Readmission: 33% -No Readmission: 19% | |
| 5 Freeman (2013) USA | 4296 | 7% (90 d) | N/A | Hospital stay<5d or >16 d Age >78 a. | Respiratory, atrial fibrillation | N/A | |
| 7 Lucas (2013) USA | TS: 3375 (GDS, VS, TS: 230 864) | TS: 11.1% (global: 7.8%) | N/A | ASA, alb. <3.5mg/dL, DM, complications, urgent, discharged to rehab, prolonged hospital stay | N/A | N/A | Predictive model: St/2+ASA TS: ROC=0.507 |
| 15 McDevitt (2013) Ireland | 1284 | 10% (28 d) | 3.36% | Residence, Comorbidities>2, Tumor stage III-IV | Respiratory complications, cardio/cerebrovascular, infections | N/A | |
| 16 Hu (2014) USA | 11 432 | 12.8% | N/A | Patient comorbidity (CHF and COPD), resection type, neoadjuvant chemoradiotherapy, socioeconomic factors (age; residence in place with moderate population) | Respiratory (respiratory failure, pneumonia, pneumothorax), cardiac complications | Exitus 90 d: -Readmission: 14.4% -No Readmission: 2.5% | 28.3% readmissions at other hospitals |
| 6 Gonzalez (2015) USA | TS: 90 188 (TS, CAB, colectomy: 1 033 255) | TS:10.8% | 2.66% | Complications: influence time until readmission. Other factors not analyzed | Postoperative complications, cardiac complications | Exitus 90 d: -Readmission: 10.8% -No Readmission: 3.7% | Mortality declines as time until readmission increases |
| 17 Puri (2015) USA | 129 893 | 4.3% | 3.9% | Age, Male, pre-op radiotherapy, Comorbidity (Charlson-Deyo), Pneumonectomy | N/A | Exitus 30 d: -Readmission: 3.9% -No Readmission: 2.8% Exitus 90 d: -Readmission: 7% -No Readmission: 3.3% | |
| 18 Rajaram (2015) USA | 1847 | 9.3% | N/A | Complications | Respiratory complications | N/A | No differences VATS-TT |
| 19 Ogawa (2015) Japan | 979 | 22.1% (90 d) | 3.2% | Male, “lung age” and “age difference”, tobacco habit rate, intraoperative bleeding, complications, histologic type, prolonged hospitalization (total and postoperative) | Respiratory complications | 5-yr survival: - No Readmission: 78% -Readmission: 44% | Proposed predictive model (complications and Readmission 90 d): Age difference=Biological “lung age” |
| 20 Assi (2015) USA | 213 | 13% | N/A | Readmission in ICU, Charlson-Deyo>0, COPD | N/A | N/A | Approach (TT-VATS) and complications: No risk factor |
| 21 Langan (2015) USA | TS: 1032 (GDS, TS: 2797) | TS: 10.5% (30 d) 18% (90 d) | N/A | Comorbidities>2, complications>2, hospital of initial admission | Infections, gastrointestinal and pulmonary complications | N/A | Risk factors, similar at 30 and 90 d |
| 22 Ward (2015) USA | 8930 | 7.4% | N/A | ASA: 3, Pneumonectomy, complications | Air leak (VATS), infections (TT) | N/A | Approach (TT-VATS): No risk factor |
| 23 Stitzenberg (2015) USA | TS: 20 362 (GDS, TS: 29,719) | 13% (30 d) 23% (90 d) | N/A | Age, male, stage, comorbidity, no home discharge, hospital stay, complications (90 d, not 30 d), hospital volume and residence-hospital distance (30 d, not 90 d) | Respiratory complications (dyspnea, pneumonia, thoracic pain) Cardiac (arrhythmia, CHF) | Exitus 90 d: -Readmission: 14.6% -No Readmission: 9% Exitus 1 yr: -Readmission: 30% -No Readmission: 15% | Risk factors and causes for readmission similar for 30 and 90 d |
| 24 Stiles (2016) USA | 22 647 | 11.5% (30 d) 19.8% (90 d) | 4.7% | Male, insurance, comorbidities, hospital stay | Respiratory, cardiovascular, postoperative complications | N/A | Approach (TT-VATS) Charlson-Deyo and complications: No risk factor |
| 25 Medbery (2016) USA | 19 711 | 4.3% | N/A | Male, Comorbidities, socioeconomic level, insurance, residence, VATS (univariate: non-teaching hospital, hospital stay) | N/A | N/A | Special attention to influence of socioeconomic factors on readmission |
| 26 Rosen (2016) USA | 59 734 | 4.5% | N/A | Male, age (bivariate), Charlson-Deyo, Comorbidities, grade, advanced stage | N/A | N/A | Special attention to influence of hospital stay reduction program: No more readmissions (VATS nor TT) |
| 27 Dickinson (2017) USA | 505 | 8.3% | 0% | FEV1, operative time, postoperative pain scale 12–24h≥6, perioperative furosemide, transfusion, air leak>5 d, discharge to rehab | Respiratory complications | N/A | Prospective study with 1 yr of follow-up |
The corresponding bibliographic reference appears together with the author.
