To evaluate quality of life (QoL) and overall survival after radical cystectomy with cutaneous ureterostomies for locally advanced bladder cancer in elderly patients with high surgical risk.
MethodsFifty eight patients older than 74 years (mean age 80.6±4.3) with locally advanced bladder cancer (group A), underwent radical cystectomy and ureterocutaneous diversion. Patients completed the EORTC QLQC30 before and six months after surgery to assess functional, clinical, and QoL outcomes. The same evaluation was carried out in a control group (group B) of 29 patients (mean age 82.3±3.8 years), who had refused cystectomy. Questionnaires were also administered to patients of both groups who survived at least 20 months and 5 years.
ResultsAll patients presented with an ASA score ≥3. Mean hospital stay was 15.1 days (±4.8) in group A and 23.5 days (±4.1) in group B. No intraoperative complications occurred in group A. Postoperative overall survival evaluated within 6 months in group A was 97% versus 79% in group B (P<.001).
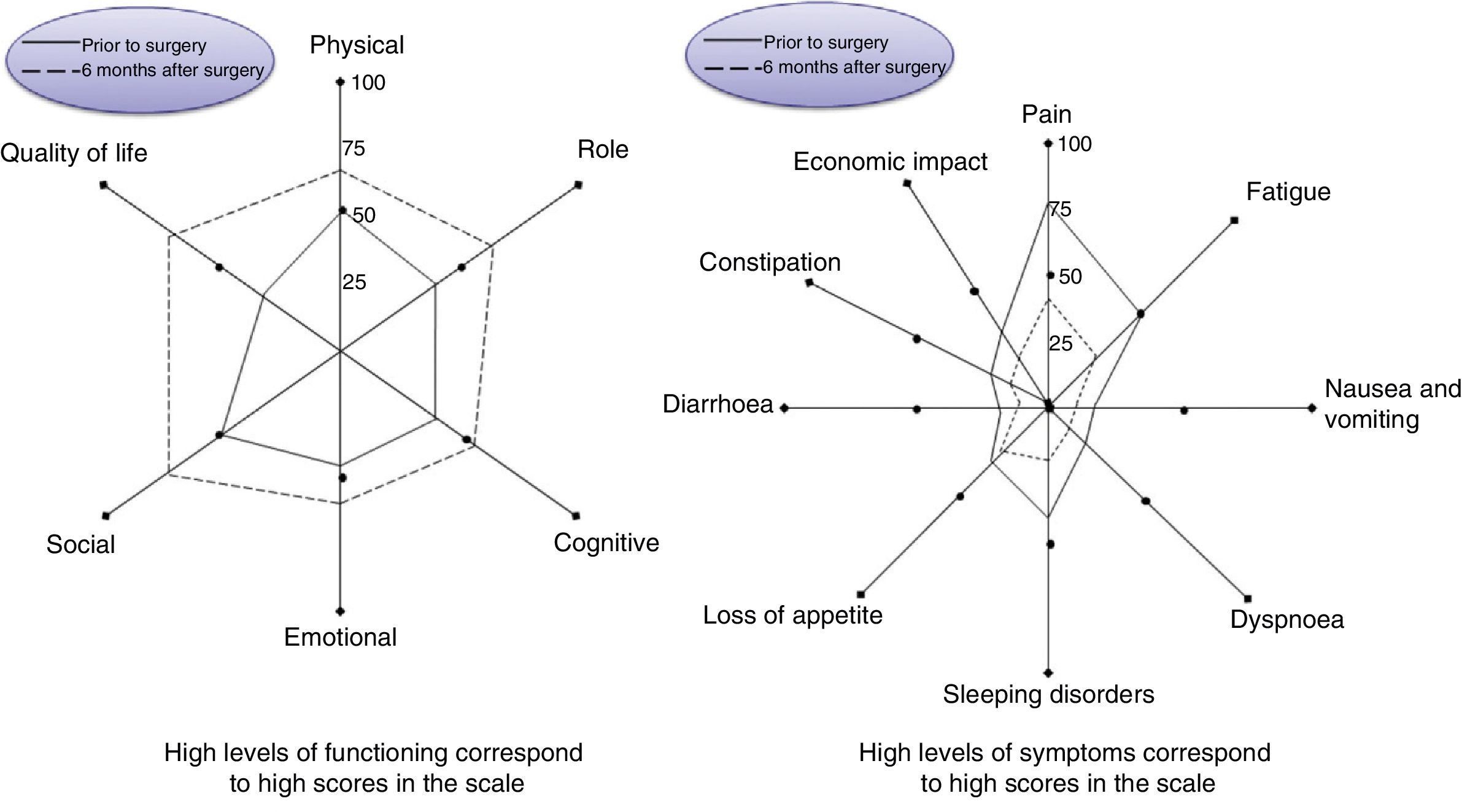
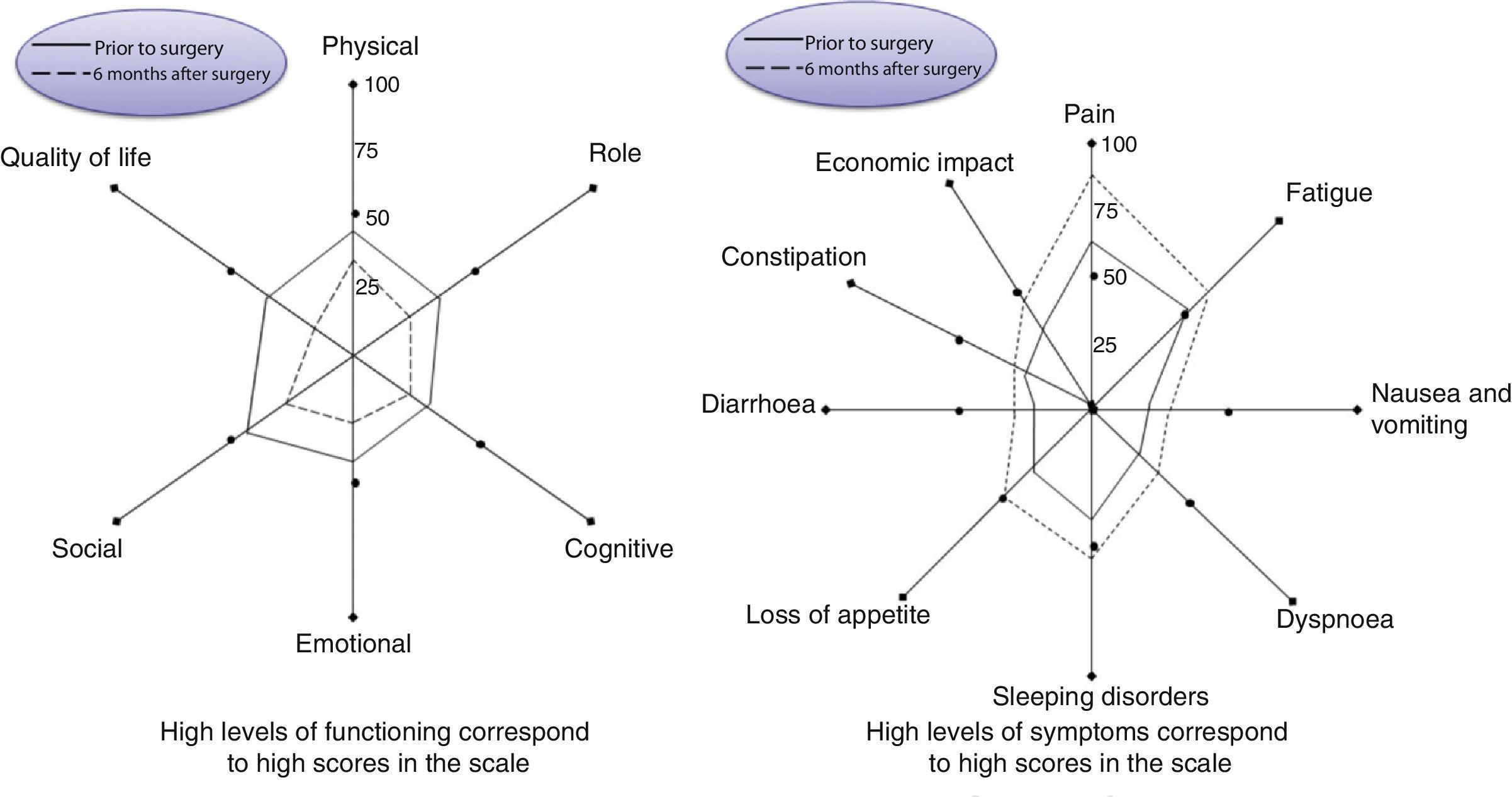
Relation between two groups at 6 months for Qol, functional and symptomatic items investigated showed in group A a statistically significant improvement for all parameters (P<.001). This advantage for patients belonging to group A still resulted evident at 20 months and 5 years.
