The objective of this study was to compare with the conventional open approach, the surgical and aesthetic results of endoscopic thyroidectomy via unilateral axillo-breast approach (UABA) with gas insufflation in patients with a unilateral thyroid nodule.
MethodsBetween August 2017 and August 2020, a prospective comparative cohort study was carried out in patients proposed for hemithyroidectomy. The patients were assigned to one type of approach (Open or Endoscopic) in a successive manner. Surgical results and aesthetic satisfaction at hospital discharge and during the 12-month follow-up were evaluated and compared between both groups.
ResultsA total of 200 patients were included in the study: 100 for the Open approach and 100 for the Endoscopic. The baseline patient characteristics were similar between both groups. Total operative time was longer in the Endoscopic approach, due to the time required for subcutaneous dissection (the hemithyroidectomy time was similar in both groups). There was no significant difference in the frequency of major complications. The length of hospital stay was longer (for 1 day) in the Endoscopic group. The aesthetic satisfaction of the patients was significantly higher in the Endoscopic than in the Open group (p < 0.001), at hospital discharge and at 12-month follow-up.
ConclusionUABA with gas insufflation for hemithyroidectomy represents a safe and effective therapeutic option for the treatment of unilateral benign thyroid pathologies.
El objetivo de este estudio fue comparar con el abordaje abierto convencional, los resultados quirúrgicos y estéticos de la tiroidectomía endoscópica por abordaje axilo-mamario unilateral (de sus siglas en inglés, UABA) con insuflación de gas en pacientes con nódulo tiroideo unilateral.
MetodosEntre agosto 2017 y agosto 2020, se llevo a cabo un estudio prospectivo comparativo de cohortes en pacientes propuestos para hemitiroidectomía. Los pacientes se asignaron a un tipo de abordaje (Abierto o Endoscópico) de manera sucesiva. Los resultados quirúrgicos y la satisfacción estética al alta hospitalaria y durante el seguimiento a 12 meses fueron evaluados y comparados entre ambos grupos.
ResultadosUn total de 200 pacientes fueron incluidos en el estudio: 100 se asignaron al abordaje Abierto y 100 al Endoscópico. Las características demográficas de los pacientes fueron similares entre ambos grupos. El tiempo operatorio total fue mayor en el abordaje Endoscópico, debido al tiempo necesario para la disección subcutánea (el tiempo de hemitiroidectomía fue similar en ambos grupos). No hubo diferencia significativa en la frecuencia de complicaciones mayores. El tiempo de estancia hospitalaria fue mayor (por 1 día) en el grupo Endoscópico. La satisfacción estética de los pacientes fue significativamente mayor en el grupo Endoscópico que en el Abierto (p < 0,001), al alta hospitalaria y al seguimiento a 12 meses.
ConclusionEl UABA con insuflación de gas para la hemitiroidectomía representa una opción terapéutica segura y eficaz para el tratamiento de patologías benignas tiroideas unilaterales.
