To analyse the influence of socioeconomic status on the clinical profile of patients undergoing non-traumatic lower-limb amputation.
MethodsRetrospective study of 697 lower-limb amputee patients in an Angiology and Vascular Surgery Department during a 5-year period. Patients were classified according to their socioeconomic status (low, medium and high). We analysed demographic (age and gender) and clinical variables (cause of amputation, comorbidity, cardiovascular risk factors and amputation level).
ResultsMean age was 70.5 ± 11.9 years, and the median was 72 years. The low socioeconomic status group presented a higher frequency of amputations in men. Cardiovascular risks factors were more frequent in this socioeconomic group, and the difference was statistically significant for diabetes (85.8% low, 69.3% medium, 65% high; P < .01) and obesity (31.4% low, 22.6% medium, 12.5% high, P < .01). Diabetic retinopathy was the only comorbidity with a significant association with low socioeconomic status (21.1% low, 15.3% medium, 12.5% high, P < .03). Regarding the cause for amputation, there was no difference in terms of socioeconomic status. The low socioeconomic level showed a higher frequency of major amputation, which was a significant difference (63.6% low, 41.2% medium, 55% high, P < .04) and a hi+3gher predisposition for this amputation level.
ConclusionsThe low socioeconomic status has been shown to determine an unfavourable vascular risk profile in lower-limb non-traumatic amputees and a higher predisposition of a major amputation. This socioeconomic level demonstrates a negative influence on these patients’ diabetes, obesity and diabetic retinopathy.
Analizar la influencia del nivel socioeconómico (NSE) sobre el perfil clínico del paciente amputado de miembro inferior por causa no traumática.
MétodosEstudio retrospectivo con 697 pacientes amputados de miembro inferior, en un Servicio de Angiología y Cirugía Vascular, durante un periodo de 5 años. Los pacientes fueron divididos según NSE (bajo, medio y alto). Se analizaron variables demográficas (edad y género) y clínicas (causa, comorbilidad, factores de riesgo cardiovascular y nivel de amputación).
ResultadosLa edad media fue 70,5 ± DE 11,9 años y la mediana 72 años. El NSE bajo presentó mayor frecuencia de hombres amputados. Todos los factores de riesgo cardiovascular fueron más frecuentes en este nivel, aunque solo fue estadísticamente significativo en diabetes (85,8% bajo, 69,3% medio, 65% alto; P < 0,01) y obesidad (31,4% bajo, 22,6% medio, 12,5% alto, P < 0,01). La retinopatía diabética fue la única comorbilidad que mostró asociación significativa con el NSE bajo (21,1% bajo, 15,3% medio, 12,5% alto, P < 0,03). No existió diferencia entre los NSE respecto de la causa de amputación. Se observó mayor frecuencia de amputación mayor en el NSE bajo, siendo esta diferencia estadísticamente significativa (63,6% bajo, 41,2% medio, 55% alto, P < 0,04) y una mayor predisposición a este nivel de amputación.
ConclusionesEl NSE bajo determina un perfil de riesgo vascular más desfavorable en los pacientes amputados de miembro inferior por causa no traumático y una mayor predisposición a sufrir amputación mayor. Este NSE muestra una influencia negativa sobre diabetes, obesidad y retinopatía diabética en estos pacientes.
Important advances have been made in the field of vascular surgery in the last decade, both in endovascular techniques and in direct arterial surgery. However, it still has not been possible to reduce the rate of non-traumatic lower extremity amputation (NLEA) in Spain. Currently, Spain is the country with the second highest rate of NLEA due to diabetic foot, only surpassed by the United States.1,2
When we analyse the demographic data from studies in recent decades, we find that these are fundamentally elderly patients who have a higher incidence of peripheral vascular disease, cardiovascular risk factors (CVRF), and concomitant disease.3–9 The longer life expectancy in Spain and vascular disorders typical of the elderly favour an increase in this type of surgical event. However, these circumstances alone do not explain the growing trend of these interventions, and other factors likely play a key role in non-traumatic NLEA amputations.
This study analyses this persistent vascular problem using an approach that is somewhat unusual: the impact of a social variable on the health status of NLEA amputees.
Since the publication by Black,10 the high influence of socioeconomic factors on the health of a population has been recognized. People living in poor social and economic conditions have been shown to be at higher risk of developing non-communicable diseases, and health inequality is still considered a serious problem today.
Following the line of research of certain authors with a social approach to healthcare11,12 the main objective of this study is to determine the influence of a social variable – socioeconomic status – on this type of surgical procedures, (SES), more specifically on the clinical profile of non-traumatic lower extremity amputees, providing unusual insight for this growing vascular problem.
MethodsStudy designA retrospective clinical study was carried out over a 5-year period, from January 1, 2009 to January 1, 2014, including non-traumatic lower extremity amputees from the Angiology and Vascular Surgery Service of the San Cecilio University Hospital in Granada, Spain.
SampleInclusion criteria: adult patients who had undergone non-traumatic lower extremity amputation at the hospital during the study period.
Patients amputated on more than one occasion in the study period were registered for the highest level of amputation, thereby avoiding duplications.
All patients included in the study signed a general informed consent form for the surgical procedure (provided by the hospital) and gave their authorization for data collection for this study by means of a specific informed consent form.
Variables studiedThree types of variables were analysed: demographic (age and gender), clinical (CVRF, cause, comorbidity, level of amputation) and social (SES).