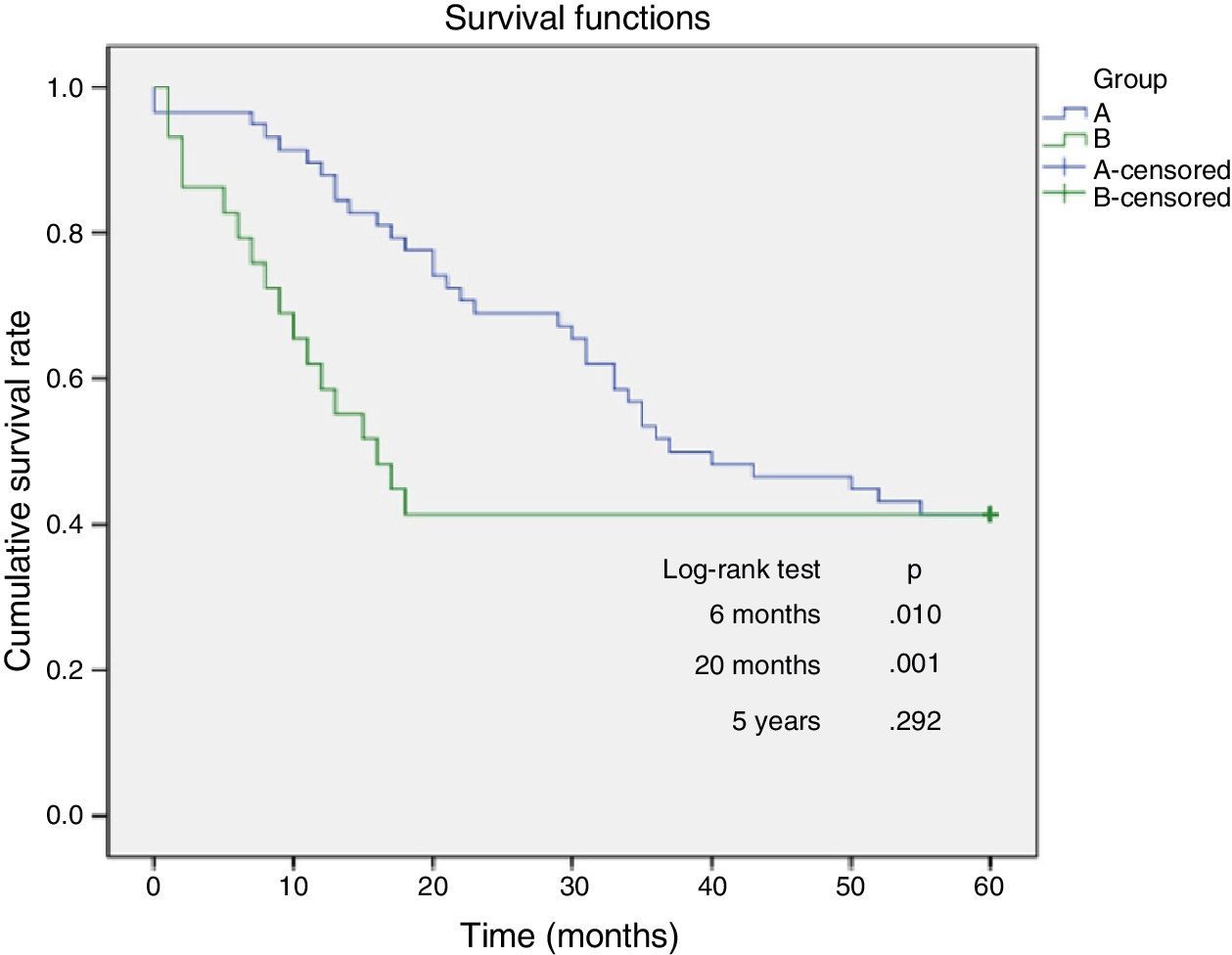
Short-term and 20 months overall survival resulted statistically significant in favour of group A (P<.001).
ConclusionRadical cystectomy with cutaneous ureterostomy represents a valid alternative in elderly patients with invasive bladder cancer and high operative risk. Comparison between two groups showed a statistically significant difference for almost all the Qol related parameters and for short and medium term overall survival.
Evaluar la calidad de vida (QoL) y supervivencia global tras cistectomía radical con ureterostomías cutáneas por cáncer localmente avanzado de vejiga en pacientes ancianos con alto riesgo quirúrgico.