Thyroid nodules are significantly more frequent in young women than in men.1 Conventional thyroidectomy, through classic Kocher incision, leaves a noticeable scar in the lower neck that can significantly affect quality of life, especially in patients with poor wound healing.2–6 In the last 30 years, advances in minimally invasive surgery have resulted in different methods for thyroid gland surgery with potential benefits such as limiting external scarring, improving cosmetic result, reducing postoperative pain and recovery time after surgery, without compromising efficacy in the treatment of thyroid disease.7–9
Minimally invasive approaches for thyroidectomy can be classified as cervical or extracervical.7,8 Multiple clinical studies comparing the different minimally invasive approaches in terms of feasibility, invasiveness, and aesthetics are described in the literature, but there is no clear evidence and thus no consensus on the best minimally invasive approach for thyroidectomy.7–9 In 2013, Lee et al. first reported UABA with gas insufflation for thyroidectomy as a modification of the bilateral axillary-breast approach (BABA) previously described by Choe et al. and the unilateral axillary-breast approach (UABA) without gas insufflation described by Koh et al.10–12 Both the initial BABA and UABA without gas insufflation are aesthetically adequate and surgically effective approaches, but a major disadvantage is the need for extensive dissection of the subcutaneous tissue from the axilla to the thyroid cell to create the skin flap and place the external retractor that maintains the surgical working space.10–12 UABA with gas insufflation is theoretically less invasive by considerably decreasing the dissection of the subcutaneous tissue; it is no longer necessary to place an external retractor to maintain the surgical working space, and it also preserves aesthetic results by keeping the scars out of the neck.10,13
Most studies evaluating minimally invasive extracervical approaches for thyroidectomy are from Asian countries, where these techniques have been widely accepted, probably due to the cultural and psychosocial controversies that a scar on the neck represents in these regions.7,8 In America and Europe, these minimally invasive surgical approaches are being adopted with caution, for reasons such as differences in population, complexity of surgical techniques, and relative costs.2,9 However, an earlier systematic review of the literature revealed that European studies evaluating these techniques reported to date, are scarce and there is no European study that evaluates thyroidectomy via UABA with gas insufflation.8,9 The aim of this prospective study was to compare the surgical and aesthetic results of endoscopic thyroidectomy via UABA with gas insufflation with the conventional open approach in patients with a unilateral thyroid nodule.
MethodsBetween August 2017 and August 2020, a prospective comparative cohort study was conducted in patients proposed for hemithyroidectomy with restrictive selection criteria in our centre’s medical-surgical endocrinology unit. This study was approved by our hospital’s Ethics and Research Committee (HCB/0202). All patients were informed in detail of each procedure before giving their written consent. This study was designed, developed, analysed, and reported according to STROBE recommendations.14
PatientsSelection criteriaInclusion criteria were patients older than 18 years of age with indication for hemithyroidectomy presenting with benign thyroid nodule <5 cm, cytologically indeterminate nodule (Bethesda category III) <5 cm, and with preoperative thyroid ultrasound with estimated thyroid diameter <20 cm and estimated glandular volume <45 mL. Preoperative breast and axillary evaluations (mammography/ultrasound) without pathological findings.
Exclusion criteria were as follows: indication for total thyroidectomy and/or history of thyroid surgery, radioactive iodine ablation, head or neck radiotherapy, vocal fold paralysis, patients with an intellectual disability, diagnosis of thyroid cancer, large metastatic lymph node clusters with invasion of surrounding structures, giant intrathoracic goitres. Presence of pacemakers or central venous access for placement at pectoral, subclavian or cervical level, osteoarthritis, surgery, or limited shoulder joint mobility. Patients with high anaesthetic risk or intolerant to CO2 insufflation.
Elimination criteria: impossibility of performing the surgical intervention, decision by the patient not to continue in the study, loss to follow-up, either for reasons unrelated to the procedure or for personal reasons.
Preoperative assessment and evaluation of variablesAfter a detailed oral and written explanation of the risks, advantages, and disadvantages of the conventional open and endoscopic procedure via UABA with gas insufflation, the patients were assigned to a technique according to order of arrival (1 to 1 ratio) and were categorized into two groups according to the approach used, conventional open group (open), or endoscopic via UABA with gas insufflation (endoscopic). As preoperative assessment, and according to international guidelines, physical examination of the head and neck, laboratory tests, cervical ultrasound, and fine needle aspiration (FNA) were performed. The main study variable was the presence of a major complication (intraoperative and/or postoperative). The surgical outcomes evaluated were operative time (time between skin incision and closure), intraoperative blood loss, postoperative pain (assessed by visual analogue scale [VAS]), drainage (every 24 h), drainage removal time, hospital stay, pathological findings, nodule size, and postoperative complications (transient or permanent vocal fold paralysis, hypocalcaemia, wound infection, seroma, postoperative haemorrhage/haematoma, skin burn, subcutaneous emphysema, neck or chest wall paraesthesia, and swallowing difficulty). Vocal fold paralysis was considered permanent in the absence of recovery at six months postoperatively. Outpatient follow-up of patients was performed at two weeks, three and 12 months after surgery. All patients were assessed for postoperative pain, postoperative complications, and cosmetic results by evaluating the degree of patient satisfaction using the scale: 1 = very dissatisfied, 2 = dissatisfied, 3 = acceptable, 4 = satisfied, and 5 = very satisfied.