yrs: years; alb. albumin; ASA: American Society of Anesthesiologists; CAB: coronary artery bypass; c: C-statistic; GDS: general and digestive surgery; TS: thoracic surgery; VS: vascular surgery; d: days; DM: diabetes mellitus; Ex.Readmission: Exitus during readmission; n: sample size; FEV1: forced expiratory volume in one second; CHF: congestive heart failure; N/A: not analyzed; preop.: preoperative; ROC: Receiver Operating Characteristic curve; TT: thoracotomy; ICU: intensive care unit; VATS: video-assisted thoracoscopic surgery; vol.: volume.
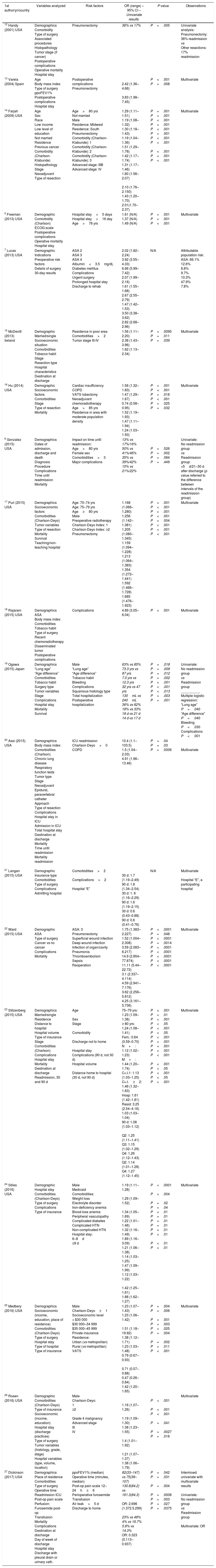
Variables analyzed in the different studies analyzed, showing those that were significant for the different authors in the multivariate analysis (or univariate if that was the resulted given) with OR values and corresponding p value for each significant variable.
| 1st author/yr/country | Variables analyzed | Risk factors | OR (range) – 95% CI – Univariate results | P value | Observations |
|---|---|---|---|---|---|
| 12 Handy (2001) USA | Demographics Comorbidity Type of surgery Associated procedures Histopathology Tumor stage (if cancer) Postoperative complications Operative mortality Hospital stay | Pneumonectomy | 36% vs 17% | P=.005 | Univariate analysis: Pneumonectomy: 36% readmission vs Other resections: 17% readmission |
| 13 Varela (2004) Spain | Age Body mass index Type of surgery ppoFEV1% Postoperative complications Hospital stay | Postoperative complications Pneumonectomy | 2.42 (1.36–4.66) 3.83 (1.98–7.45) | P<.001 P=.008 | Multivariate |
| 14 Farjah (2009) USA | Age Sex Race Low income Low level of education Not married Residence Previous cancer Comorbidity (Charlson-Klabunde) Histopathology Stage Neoadjuvant Type of resection | Age>80 yrs Not married Male Residence: Midwest Residence: South Pneumonectomy Comorbidity (Charlson-Klabunde): 1 Comorbidity (Charlson-Klabunde): 2 Comorbidity (Charlson-Klabunde): 3 Advanced stage: IIIB Advanced stage: IV | 1.29 (1.11–1.51) 1.19 (1.08–1.32) 1.30 (1.18–1.43) 1.19 (1.04–1.36) 1.51 (1.29–1.78) 1.42 (1.17–1.74) 1.31 (1.17–1.46) 1.80 (1.56–2.07) 2.10 (1.76–2.150) 1.43 (1.20–1.70) 2.01(1.70–2.37) | P=.001 P=.001 P<.001 P=.001 P<.001 P=.001 P<.001 P<.001 P<.001 P<.001 P<.001 | Multivariate |
| 5 Freeman (2013) USA | Demographic Comorbidity (Charlson) ECOG scale Postoperative complications Operative mortality Hospital stay | Hospital stay<5 days Hospital stay>16 day Age>78 yrs | 1.61 (N/A) 1.37 (N/A) 1.49 (N/A) | P=.001 P=.001 P<.001 | Multivariate |
| 7 Lucas (2013) USA | Demographic Indications Preoperative risk factors Details of surgery 30-day results | ASA 2 ASA 3 ASA 4 Albumin<3.5mg/dL Diabetes mellitus Complications Urgent surgery Prolonged hospital stay Discharge to rehab | 2.02 (1.82–2.24) 3.92 (3.55–4.33) 6.66 (5.99–7.42) 2.07 (1.99–2.16) 1.61 (1.55–1.68) 2.67 (2.55–2.79) 1.47 (1.42–1.53) 3.50 (3.38–3.62) 2.82 (2.68–2.96) | N/A | Attributable population risk: ASA: 66.1% 12.6% 8.8% 9.7% 10.3% 47.9% 7.8% |