MétodosCincuenta y ocho pacientes, mayores de 74 años (edad media 80,6±4,3) con cáncer de vejiga localmente avanzado (grupo A), fueron sometidos a una cistectomía radical y derivación ureterocutánea. Los pacientes completaron el cuestionario EORTC QLQC30 antes y 6 meses después de la cirugía para valoración de resultados funcionales, clínicos y de QoL. La misma evaluación fue realizada en un grupo control (grupo B) de 29 pacientes (edad media 82,3±3,8 años), que habían rechazado la cistectomía. Los cuestionarios también fueron remitidos a pacientes de ambos grupos que sobrevivieron a los 20 meses y a los 5 años.
ResultadosTodos los pacientes presentaron un ASA ≥3. La estancia hospitalaria media fue de 15,1 días (±4,8) en el grupo A y de 23,5 días (±4,1) en el grupo B. No hubo complicaciones intraoperatorias en el grupo A. La supervivencia global postoperatoria evaluada a los 6 meses en el grupo A fue del 97 vs 79% en el grupo B (p<0,001).
La relación de calidad de vida e ítems de función y síntomas entre los 2 grupos a los 6 meses mostró una mejoría significativa de todos los parámetros en el grupo A (p<0,001). Esta ventaja de los pacientes del grupo A fue todavía más evidente a los 20 meses y a los 5 años.
La supervivencia a corto plazo y a los 20 meses fue significativamente mayor en el grupo A (p<0,001).
ConclusiónLa cistectomía radical con ureterostomía cutánea representa una alternativa válida en pacientes ancianos con cáncer de vejiga invasivo y alto riesgo quirúrgico. La comparación entre los grupos mostró una diferencia significativa en casi todos los parámetros relacionados con la QoL y con respecto a la supervivencia a corto y medio plazo.
Bladder cancer is the fourth cause of death in people over 80 years old. The incidence of bladder cancer in patients over 85 years old is twice as high as that in patients between 65 and 69 years old.1
Although most of the patients have superficial cancer, the disease is diagnosed in an advanced stage with invasive cancer2 in 20%–40% of the cases.
Radical cystectomy is the standard treatment for locally advanced bladder cancer, but despite the continuous advances in surgical procedures, anaesthesiology and postoperative care, it still shows high rates of morbidity and mortality. Morbidity and mortality are also related to the method of urinary diversion.3
A high number of elderly patients have comorbidities such as coronary disease, diabetes mellitus and chronic obstructive pulmonary disease, which encompass true surgical challenges. High-risk elderly patients are classified as grade 3 or 4 of the American Society of Anaesthesiologists score (ASA score). If patients diagnosed with invasive bladder cancer are not treated, most of them will die due to their malignant disease.4,5 Therefore, despite the risk of a major surgery, radical cystectomy continues to be a therapeutic option in the elderly population. There are various diversion techniques. Among them, the choice must be performed according to the patient's age and general condition, tumour extension, renal function, psychological alterations, and patient's acceptance of the treatment. Cutaneous ureterostomy can be the simplest option for urinary diversion in high-risk elderly patients.
The objective of this study is to assess the quality of life (QoL) and global survival after radical cystectomy with cutaneous ureterostomy for the treatment of advanced bladder cancer in elderly patients with high surgical risk.
Materials and MethodsWe performed a retrospective revision of clinical records of 192 patients who were admitted to our department due to bladder cancer and were subjected to a radical cystectomy and urinary diversion between January 2001 and December 2008.
Of these, 76 (39.5%) were elderly patients (>74 years old; 60 males and 16 females) with ASA score ≥3. Among the 76 elderly patients, a cutaneous ureterostomy was performed in 58 cases, a Bricker diversion in 12 cases and an orthotopic ileal neobladder in 6 patients.
Characteristics of the PatientsPatients included in the study were divided into 2 groups. Group A was formed by 58 patients who were subjected to a radical cystectomy with cutaneous ureterostomy with curative intent; and group B was formed by 29 patients with similar clinical and pathological characteristics, who rejected surgery.
Indications for cystectomy included tumours with muscle invasion or superficial multifocal tumours refractory to local treatment. The most common symptoms included haematuria and anaemia, which required hospitalisation, severe local pelvic pain, frequent urination or urge incontinence.
The assessment of the QoL related to health was performed before surgery in every patient and during the follow-up using the questionnaire “European Organisation for Research and Treatment of Cancer Quality of Life questionnaire-C30” (EORTC QLQC30).6
Global survival was assessed 6 months after surgery or during follow-up in patients from group B, and 20 months and 5 years after surgery in both groups. Postoperative complications were thoroughly assessed, and they were defined and classified according to the Clavien classification.7
TreatmentRadical cystectomy consisted of the resection of the bladder, distal ureters, seminal vesicle and prostate in men, and uterus, anterior vaginal wall and urethra in women.