Surgical procedureAll surgeries were performed by surgeons trained in endocrine and minimally invasive surgery with experience of more than 30 endoscopic thyroidectomies (cut-off previously recommended as an adequate learning curve).7,8 Antibiotics were not used prophylactically. The operative concept of hemithyroidectomy was defined for this study as unilateral thyroid lobectomy with isthmectomy.
Open hemithyroidectomyThe surgical technique for the conventional open procedure is previously described in Gómez Ramírez J, Endocrine Surgery, 2020.15
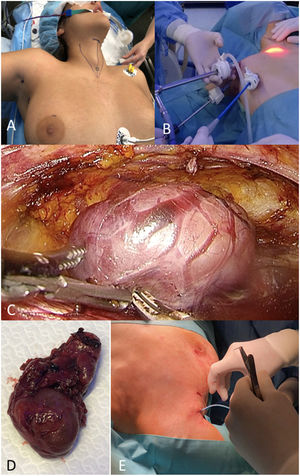
Hemithyroidectomy via UABA with gas insufflationAccording to the technique described by Lee et al. the patient is placed in the supine position with their neck rotated to the contralateral side of the lesion and extended, using a pillow for the ipsilateral shoulder.10,13,16 The arm on the side of the lesion is placed in abduction to expose the axilla, the anterior borders of the sternocleidomastoid muscles (SCM) and sternal fork are identified and marked. For trocar placement, a mark is made 1 cm posterior to the anterior axillary line and parallel to the axillary skin fold, another mark 5−6 cm below and parallel to the previous mark, just at the latero-superior mammary fold, proximal to the axilla and a third mark, at the circumareolar laterosuperior border of the ipsilateral breast (Fig. 1A). The main surgeon is positioned between the abducted arm and the patient's body, the assistant surgeon above the abducted arm and the scrub nurse on the contralateral side, positioning of the viewing screens depends on the number available. Then, the specific incisions are made to insert a 12 mm trocar at the level of the second axillary marking until reaching the suprafacial plane of the pectoralis major muscle, which will be used to introduce the 10 mm/30° endoscope, reaching, through an avascular plane and by means of blunt dissection and facilitated by CO2 insufflation with a pressure between 5 and 8 mmHg, the sternal fork and the insertion of the ipsilateral ECM muscle. Another 5 mm trocar is introduced through the circumareolar marking (with subcutaneous trajectory towards the sternal fork) to insert the energy device to be used (Fig. 1B). The sternal fork area is dissected under endoscopic guidance and with the energy device, to facilitate insertion of the remaining 5 mm axillary trocar, which will serve as a working port, providing a comfortable position for both the surgeon and all members of the surgical team. CO2 pressure is maintained between 5 and 8 mmHg, while the working space is created. Dissection is initiated through the space between the sternal and clavicular head of the ECM muscle, the internal jugular vein and the sternothyroid muscle are identified and dissected, thus revealing the thyroid gland. The trachea and lower pole of the gland are identified and bluntly dissected with the dissector and energy device, the gland is retracted medially and upwards to identify the recurrent laryngeal nerve and parathyroid glands (Fig. 1C). The upper pole is dissected taking care not to damage these critical structures and then the superior thyroid arteries are carefully dissected and sectioned using the energy device avoiding damage to the cricothyroid muscle, Berry's ligament is dissected respecting the recurrent laryngeal nerve, and finally the isthmus is dissected and sectioned, thus completing the hemithyroidectomy. The specimen is placed in an endobag which is retrieved through a 12 mm axillary port without traumatizing the specimen (Fig. 1D). Haemostasis is checked endoscopically, and a suction drain is placed in the surgical site with exit through the 5 mm axillary port (Fig. 1E). Finally, the skin is sutured, and a compression bandage is placed.