| 15 McDevitt (2013) Ireland | Demographic Married/single Socioeconomic situation Comorbidities Tobacco habit Stage Resection type Hospital characteristics Destination at discharge | Residence in poor area Comorbidities>2 Tumor stage III-IV | 1.56 (1.11–2.20) 2.38 (1.43–3.96) 1.62 (1.13–2.34) | P=.0095 P=.011 P=.039 | Multivariate |
| 16 Hu (2014) USA | Demographic Socioeconomic factors Comorbidities Stage Type of resection Mortality | Cardiac insufficiency COPD VATS lobectomy Neoadjuvant chemoradiotherapy Age>85 yrs Residence in area with moderate population density | 1.56 (1.32–1.83) 1.47 (1.29–1.67) 0.74 (0.58–0.95) 1.52 (1.19–1.93) 1.47 (1.11–1.94) 1.24 (1.03–1.50) | P<.001 P<.001 P=.018 P<.001 P=.025 P=.032 | Multivariate |
| 6 Gonzalez (2015) USA | Demographics Dates of admission, discharge and death Diagnosis Procedure Complications Time until readmission Mortality | Impact on time until readmission: Age>80 yrs Female sex Comorbidities>3 Major complications | 13% vs 17%/16% 50% vs 41%/46% 35% vs 39%/42% 15% vs 21%/22% | P=.526 P=.002 P=.084 P=.449 | Univariate: No readmission group vs Readmission group: <5d/21–30 d after discharge (p value referred to the difference between intervals of the readmission group) |
| 17 Puri (2015) USA | Demographics Socioeconomic factors Comorbidities (Charlson-Deyo) Tumor variables Type of resection Mortality Survival Teaching/non-teaching hospital | Age: 70–74 yrs Age: 75–79 yrs Age≥80 yrs Male Preoperative radiotherapy Charlson-Deyo Index: 1 Charlson-Deyo Index: ≥2 Pneumonectomy | 1.168 (1.066–1.280) 1.256 (1.142–1.381) 1.205 (1.080–1.345) 1.159 (1.094–1.228) 1.213 (1.064–1.383) 1.354 (1.272–1.441) 1.592 (1.466–1.728) 1.685 (1.476–1.923) | P=.001 P<.001 P=.001 P<.001 P=.004 P<.001 P<.001 P<.001 | Multivariate |
| 18 Rajaram (2015) USA | Demographics ASA Body mass index Comorbidities Tobacco habit Type of surgery Recent chemoradiotherapy Disseminated tumor Postoperative complications | Complications | 4.89 (3.05–6.04) | P<.001 | Multivariate |
| 19 Ogawa (2015) Japan | Demographics “Lung age” “Age difference” Comorbidities Tobacco habit Surgery type Tumor variables Stage Complications Hospital stay Mortality Survival | Male “Lung age” “Age difference” Tobacco habit Bleeding Complications Squamous histology type Total hospitalization Postoperative hospitalization | 63% vs 85% 73.3 yrs vs 87 yrs 7.0 yrs vs 12.3 yrs 32 yrs vs 47 yrs 130mL vs 240mL 36% vs 82% 18% vs 33% 18 d vs 21 d 14 d vs 17 d | P=.018 P=.009 P=.012 P=.002 P<.001 P<.001 P<.013 P=.003 P=.001 | Univariate: No readmission group vs Readmission group __________ Multiple logistic regression: “Lung age” P=.040 “Age difference” P=.040 Bleeding P=.030 Complications P<.001 |
