Treatment of penetrating trauma to the neck is complex due to the vital structures involved. Early diagnosis of cervical injuries is essential, as any delay could lead to elevated morbidity and mortality. We present a case of a penetrating cervical wound with Horner syndrome and no associated vascular injury.
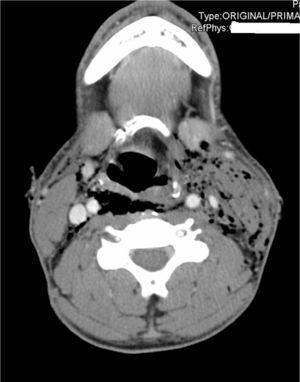
The patient is a 28-year-old male, with no prior medical history of interest, who was sent to our hospital after a suicide attempt with a sharp object (knife) to the neck. We observed dysphonia, but no dyspnoea. Upon examination, vital signs were normal, oxygen saturation was 100% and the Glasgow Coma Scale was 14 points. The patient had 5 injuries in cervical zone II (3 superficial right lateral incised wounds and 2 incised-contused wounds that surpassed the platysma on the left side) with crackles upon palpation on the left side. Anisocoria was observed with miosis of the left eye and ipsilateral ptosis (Fig. 1); the remaining examination was normal. Cervical and chest radiograph demonstrated subcutaneous emphysema without pneumothorax. CT angiography with oral contrast is shown in Fig. 2. Laryngoscopy revealed paralysis of the left vocal cord in a paramedian position together with paralysis of the left hypoglossal nerve; sharp force injury to the left pyriform sinus could not be ruled out. Conservative therapy was begun with intravenous antibiotics, nil per os and follow-up radiology study with a second cervical CT in 24h, which demonstrated improvements in the patient's condition, including reduced subcutaneous emphysema and pneumomediastinum. After progressively initiating oral tolerance, the patient progressed favourably with follow-up lab work and radiological studies within normal ranges. The patient was discharged on the 7th day after hospitalisation after psychiatric testing. At the one-year follow-up visit in the outpatient clinic, the patient continued to have Horner syndrome, but no longer presented paralysis of the vocal cord or of the left hypoglossal nerve.
Cross-section of the cervical CT angiography: subcutaneous emphysema, especially on the left, that reaches the mediastinum, with a possible punctiform injury of the left pyriform sinus; there are no observed injuries to the cervical vessels or extravasation of oral contrast, hematomas, or other alterations.
Essential treatment for patients with penetrating cervical wounds involves initial airway assessment and, afterwards, haemorrhage control. Once these two aspects are regulated and the patient is haemodynamically stable, the cervical lesions can be evaluated. The diagnostic method of choice in a stable patient is CT angiography,1,2 as it is not only a non-invasive method that can evaluate patients at risk for vascular injuries in the neck (pseudoaneurysms, arterial dissections, arteriovenous fistulas, vascular occlusions), but it is also able to diagnose injuries to the digestive tube, airway, spinal cord, etc. that may have gone unnoticed on initial examination. Furthermore, this selective treatment of cervical lesions should include an endoscopic study of the airway and an oesophagogram/oesophagoscopy to exclude airway and oesophageal injuries. Our case was characterised by an uncommon clinical presentation: traumatic Horner syndrome.
Horner syndrome is defined by the triad comprised of anisocoria (resulting from the miosis of the affected eye), ptosis and anhidrosis, which is caused by the loss of sympathetic innervation of the eye and ipsilateral face.3 Trauma-induced Horner syndrome is a rare entity and represents 4%–13% of these syndromes; the most frequent aetiology is tumour-related (35%–60%).4,5 In order to evaluate Horner syndrome caused by trauma, it is important to understand the anatomy of the sympathetic system. This involves 3 nervous system stations that do not cross over: the first neuron originates from the hypothalamus, descends along the brainstem to the ciliospinal centre in the spinal cord to the C8-T2 region. At this point, it connects with the second neuron that crosses under the subclavian artery and ascends in the neck to form a synapse in the superior cervical ganglion near the carotid bulb. After making the synapse with the third neuron, its fibres divide: the vasomotor fibres follow the external carotid, while the oculosympathetic form a plexus around the wall of the internal carotid and enter into the skull up to the orbit.
Thus, in cases with cervical penetrating trauma and Horner syndrome, an associated vascular injury should be suspected, such as dissection of the carotid artery,6 and therefore the diagnostic test of choice is CT angiography.7 Nonetheless, in our case this injury was absent in spite of the close proximity, and there was only an associated small punctiform lesion in the left pyriform sinus that caused important emphysema and pneumomediastinum, which was treated conservatively with success. In addition, the presence of Horner syndrome, dysphonia and subcutaneous emphysema are soft signs in cervical penetrating injuries that require complete diagnostic study.
In short, patients with penetrating cervical trauma must be assessed for airway trauma and vascular injuries, as they are a risk to the patient's life.
Please cite this article as: Guillén-Paredes MP, Flores-Pastor B, Escobar C, de Andrés García B, Aguayo-Albasini JL. Síndrome de Horner traumático sin lesión vascular. Cir Esp. 2015;93:e139–e141.