Statistical analysisVariables were expressed as medians and percentages for qualitative variables and for quantitative variables as mean, standard deviation, and interquartile range 25%–75%. Differences between the UABA and open approach groups were assessed by univariate analysis using Pearson's χ2 or Fisher's exact test, 2-sided for dichotomous variables. After assessment of normality (Kolmogorov-Smirnov test), the Student's t test and Mann–Whitney U test were used for comparisons of parametric and nonparametric continuous variables, respectively. Statistical significance was considered at a p-value < .05. SPSS version 21 (IBM Corp., Armonk, NY, USA) will be used for the treatment of the variables.
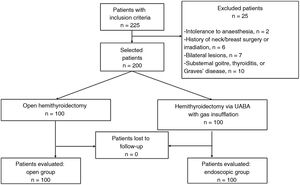
ResultsA total of 225 patients were evaluated for the study, 200 met the selection criteria and were included in the study. Of the 200 patients, 100 were assigned to the open technique and 100 to the endoscopic approach (Fig. 2). Demographic and clinical characteristics are summarized in Table 1. Baseline demographic characteristics were similar between both groups. Likewise, the distribution of type of symptoms, thyroid function, nodule size, and location was similar for both groups. Table 2 summarizes the surgical results. The total operative time was significantly longer in the endoscopic group, due to the time required for subcutaneous dissection from the placement of the trocars to dissection of the surgical space in the thyroid cell, since the hemithyroidectomy time was similar in both groups. There was no blood loss during surgery > 10 mL in any of the patients in either group and none of the patients in the endoscopic group required conversion to open surgery. Regarding complications, there was no significant difference in the presence of haematoma, seroma, vocal fold paralysis (recurrent laryngeal nerve injury), or postoperative pain. However, the endoscopic group had minor complications (21%) such as subcutaneous emphysema (17%), pectoral (3%) and cervical hypoaesthesia (1%), which resolved spontaneously after three months of follow-up. No drain was placed in any of the patients in the open group, in contrast to the endoscopic group who were all left with a drain. The length of hospital stay was significantly longer in the endoscopic group (two days in 28% of patients, p = .01) (Table 2). There was no statistically significant difference in final pathological anatomy between the groups (Table 3). Table 4 summarizes the aesthetic results of both groups. Patient satisfaction with the aesthetic outcome was significantly higher in the endoscopic group compared to the open group (very satisfied vs. satisfied, p < .001), at hospital discharge and persistent during the 12-month follow-up.
Demographic and clinical characteristics of the open and endoscopic groups.
| Characteristic | Open group (%), n = 100 | Endoscopic group (%), n = 100 | p-value |
|---|---|---|---|
| Age, years, mean ± SD | 43 ± 11.5 | 42 ± 8.1 | .1 |
| Gender (female/male) | 86/14 | 89/11 | .302 |
| BMI, kg/m2, mean ± SD | 23.21 ± 3.8 | 23.12 ± 4.1 | .61 |
| ASA | .108 | ||
| I | 76 (76) | 69 (69) | |
| II | 21 (21) | 29 (29) | |
| III | 3 (3) | 2 (2) | |
| IV | 0 | 0 | |
| Symptoms | .206 | ||
| Asymptomatic | 52 (52) | 54 (54) | |
| Tumefaction | 32 (32) | 36 (36) | |
| Compression | 3 (3) | 3 (3) | |
| Tumefaction and compression | 3 (3) | 0 (0) | |
| Pain | 3 (3) | 3 (3) | |
| Other | 7 (7) | 4 (4) | |
| Thyroid function | .37 | ||
| Normal | 97 (97) | 96 (96) | |
| Hyperthyroidism | 3 (3) | 3 (3) | |
| Hypothyroidism | 0 (0) | 1 (1) | |
| Nodule size, media ± SD, mm | 27.81 ± 5.8 | 29.32 ± 7.1 | .407 |
| Location | .13 | ||
| Right lobe | 59 (59) | 53 (53) | |
| Left lobe | 41 (41) | 47 (47) |
Data are presented in numbers and percentage in brackets unless otherwise indicated.