| 20 Assi (2015) USA | Demographics Body mass index Comorbidities (Charlson) Chronic lung disease Respiratory function tests Tumor type Stage Neoadjuvant Epidural, paravertebral catheter Approach Type of resection Complications Hospital stay in ICU Admission in ICU Total hospital stay Destination at discharge Mortality Time until readmission Mortality readmission | ICU readmission Charlson-Deyo>0 COPD | 10.4 (1.1–103.5) 1.5 (1.04–2.03) 4.91 (1.96–13.46) | P=.04 P=.03 P=.0006 | Multivariate |
| 21 Langan (2015) USA | Demographic Insurance type Comorbidities Type of surgery Complications Admitting hospital | Comorbidities>2 Complications>2 Hospital “E” | 30 d: 1.7 (1.19–2.49) 90 d: 1.8 (1.34–2.54) 30 d: 1. 6 (1.16–2.29) 90 d: 1.6 (1.19–2.15) 30 d: 0.6 (0.43–0.88) 90 d: 0.6 (0.41–0.76) | N/A | Multivariate Hospital “E”, a participating hospital |
| 22 Ward (2015) USA | Demographic ASA Type of surgery Cancer vs no cancer Complications Mortality | ASA: 3 Pneumonectomy Superficial wound infection Deep wound infection Infection of organ/cavity Pneumonia Thromboembolism Sepsis Reoperation | 1.75 (1.383–2.227) 1.52 (1.004–2.308) 3.59 (2.083–6.217) 14.9 (2.854–77.874) 11.11 (5.44–22.72) 3.1 (2.337–4.114) 4.59 (2.941–7.176) 3.62 (2.256–5.812) 4.25 (3.161–5.736) | P<.0001 P=.048 P<.0001 P=.0014 P<.0001 P<.0001 P<.0001 P<.0001 P<.0001 | Multivariate |
| 23 Stitzenberg (2015) USA | Demographics Married/single Residence Distance to hospital Hospital volume Type of insurance Stage Comorbidities (Charlson) Complications Hospital stay Mortality Destination at discharge Readmission, 30 and 90 d | Age Sex Stage Comorbidity Discharge not to home Hospital stay Complications (90 d, not 30 d) Hospital volume Distance home to hospital (30 d, not 90 d) | 75–79 yrs: 1.23 (1.09–1.38) ≥ 80 yrs: 1.24 (1.08–1.41) Fem.: 0.64 (0.59–0.70) N+: 1.12 (1.02–1.23) M+: 1.44 (1.20–1.74) Ch.I.1: 1.13 (1.03–1.25) Ch.I.≥2: 1.46 (1.32–1.63) Hosp: 1.61 (1.42–1.81) Resid: 3.25 (2.54–4.16) 1.03 (1.03–1.04) 90 d: 1.08 (1.03–1.12) Q2: 1.25 (1.11–1.41) Q3: 1.15 (1.02–1.29) Q4: 1.26 (1.12–1.43) Q2: 1.14 (1.01–1.28) Q4: 1.27 (1.12–1.45) | P<.001 P<.01 P<.001 P<.05 P<.001 P<.05 P<.001 P<.001 P<.001 P<.001 P<.001 P<.001 P<.05 P<.001 P<.05 P<.001 | Multivariate |
| 24 Stiles (2016) USA | Demographic Hospital stay Comorbidities (Charlson-Deyo) Type of surgery Complications Type of insurance | Male Medicaid Comorbidities: Weight loss Electrolyte disorder Iron-deficiency anemia Blood-loss anemia Peripheral vasculopathy Complicated diabetes Complicated HTN Non-complicated HTN Hospital stay: 6–8d ≥9 d | 1.19 (1.11–1.28) 1.29 (1.09–1.52) 1.34 (1.05–1.69) 1.22 (1.01–1.46) 1.32 (1.16–1.49) 1.89 (1.16–3.09) 1.21 (1.06–1.38) 1.14 (1.03–1.25) 1.47 (1.09–1.99) 1.12 (1.03–1.22) 1.42 (1.25–1.61) 1.88 (1.62–1.27) | P<.0001 P<.004 P=.02 P=.04 P<.01 P=.01 P<.01 P=.01 P<.01 P<.01 P<.01 P<.01 | Multivariate |