Cutaneous ureterostomy was performed in all the patients treated after the placement of Wiruthan® catheters in ureters, especially designed for cutaneous ureterostomies. These catheters were changed monthly.
All patients received prophylaxis with subcutaneous low-molecular-weight heparin, which started 12h before surgery and continued until discharge from the hospital. Endovenous antibiotics were administered during the first 2 postoperative days.
Quality of Life QuestionnairesThe EORTC QLQ-C30 questionnaire (EORTC, Brussels, 2001) is an instrument validated for quality of life assessment in oncological patients. The most recent version, 3.0, was used in this study. This tool is constantly updated based on the results obtained with the research funded by the International Quality of Life Unit (QLU) and validated by the Quality of Life Group (QLG) from the European Organisation for Research and Treatment of Cancer (EORTC).
The questionnaire consists of 30 questions and covers the following areas: 16 items for 5 functional scales (physical activity, personal role issues, cognitive activity, emotional state, social support), 6 items for 3 scales of symptoms (fatigue, pain, nausea, vomiting), 5 special items (constipation, diarrhoea, insomnia, dyspnoea, economic conditions), and 1 item about the Qol global index.
All patients were invited to participate by filling in the QoL questionnaire if it was possible the day of surgery and 6 months later.
Statistical MethodThe Mann–Whitney U test was used to analyse the differences between the 2 groups. The Kaplan–Meier method was used to calculate the survival functions, and the differences were assessed with 3 tests: Log-rank, Breslow, and Tarone-Ware. All the statistical studies were bilateral and all the analyses were performed using the R software version 2.15.2. Values of P<.05 were considered statistically significant.
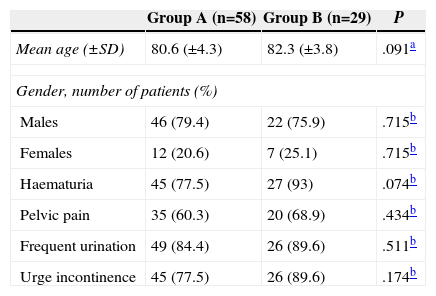
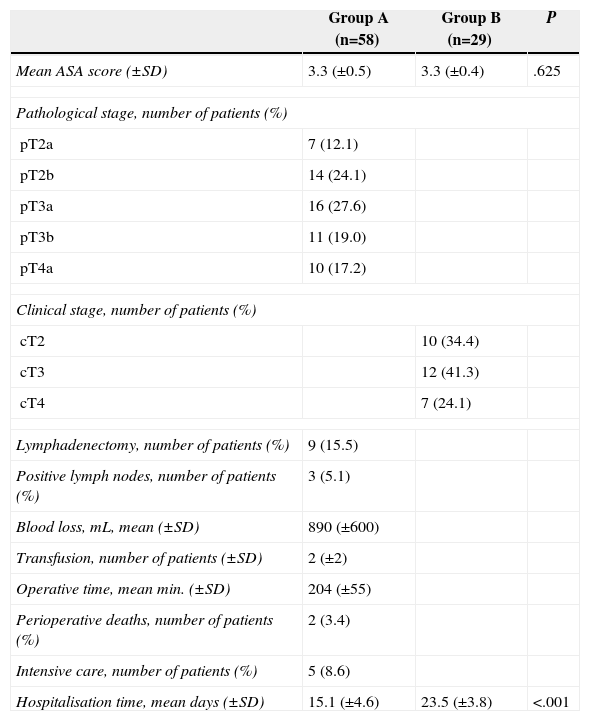
ResultsFifty eight patients were included in group A: 46 men and 12 women, with an average age of 80.6 years (±4.8), 32 of which (55%) were over 80 (Table 1) years old. Twenty-nine patients were included in group B: 22 men and 7 women, with an average age of 82.3 (±3.9), 15 of which (51.7%) were over 80 years old. All patients at baseline time showed similar pathological characteristics without significant differences in the ASA score (P≥.05) (Table 2).