ASA, American society of anaesthesiology score; BMI, body mass index; SD, standard deviation.
Surgical results of the open and endoscopic groups.
| Variable | Open group (%), n = 100 | Endoscopic group (%), n = 100 | p-value | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Follow-up | Follow-up | ||||||||
| 2 weeks | 3 weeks | 12 months | 2 weeks | 3 months | 12 months | ||||
| Subcutaneous dissection time, mean ± SD (min) | 28.4 ± 7.3 | ||||||||
| Hemithyroidectomy time, mean ± SD (min) | 31.8 ± 3.5 | 37.2 ± 2.9 | .057 | ||||||
| Total operative time, mean ± SD (min) | 31.8 ± 3.5 | 65.6 ± 10.2 | < .001 | ||||||
| Intraoperative bleeding | .99 | ||||||||
| <10 mL | 100 (100) | 00 (100) | |||||||
| >10 mL | 0 (0) | 0 (0) | |||||||
| Complications | |||||||||
| - Minor: | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 21 (21) | 9 (9) | 0 (0) | 0 (0) | < .001 |
| Subcutaneous emphysema | 17 (17) | 8 (8) | 0 (0) | 0 (0) | |||||
| Pectoral hypoaesthesia | 3 (3) | 1 (1) | 0 (0) | 0 (0) | |||||
| Cervical hypoaesthesia | |||||||||
| - Major: | |||||||||
| Dysphonia | 1(1) | 0 (0) | 0 (0) | 0 (0) | |||||
| Pain ≥3 VAS | 7 (7) | ||||||||
| Skin burn | 4 (4) | .094 | |||||||
| Subcutaneous haematoma | 6 (6) | 3 (3) | 3 (3) | 0 (0) | 1 (1) | 2 (2) | 1 (1) | 0 (0) | |
| Cervical/pectoral paraesthesia | 3 (3) | 3 (3) | 3 (3) | 0 (0) | 1 (1) | 1 (1) | 1 (1) | 0 (0) | |
| Other | 3 (3) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | ||
| 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (1) | 1 (1) | 0 (0) | 0 (0) | ||
| 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | ||
| 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | ||
| 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | |||
| Hospital stay | .01 | ||||||||
| 1 day | 100 (100) | 72 (72) | |||||||
| 2 day | 0 (0) | 28 (28) | |||||||
Data are presented as numbers and percentages in parentheses, unless otherwise indicated.
SD, standard deviation.
Pathological characteristics of the open and endoscopic groups.
| Variable | Open group (%), n = 100 | Endoscopic group (%), n = 100 | p-value |
|---|---|---|---|
| Benign | 97 (97) | 95 (95) | .24 |
| Follicular adenoma | 55 (55) | 52 (52) | |
| Nodular hyperplasia | 26 (26) | 25 (25) | |
| Multinodular goitre | 13 (13) | 13 (13) | |
| Other | 3 (3) | 5 (5) | |
| Papillary carcinoma | 3 (3) | 4 (4) | .71 |
| pT1a | 3 (3) | 3 (3) | |
| pT1b | 0 (0) | 1 (1) | |
| Follicular carcinoma | 0 (0) | 1 (1) | .83 |
| pT1a | 0 (0) | 1 (1) |
Data are presented in numbers and percentages in brackets unless otherwise indicated.
SD, standard deviation.