| 25 Medbery (2016) USA | Demographics Socioeconomic (income, education, place of residence) Comorbidities (Charlson-Deyo) Type of surgery Hospital stay Type of hospital Type of insurance | Male Charlson-Deyo≥1 Socioeconomic level < $30 000 $30 000–34 999 $35 000–45 999 Private insurance Residence: Urban (vs metropolitan) Rural (vs metropolitan) VATS | 1.23 (1.07–1.43) 1.23 (1.06–1.42) 1.51 (1.18–19.92) 1.38 (1.12–1.71) 1.23 (1.03–1.48) 0.79 (0.67–0.93) 0.71 (0.57–0.88) 0.47 (0.26–0.84) 1.42 (1.20–1.65) | P=.004 P=.006 P<.001 P=.003 P=.025 P=.004 P=.002 P=.011 P<.001 | Multivariate |
| 26 Rosen (2016) USA | Demographic Comorbidities (Charlson-Deyo) Type of insurance Socioeconomic (income, education) Hospital stay (discharge practices) Type of surgery Tumor variables (histology, grade, stage) Hospital variables (type, volume, location) | Male Charlson-Deyo: 1 ≥2 Grade 4 malignancy Advanced stage III IV | 1.16 (1.07–1.26) 1.19 (1.09–1.30) 1.38 (1.23–1.55) 1.4 (1.01–1.92) 1.21 (1.07–1.37) 1.38 (1.06–1.79) | P<.001 P<.001 P<.001 P=.041 P=.0027 P=.016 | Multivariate |
| 27 Dickinson (2017) USA | Demographics Place of residence Comorbidities Type of surgery Operative time Readmission ICU Post-op pain scale Perfusion: Furosemide post-op Transfusion Mortality Complications Destination at discharge Day of week of discharge Hospital stay Discharge with pleural drain or urinary cath. | ppoFEV1% (median) Operative time (minutes, median) Post-op pain scale 12–24h≥6 Perioperative furosemide Transfusion Air leak>5 d Discharge to home | 82(33–147) vs 75(39–107) 130.8(84.2) vs 161.3(84.3) OR: 2.696 (1.372.5.299) 23% vs 48% 4% vs 16.7% 5.8% vs 14.3% OR: 0.323 (0.113–0.937) | P=.042 P=.031 P=.004 P=.0008 P=.003 P=.027 P=.0375 | Intermixed univariate with multivariate results Univariate: No readmission group vs Readmission group Multivariate: OR |
The corresponding bibliographic reference appears together with the author.
yrs: years; ASA: American Society of Anesthesiologists; d: days; COPD: chronic obstructive pulmonary disease; Fem.: female; HTN: hypertension; CI: confidence interval; Ch.I.: Charlson index; M+: distant metastasis; N/A: not analyzed, not available; N+: node involvement; OR: odds ratio; post-op: postoperative; ppoFEV1%: predicted post-op forced expiratory volume in one second %; Q: quartile; Hosp.: hospital; V.: variables; VATS: video-assisted thoracic surgery; vs: versus; ICU: intensive care unit; $: US dollars.
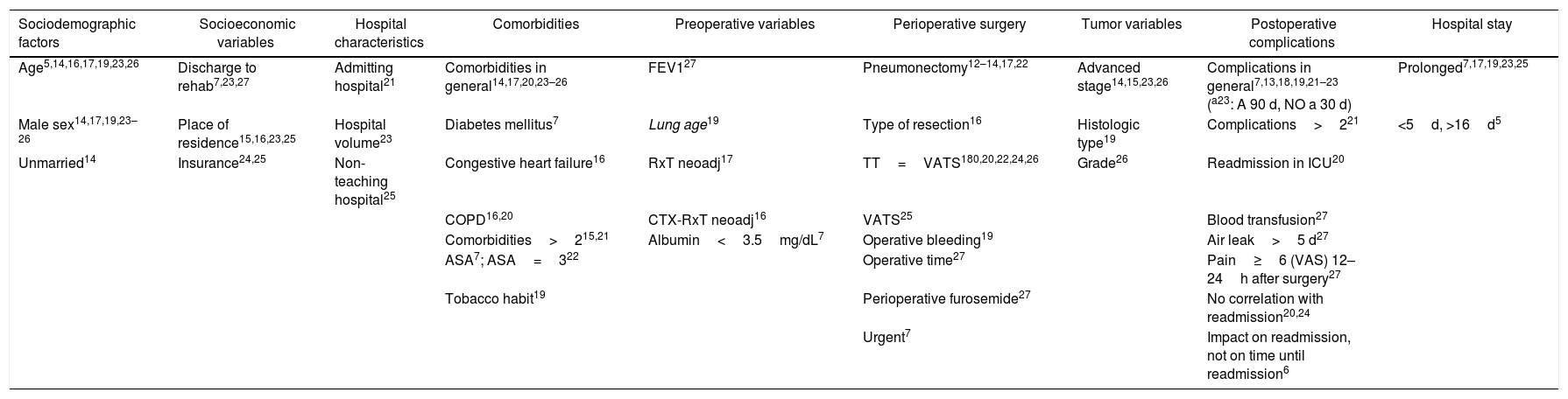
Risk factors for readmission.