Basic Characteristics of Patients (n=87 Patients).
| Group A (n=58) | Group B (n=29) | P | |
|---|---|---|---|
| Mean age (±SD) | 80.6 (±4.3) | 82.3 (±3.8) | .091a |
| Gender, number of patients (%) | |||
| Males | 46 (79.4) | 22 (75.9) | .715b |
| Females | 12 (20.6) | 7 (25.1) | .715b |
| Haematuria | 45 (77.5) | 27 (93) | .074b |
| Pelvic pain | 35 (60.3) | 20 (68.9) | .434b |
| Frequent urination | 49 (84.4) | 26 (89.6) | .511b |
| Urge incontinence | 45 (77.5) | 26 (89.6) | .174b |
Clinical, Pathological and Surgical Data (n=87 Patients).
| Group A (n=58) | Group B (n=29) | P | |
|---|---|---|---|
| Mean ASA score (±SD) | 3.3 (±0.5) | 3.3 (±0.4) | .625 |
| Pathological stage, number of patients (%) | |||
| pT2a | 7 (12.1) | ||
| pT2b | 14 (24.1) | ||
| pT3a | 16 (27.6) | ||
| pT3b | 11 (19.0) | ||
| pT4a | 10 (17.2) | ||
| Clinical stage, number of patients (%) | |||
| cT2 | 10 (34.4) | ||
| cT3 | 12 (41.3) | ||
| cT4 | 7 (24.1) | ||
| Lymphadenectomy, number of patients (%) | 9 (15.5) | ||
| Positive lymph nodes, number of patients (%) | 3 (5.1) | ||
| Blood loss, mL, mean (±SD) | 890 (±600) | ||
| Transfusion, number of patients (±SD) | 2 (±2) | ||
| Operative time, mean min. (±SD) | 204 (±55) | ||
| Perioperative deaths, number of patients (%) | 2 (3.4) | ||
| Intensive care, number of patients (%) | 5 (8.6) | ||
| Hospitalisation time, mean days (±SD) | 15.1 (±4.6) | 23.5 (±3.8) | <.001 |
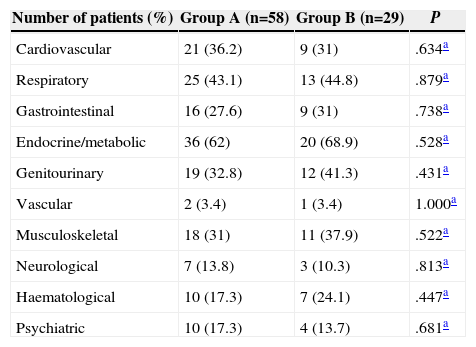
Significant comorbidities were observed in 52 patients from group A (89.8%) and in 26 patients from group B (89.6%). Fifty three percent of all patients from both groups showed more than one comorbidity.
Previous medical history of cardiovascular disease was observed in 36.2% and 31% of the patients of group A and B, respectively, pulmonary disease in 43.1% and 44.8%, chronic renal failure in 6.9% and 3.4%, and metabolic diseases in 62% and 68.9% (Table 3). Fifteen patients from group A (26%) and 4 patients from group B (14%) had previous medical history of abdominal surgery.
Comorbidities of Patients.
| Number of patients (%) | Group A (n=58) | Group B (n=29) | P |
|---|---|---|---|
| Cardiovascular | 21 (36.2) | 9 (31) | .634a |
| Respiratory | 25 (43.1) | 13 (44.8) | .879a |
| Gastrointestinal | 16 (27.6) | 9 (31) | .738a |
| Endocrine/metabolic | 36 (62) | 20 (68.9) | .528a |
| Genitourinary | 19 (32.8) | 12 (41.3) | .431a |
| Vascular | 2 (3.4) | 1 (3.4) | 1.000a |
| Musculoskeletal | 18 (31) | 11 (37.9) | .522a |
| Neurological | 7 (13.8) | 3 (10.3) | .813a |
| Haematological | 10 (17.3) | 7 (24.1) | .447a |
| Psychiatric | 10 (17.3) | 4 (13.7) | .681a |
Data regarding the surgical intervention and recovery, as well as the average hospitalisation time are summarised in Table 2.
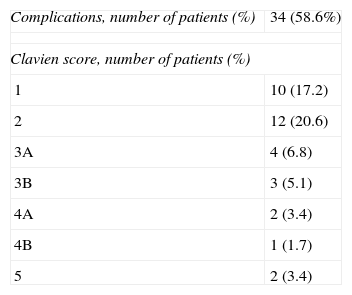
There were no intraoperative complications. Postoperative complications, defined and classified according to the Clavien classification, are summarised in Table 4.