Cosmetic results of the open and endoscopic groups.
| Variable | Open group (%), n = 100 | Endoscopic group (%), n = 100 | p-value | ||||||
|---|---|---|---|---|---|---|---|---|---|
| n (%) | Follow-up | n (%) | Follow-up | ||||||
| 2 weeks | 3 months | 12 months | 2 weeks | 3 months | 12 months | < .001* | |||
| Very satisfied | 68* (68) | 68 (68) | 74 (74) | 81 (81) | 91* (91) | 94 (94) | 97 (97) | 99 (99) | |
| Satisfied | 25 (25) | 25 (25) | 23 (23) | 16 (16) | 9 (9) | 6 (6) | 3 (3) | 1 (1) | |
| Acceptable | 7 (7) | 7 (7) | 3 (3) | 3 (3) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | |
| Dissatisfied | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | |
| Very dissatisfied | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | |
Data are presented as numbers and percentages in brackets, unless otherwise indicated.
SD, standard deviation.
UABA with gas insufflation for thyroidectomy is one of the most internationally accepted endoscopic techniques.7,8,13,17 Clinical studies in South Korea and Vietnam demonstrate that UABA with gas insufflation is a safe and effective technique for the treatment of different thyroid pathologies;10,12,13,17 however, there are factors that limit its wide application (especially in America and Europe), such as patient demographics, advanced surgical skills required for both endocrine and minimally invasive surgery and, most importantly, the need to confirm its safety and efficacy compared to the conventional open technique.2,8,9 The present study was designed and conducted with the aim of evaluating the surgical results of endoscopic thyroidectomy via UABA with gas insufflation (compared to the conventional open approach) in the subgroup of patients who can gain the greatest benefit from this procedure and under controlled conditions. In our study, most of the patients in both groups were women with a mean body mass index (BMI) <25 kg/m2, ASA I-II, mean age <55 years, with homogeneous clinical manifestations and thyroid nodule characteristics in both comparison groups.
In our study, all procedures were performed by the same surgical team with experience in both endocrine and minimally invasive surgery and with previous surgical training in the endoscopic technique used. These characteristics may explain the intraoperative bleeding of <10 mL in all patients and conversion to open surgery not being required in any of the patients in the endoscopic group. However, the total operative time was significantly longer in the endoscopic group than in the open group (65.6 ± 10.2 vs. 31.8 + 3.5 min, respectively; p < .001), the difference being explained by the time required from trocar placement to subcutaneous dissection to create the surgical space in the thyroid cell, since in the specific time for hemithyroidectomy there was no statistically significant difference (open: 31.8 + 3.5 min vs. endoscopic: 37.2 + 2.9 min; p = .057). Nevertheless, the total operative time for the endoscopic technique in our study was shorter than for other types of endoscopic approaches.12,18–21 Koh et al. reported a mean operative time for hemithyroidectomy via UABA without gas insufflation of 119.23 + 31.47 min and Youn et al. of 165.3 + 43.5 for hemithyroidectomy via BABA, these differences with our study may be due to the minimal subcutaneous dissection required for UABA with gas insufflation, compared to the other two techniques.12,19 Likewise, there were no differences in major postoperative complications such as dysphonia, pain, or presence of haematoma (Table 2); but the endoscopic group had minor complications related to the subcutaneous dissection procedure (pectoral or cervical hypoaesthesia), and CO2 insufflation, the latter being the most frequent (17%). It is important to note that all these complications resolved by the third month of follow-up and without the need for any specific treatment.