| Sociodemographic factors | Socioeconomic variables | Hospital characteristics | Comorbidities | Preoperative variables | Perioperative surgery | Tumor variables | Postoperative complications | Hospital stay |
|---|---|---|---|---|---|---|---|---|
| Age5,14,16,17,19,23,26 | Discharge to rehab7,23,27 | Admitting hospital21 | Comorbidities in general14,17,20,23–26 | FEV127 | Pneumonectomy12–14,17,22 | Advanced stage14,15,23,26 | Complications in general7,13,18,19,21–23 (a23: A 90 d, NO a 30 d) | Prolonged7,17,19,23,25 |
| Male sex14,17,19,23–26 | Place of residence15,16,23,25 | Hospital volume23 | Diabetes mellitus7 | Lung age19 | Type of resection16 | Histologic type19 | Complications>221 | <5d, >16d5 |
| Unmarried14 | Insurance24,25 | Non-teaching hospital25 | Congestive heart failure16 | RxT neoadj17 | TT=VATS180,20,22,24,26 | Grade26 | Readmission in ICU20 | |
| COPD16,20 | CTX-RxT neoadj16 | VATS25 | Blood transfusion27 | |||||
| Comorbidities>215,21 | Albumin<3.5mg/dL7 | Operative bleeding19 | Air leak>5 d27 | |||||
| ASA7; ASA=322 | Operative time27 | Pain≥6 (VAS) 12–24h after surgery27 | ||||||
| Tobacco habit19 | Perioperative furosemide27 | No correlation with readmission20,24 | ||||||
| Urgent7 | Impact on readmission, not on time until readmission6 |
The corresponding bibliographic reference appears in superscript.
ASA: American Society of Anesthesiologists; VATS: video-assisted thoracoscopic surgery; d: days; VAS: visual-analog scale; COPD: chronic obstructive pulmonary disease; CTx: chemotherapy; RxT: radiotherapy; TT: thoracotomy; ICU: Intensive Care Unit; FEV1: forced expiratory volume in one second.
Regarding sociodemographic variables as determining factors for readmission, several studies showed an association with sex, which was male in all cases14,17,19,23–26; advanced age was also associated with readmission in several of the articles5,14,16,17,19,23,26; one study also found a relationship between being single/unmarried and the risk of readmission.14
According to results presented by different authors, a patient's socioeconomic situation was also associated with the probability of readmission (estimated as discharge to a care facility,7,23,27 place of residence,15,16,23,25 or even insurance24,25).
The hospital of the initial admission,21 hospital volume,23 and non-teaching hospitals25 were also associated with readmission in certain studies.
As for the clinical characteristics of the patients, the presence of comorbidities was associated with readmission (in a broad sense for some authors,14,17,20,23–26 and more specifically for others – diabetes mellitus,7 congestive heart failure,16 chronic obstructive pulmonary disease [COPD],16,20 more than two comorbidities15,21). The ASA classification was associated with the risk of readmission in two studies,7,22 tobacco habit only in one,19 and two of the studies found a correlation with respiratory function tests (forced expiratory volume in one second [FEV1])27; and a parameter described by the authors themselves, the “lung age”, based on the results of said respiratory tests19). Radiotherapy17 and neoadjuvant chemoradiotherapy16 were found to be risk factors in isolated studies.
Regarding the surgical variables, pneumonectomy was identified as a determining factor for readmission in several of the studies,12–14,17,22 while another found differences between the different types of resection.16 As for the approach, several studies did not find differences in risk of readmission between thoracotomy and video-assisted thoracoscopic surgery (VATS)18,20,22,24,26; however, one study suggested that VATS was a risk factor for readmission,25 while another found a protective effect.16 The study by Lucas et al.7 was the only paper that identified the urgent nature of the surgery as a risk factor for readmission.