Postoperative Complications.
| Complications, number of patients (%) | 34 (58.6%) |
| Clavien score, number of patients (%) | |
| 1 | 10 (17.2) |
| 2 | 12 (20.6) |
| 3A | 4 (6.8) |
| 3B | 3 (5.1) |
| 4A | 2 (3.4) |
| 4B | 1 (1.7) |
| 5 | 2 (3.4) |
| Clavien score |
| Grade 1: any deviation of the normal postoperative course without need of pharmacological treatment or surgical, endoscopic or radiologic intervention. |
| Treatments allowed include antiemetics, antipyretics, analgesics, diuretics, electrolytes and physiotherapy. |
| Grade 2: complications that require pharmacological treatment not included in grade 1, blood transfusion and total parenteral nutrition. |
| Grade 3: complications that require surgical, endoscopic or radiologic intervention. |
| ≫Grade 3A: intervention without general anaesthesia. |
| ≫Grade 3B: intervention with general anaesthesia. |
| Grade 4: life-threatening complications that require treatment in middle care or intensive care units. |
| ≫Grade 4A: failure of a single organ. |
| ≫Grade 4B: multiple organ failure. |
| Grade 5: death of the patient. |
Postoperative morbidity rate was 58.6%; 38% were due to minor complications and 20.6% were due to major complications, respectively. The most frequent complication was temporary confusion related to anaesthesia (12%). The most frequent major complication was wound infection (8.6%). Congestive heart failure and urinary tract infection were observed in 4 (6.9%) and 3 (5.2%) patients, respectively. Pyelonephritis and disseminated intravascular coagulation were observed in 1 (1.7%) patient and myocardial infarction and respiratory distress occurred in 2 (3.4%) different patients. Wound disruption was observed in 3 (3.4%) patients, pelvic bleeding in 1 (1.7%), who required a reoperation; lymphocele and ileus in 2 (3.4%) and subcutaneous haematoma in 1 (1.7%) patient. There were 2 postoperative deaths (3.4%): one patient died of a myocardial infarction 2 days after surgery and another patient died of pulmonary embolism 31 days after surgery.
The average hospitalisation time was 23.5 days (±4.1) in group B due to frequent admissions: 21 were re-admitted due to persistent haematuria and were subjected to TUR and/or radiotherapy as haemostatic treatment; 6 were admitted due to hydronephrosis and postrenal renal failure treated with percutaneous nephrostomy.
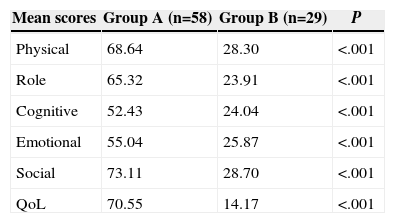
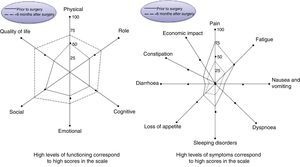
In group A, when comparing the preoperative condition of the patients with the postoperative condition from a functional, symptomatic and QoL results’ perspective, a significant improvement was generally observed in all the investigated items (Figs. 1 and 2). Improvements regarding the preoperative data were observed 6 months later, particularly in the QoL, pain, fatigue, and sleeping disorders.
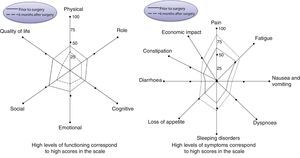
A similar assessment was performed in patients from group B, comparing the same baseline data (when rejecting surgery) with an assessment 6 months later (Fig. 3). A significant deterioration of all items was observed, being more evident for quality of life and pain.
The comparison between the 2 groups 6 months later showed a significant improvement in group A in all the studied items (P<.001) (Table 5).
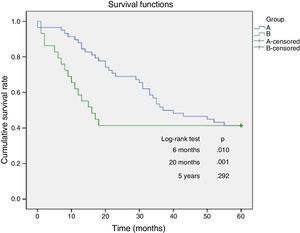
The global survival assessed 6 months later was of 97% in group A and 79% in group B, and the comparison between both groups was statistically significant (P<.01).
The assessment of the mid-term global survival (820 months) was significantly better in group A (P<.01). The survival after 5 years was not significant, and this was probably due to the deaths unrelated to cancer which occurred in group A.
The comparison among patients who survived from both groups 5 years after the analysed parameters still showed a statistically significant difference in favour of patients from group A (P<.01), especially regarding pain, fatigue, nausea, dyspnoea, sleeping disorders, appetite, and economic aspects.
DiscussionRadical cystectomy is the “gold standard” treatment for invasive/locally advanced bladder cancer. Nevertheless, the patient's physical condition and age can influence the treatment selection, and often radical cystectomy is reserved for younger patients without relevant comorbidities.