Unlike the open group in which all patients were discharged on postoperative day 1, the hospital stay was significantly longer in the endoscopic group (28% of patients were hospitalized for 2 days). This was because the patients stayed in hospital until the suction drain placed during the surgical procedure was removed (unlike the open group in which no drain was placed, a drain was placed in all patients in the endoscopic group), which remained in situ for more than 24 h in the first 20 patients, and in the remaining patients, the drain was removed within the first 24 h of the postoperative period (very little drainage); none of this had an impact on the development of seromas. In our study no patient developed a seroma, unlike the study by Lee et al. who reported two cases of seroma (2.9%, 2 of 68 patients) and in a recent study where they used the UABA technique, but without gas insufflation, five cases developed seroma (9.6%; 5 of 52 patients).10,12 The wide subcutaneous dissection for the surgical working space may be the reason seroma developed in these approaches, which would explain why the endoscopic group of our study (with minimal subcutaneous dissection required) did not develop a seroma, even despite early removal of the suction drain. Under this same concept, further studies to evaluate the usefulness of suction drainage in UABA with gas insufflation will be necessary, as inserting a drain or not may have an impact on the hospital stay of these patients. It is essential to highlight that the use of CO2 can theoretically be associated with severe complications. However, the gas pressure of 5−8 mmHg recommended and used in our study has not been associated with serious complications and this is consistent with studies by Lee et al. and Nguyen et al.10,13
The cosmetic outcome was significantly better evaluated in the endoscopic group compared to the open group. At hospital discharge, 91% of patients in the endoscopic group were very satisfied with the appearance of their neck and scars and the remaining 9% were satisfied, compared to patients in the open group in which 68% were very satisfied, 25% satisfied, and 7% considered it acceptable, these differences remained significant during follow-up at 2 weeks, 3, and 12 months (p < .001, Table 4). Thyroid nodules are more frequent in young women than in men.1 The surgical scar from conventional open thyroidectomy is located in a visible and exposed area on the anterior aspect of the neck, and in some patients it can even develop in a hypertrophic or keloid fashion, which can cause significant cosmetic problems and impact the psychosocial functionality of the patients.3,5,6,22 Balci et al. reported that the quality of life (QoL) of patients with keloid and hypertrophic scars is affected as much as that of patients with psoriasis.23 In addition, a decrease in QoL is frequent in patients with chronic skin diseases.4 The Dermatology Life Quality Index (DLQI) questionnaire was used to assess the quality of life of patients with dermatological diseases such as psoriasis, acne vulgaris, atopic dermatitis, and hypertrophic scars.4,23–28 In patients with vitiligo, the mean DLQI questionnaire score ranged from 4.82 to 10.67.24–26 In patients with psoriasis and scabies, the mean DLQI score ranged from 8.73 to 9.16 and 10.09, respectively.23,27,28 The mean DQLI score of patients with severe atopic dermatitis was 8.829. Choi et al. reported a mean DQLI score in patients with post-thyroidectomy surgical scar of 9.02, which is similar to that of patients with psoriasis or severe atopic dermatitis.4,29,30 Studies that assess quality of life in thyroidectomized patients via UABA with gas insufflation are essential.
Our study has limitations that need to be highlighted. Our patient selection criteria were restrictive with the aim of evaluating safety, feasibility, and surgical and cosmetic outcomes in the subgroup of patients who can hypothetically gain the greatest benefit from hemithyroidectomy via UABA with gas insufflation: patients with benign or indeterminate unilateral thyroid nodules <5 cm with a preference to avoid the cervical scar of the conventional open technique. However, it is beyond the scope of the study to evaluate patients with other surgical indications such as total thyroidectomy or patients diagnosed with thyroid oncologic diseases. Likewise, the results of our study come from and apply to our centre, since the procedures were performed by our surgical team with experience in both endocrine surgery and minimally invasive surgery and with previous surgical training in the endoscopic technique used; therefore, multicentre studies are necessary to confirm our findings.
In conclusion, our results suggest that in selected patients and with surgical teams experienced in endocrine and minimally invasive surgery, specialists in UABA with gas insufflation, this technique for hemithyroidectomy can be a safe and effective therapeutic option to treat unilateral thyroid disease, with a major complication profile similar to conventional open surgery, but with an excellent cosmetic result.
FundingThe authors declare that no funding was received for this study.
Conflict of interestsThe authors have no conflict of interests to declare.