Perioperative events were considered significant risk factors by two authors: Ogawa et al. (intraoperative bleeding)19 and Dickinson et al. (operative time, perioperative use of furosemide and transfusion).27
Several authors described postoperative complications as being very significant determinants for readmission,7,13,18,19,21–23 although with a few clarifications in certain cases: Langan et al. found them to be a risk factor when there were more than two complications,21 and Stitzenberg et al. found them to be a significant factor for readmission within 90 days, but not within 30 days.23 Furthermore, Assi et al. only found readmission in the ICU to be a determining factor,20 and Dickinson et al. associated readmission particularly with blood transfusion, air leak longer than 5 days, and pain intensity in the 12–24h postoperative period that was 6 or greater on the visual–analog scale.27 However, Gonzalez et al. only analyzed the possible correlation of complications over the time to readmission, with no observed relationship between the two events6; likewise, Assi et al.20 and Stiles et al.24 also found no correlation between complications and readmission after a specific evaluation.
Pathological characteristics and tumor stage have also been associated with the risk of readmission by some authors, including both the histological type19 or the degree of malignancy,26 as well as advanced tumor stage.14,15,23,26
A prolonged postoperative hospital stay was identified as a risk factor by several authors7,17,19,23,25 and differentially (when it was less than 5 days or greater than 16 days) by Freeman et al.5
In the studies evaluating readmission within 30 and 90 days, two determined that the risk factors were similar for readmission in both time periods,21,23 and the article by Stitzenberg et al.23 also found similar causes for readmission in both periods.
Main Causes of ReadmissionThe most frequent causes of readmission were respiratory in origin (respiratory failure, dyspnea, pneumonia, pneumothorax, chest pain)5,12,13,15,16,18,19,21,23,24,27 followed by cardiovascular complications (arrhythmias, heart failure).5,6,15,16,23,24 Only a few studies identified infectious causes as significant.12,15,21,22 Postoperative complications were a cause of readmission in two studies,6,24 and one study identified gastrointestinal causes.21
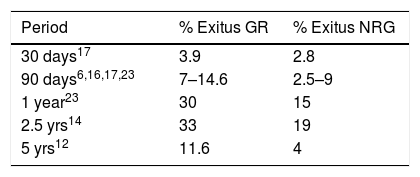
Impact on SurvivalThe impact of readmission on survival was analyzed by several authors, determining 5-year survival rates (78% in the non-readmission group [NRG] vs 44% in the readmission group [RG])19 or the mortality rate at different time periods, as shown in Table 6.
Mortality rate for different time periods.
| Period | % Exitus GR | % Exitus NRG |
|---|---|---|
| 30 days17 | 3.9 | 2.8 |
| 90 days6,16,17,23 | 7–14.6 | 2.5–9 |
| 1 year23 | 30 | 15 |
| 2.5 yrs14 | 33 | 19 |
| 5 yrs12 | 11.6 | 4 |
Next to the time period, the corresponding bibliographic reference appears in superscript.
NRG: no readmission group; GR: readmission group.
In addition to the impact of readmission, the study by Farjah et al.14 found that prolonged hospital stay and hospitalization in care centers also have a significant effect on mortality.
Hu et al.16 did not find higher 90-day mortality among patients who were readmitted two or more times during the first 60 days (16.2%) than those who were only readmitted once (13.8%, P=.295); also. the greater risk is determined by readmission during the first 30 days (OR: 5.79, P <.001). Similarly, the mortality rate showed no differences between patients who were readmitted at the hospital where they were operated on (13.6%) versus those who were readmitted at other medical centers (16.4%, P=.16). According to the results of this study, readmission for postoperative problems did not lead to higher mortality when these were due to other unrelated diagnoses (OR: 1.22, P=.21).
In a study focusing on the impact of the time elapsed until readmission, Gonzalez et al. found that the risk of mortality within 90 days increased if the readmission occurred during the first 5 days after discharge (OR: 8.12; 95% CI: 7.26–9.09), compared to when the readmission occurred after 21 days (OR: 5.97, 95% CI: 5.16–6.90). This effect was also detected on 30- and 60-day mortality rates.
The study by Puri et al.17 also showed that readmission was an independent risk factor for both 30-day mortality (OR: 1.20; 95% CI: 1.01–1.42) as well as 90-day mortality (HR: 1.37, 95% CI: 1.28–1.47).