Holmäng et al. observed in a study of 680 patients with infiltrating bladder cancer that over 60% of patients were not suitable for a radical cystectomy.8
Nowadays, advances in anaesthetic techniques associated with an increase in life expectancy lead us to consider that radical cystectomy is a valid option even in high-risk elderly patients.9
An ASA score ≥III is related with a higher complication rate that can increase according to the type of urinary diversion chosen,10–12 and nowadays, several studies have shown how the simpler urinary diversion and less operative time can significantly reduce the postoperative complications.13,14
Recently, Deliveliotis et al.15 assessed the efficacy and safety of cutaneous ureterostomy in comparison with ileal reconstruction after radical cystectomy in high-risk elderly patients. Authors showed how intraoperative and postoperative complications were more frequent in patients with ileal reconstruction in comparison with the group of cutaneous ureterostomy. The operative time, hospitalisation time, need for blood transfusion, and intensive care were higher in the group of ileal reconstruction. The authors concluded that cutaneous ureterostomy represents a simplified alternative for cutaneous diversion in high-risk elderly patients, and this possibility should be considered as the diversion of choice in this kind of patients.
Another point of view was expressed by Saika et al.,16 who stated that age is not a determinant factor in the choice of the urinary diversion method, and considered that reconstruction with neobladder after cystectomy for bladder cancer is the method of choice even in elderly patients if the baseline conditions of patients allow it.
Some authors state that considerations about the current quality of life are of great importance to assess the results of a surgical intervention and that they are one of the main reasons at the time of choosing the urinary diversion after a radical cystectomy.17
Following this area of research, Gerharz et al. carried out an exhaustive search of MEDLINE to examine the results of urinary diversion with neobladder against continent cutaneous diversion and/or orthotopic substitution of bladder regarding the quality of life or similar concepts. The authors concluded that existing studies are not capable of proving that continent reconstruction after radical cystectomy is a better option than urinary diversion.18
Despite the fact that urinary problems and sexual dysfunction are common to all methods of urinary diversion, Saika et al. published in 2007 that the quality of life related to health seems to be relatively good in elderly patients after radical cystectomy for bladder cancer, regardless of the urinary diversion method chosen.19
We have compared the quality of life and global survival of patients with cystectomy with a control group of 29 patients with infiltrating bladder cancer who rejected the radical cystectomy procedure.
Several preoperative and postoperative items were compared (functional aspects, symptoms, quality of life, and economic impact), and the assessment performed showed a significant improvement in almost all the parameters assessed 6 months after surgery. The comparison with a group of patients with infiltrating bladder cancer who rejected surgery has reinforced the concept that radical cystectomy and simple urinary diversion, such as cutaneous ureterostomy, are a viable option compared to the non-surgical treatment in elderly patients with multiple comorbidities. However, the global survival results confirm a clear short- and mid-term advantage in the treatment group compared to the group without treatment.
Although global survival 5 years later is similar, these results can be justified by a number of deaths related to age and not related to cancer in the group treated with cystectomy. In any case, the quality of life of the survivors in both groups 5 years after surgery is still significantly better in the treatment group.
The low rate of significant postoperative complications and low mortality make the cutaneous ureterostomy an even more beneficial choice, especially for a large group of patients that, in our experience, need several admissions due to haematuria and anaemia. In some cases, surgery was performed to save the patient's life.
The results of this study show that in elderly patients with high surgical risk who have infiltrating bladder cancer, which frequently causes repetitive admissions, the choice of a radical cystectomy in combination with acutaneous ureterostomy represents a valid option due to its benefits regarding quality of life, survival, and complication rates.
In conclusion, although radical cystectomy is considered, even in elderly patients, a viable option for treatment, a cutaneous ureterostomy should be preferred in high-risk elderly patients because it can be performed quickly and easily, reducing the operative time, hospitalisation time and all the complications related to surgery and a prolonged hospital stay.
Our data confirm that cutaneous ureterostomy is well-tolerated in high-risk elderly patients, and the obtained results show a significant improvement in the quality of life, compared to non-treatment, in those patients that otherwise would show major complications and a deteriorated quality of life.
Conflict of InterestThe authors declare that there are no conflicts of interest.
Please cite this article as: Mucciardi G, Macchione L, Galì A, di Benedetto A, Subba E, Pappalardo R, et al. Calidad de vida y supervivencia global en pacientes de alto riesgo tras cistectomía radical con una derivación urinaria simple. Cir Esp. 2015;93:368–374.