However, the retrospective study by Dickinson et al.27 including patients who had undergone surgery over the course of a year did not find a significant difference in mortality between the readmission group and the group that did not present readmission during the 30 days after discharge (HR: 1.13; 95% CI: 0.43–2.93; P=.8).
DiscussionTo give an idea of the specific impact of readmissions on the national healthcare system, in addition to their impact on patients themselves, it is estimated that 19% of all patients are readmitted in the first 30 days after discharge, with an annual economic impact for the US Medicare system of 17 billion dollars.28
In Spain, according to data from the Ministry of Health, Social Services and Equality, based on data from the Minimum Basic Data Set, in the last year analyzed (2013) the hospital readmission rate was 7.48% for all Major Diagnostic Categories, a figure that has been gradually increasing in successive years.29
Readmissions are more frequent in medical care processes (often related with emergency admissions) than in surgical treatment (usually scheduled and with previously prepared patients). As a result, approximately 75% of all readmissions are due to medical processes.28,30,31 However, the factors associated with readmissions and the diagnoses leading to readmission after lung surgery have not been extensively studied.
In the literature, most of the studies published on postoperative readmission focus on the readmission rates of specific processes and in specific populations, with widely varying methodologies and study population characteristics.32 Almost all of the studies evaluated in this review have been population-based retrospective cohort studies, based on large national databases in many cases. This type of studies presents an important risk of selection bias: for instance, population studies based on the Medicare database, which registers patients over 65, can only have data from older patients6,14,16,23; studies that use the National Surgical Quality Improvement Program (NSQIP) database analyze readmission after the surgical intervention,33 not only after hospital discharge7,18,22 (possible attrition bias); studies based on the National Cancer Data Base (NCDB) have a good probability of detection bias by collecting only the readmissions occurring at the hospital where the initial admission took place.17,25,26 This limitation was also presented by the multicenter study published by Langan et al.21 (in general, it is estimated that approximately one-third of readmissions occur at a different hospital than where the initial admission took place, as observed in several of the studies analyzed,5,12,13,16,27 mainly due to geographical reasons or insurance, depending on the healthcare system). Other inclusion criteria in the different studies that were presented heterogeneously were the type of surgery that the patients underwent and the indication for surgery (bronchogenic carcinoma, or other pathologies).
The readmission rates found by the different studies analyzed showed a variability that is probably explained by the disparate methodological aspects that we have just discussed, ranging from the characteristics of the population studied, databases used or participating hospitals, to the type of surgery conducted and its indications.32
Regarding the risk factors for readmission (Tables 4 and 5), the different studies on readmission after lung resection confirmed the following main factors: patient sociodemographic and socioeconomic variables; comorbidities; resection type, especially pneumonectomy, with no differences found in terms of the approach (thoracotomy vs video-assisted thoracoscopic surgery); postoperative complications; and prolonged hospital stay. In general terms, these findings correlate with published studies about readmission after different surgical procedures in different specialties.34,30
The main causes of readmission found were medical complications, especially respiratory, followed by cardiac complications. This aspect also agrees with articles published about readmissions in different types of surgical procedures, which usually conclude that the majority of postoperative admissions are due to medical complications in up to 70% of cases.35
The impact on survival is another significant dimension of postoperative readmission, as confirmed by all the studies in the series that analyzed this variable, which concurs with published data for both medical and surgical procedures in general.30
In short, the majority of studies published on readmission after lung resection surgery are widely heterogeneous in the methodology used and in the characteristics of the population studied. Nevertheless, all of them emphasize the importance of reducing postoperative readmission rates due to their impact on the healthcare system, patient survival and quality of life.
Authors’ ContributionsStudy design: García-Tirado, Júdez-Legaristi, Landa-Oviedo, Miguelena-Bobadilla.
Data collection: García-Tirado, Júdez-Legaristi, Landa-Oviedo.
Analysis and interpretation of the results: García-Tirado, Júdez-Legaristi.
Article composition: García-Tirado, Miguelena-Bobadilla.
Critical review and approval of the final version: García-Tirado, Júdez-Legaristi, Landa-Oviedo, Miguelena-Bobadilla.
Conflict of InterestsThe authors have no conflicts of interests to declare.
Please cite this article as: García-Tirado J, Júdez-Legaristi D, Landa-Oviedo HS, Miguelena-Bobadilla JM. Reingreso no planificado tras cirugía de resección pulmonar: revisión sistemática. Cir Esp. 2019;97:128–144.