The CVRF analysed included: diabetes, hypertension, dyslipidaemia, smoking and obesity. These data were collected from the patients’ clinical histories, using as a criterion the previous diagnosis of these factors recorded in the clinical history. Smoking was defined as chronic smoking. Obesity was defined with a body mass index equal to or greater than 30 kg/m2.
Patients were classified into 2 groups according to the cause: ischemic and non-ischemic. Within the ischemic cause, a distinction was made between an arteriosclerotic cause (chronic ischemia of NLEA) and a thromboembolic cause (acute ischemia of NLEA). Neuropathic and septic diabetic foot was included within the non-ischemic causes.
The comorbidities we analysed included: ischemic heart disease, arrhythmia, heart failure, kidney failure, chronic obstructive pulmonary disease, and diabetic retinopathy. The previous diagnosis of these diseases recorded in the clinical history was used as a criterion.
Amputations were divided into two categories, in accordance with the classification of the Andalusian Society of Angiology and Vascular Surgery:13 minor amputation (preserving the heel), and major amputation.
To define SES in a practical manner, 3 basic parameters were taken as a reference, which Gottfried14 and Hauser15 argue should always be analysed in any epidemiological study on SES: income, educational level and occupation.
The patients were classified into 3 SES according to a main indicator (average income of the family unit) and 2 complementary indicators (level of studies and occupation): low SES (low income level, no or low educational level, non-skilled worker), medium SES (medium income level, low or medium educational level, variable profession) and high (high income level, medium or high educational level, generally a highly qualified professional).
The main indicator was the average annual income of the family unit, since this economic capacity directly determines the social categories and their different positions, interests and demands. Income was classified into 3 categories: low (€0 to €13 499), medium (€13 500 to €35 999), and high (> €36 000).
The level of studies achieved was used as a complementary socioeconomic indicator and was grouped into 3 categories: high level (university studies), medium level (secondary education) and low level (no studies or primary education).
The third complementary indicator was the individual’s occupation or, if not, the occupation of the main provider of the family unit. The Spanish National Classification of Occupations (CNO-11) was used, which groups professions into 10 categories.16 There is no exact correlation between occupation and SES, due to inter- and intra-group differences in salary level, but the information provided by this indicator may be relevant to classify based on SES.
The data of these parameters were obtained by means of a survey, information from the social worker and the clinical history of each patient. The survey, previously authorized by the Granada Provincial Ethics Committee, was conducted by mail and by telephone.
Statistical analysisThe SPSS version 25.0 program was used. All demographic and clinical characteristics of the patients were compared using the SES. Categorical variables were compared using the chi-square test, while continuous variables were compared using the ANOVA test. An α = .05 was considered the threshold of significance.
A stepwise multivariate logistic regression model was also used to determine the factors associated with major amputation. In addition to age and sex, clinical variables and SES were included in the logistic regression model because they could be related to the need to undergo a major amputation. The main prognostic factors for major amputation were taken as independent variables: age, sex, CVRF, comorbidity and SES.
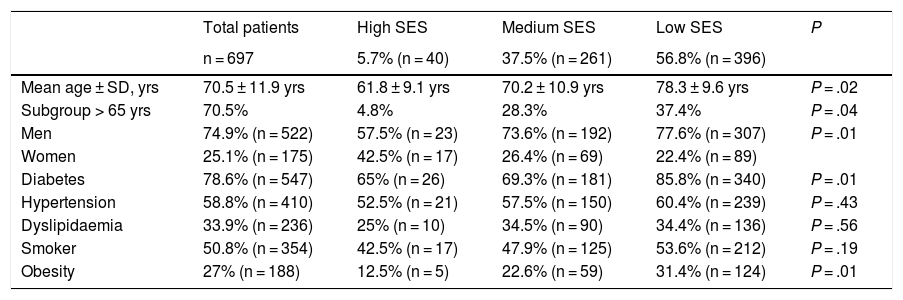
ResultsThe demographic characteristics and distribution of the CVRF according to SES are summarized in Table 1. The study included 697 patients, with a mean age ± standard deviation of 70.5 ± 11.9 years, ranging from 27 to 98 years, and a median of 72 years.
Demographic characteristics and cardiovascular risk factors of the study population, according to socioeconomic status.
| Total patients | High SES | Medium SES | Low SES | P | |
|---|---|---|---|---|---|
| n = 697 | 5.7% (n = 40) | 37.5% (n = 261) | 56.8% (n = 396) | ||
| Mean age ± SD, yrs | 70.5 ± 11.9 yrs | 61.8 ± 9.1 yrs | 70.2 ± 10.9 yrs | 78.3 ± 9.6 yrs | P = .02 |
| Subgroup > 65 yrs | 70.5% | 4.8% | 28.3% | 37.4% | P = .04 |
| Men | 74.9% (n = 522) | 57.5% (n = 23) | 73.6% (n = 192) | 77.6% (n = 307) | P = .01 |
| Women | 25.1% (n = 175) | 42.5% (n = 17) | 26.4% (n = 69) | 22.4% (n = 89) | |
| Diabetes | 78.6% (n = 547) | 65% (n = 26) | 69.3% (n = 181) | 85.8% (n = 340) | P = .01 |
| Hypertension | 58.8% (n = 410) | 52.5% (n = 21) | 57.5% (n = 150) | 60.4% (n = 239) | P = .43 |
| Dyslipidaemia | 33.9% (n = 236) | 25% (n = 10) | 34.5% (n = 90) | 34.4% (n = 136) | P = .56 |
| Smoker | 50.8% (n = 354) | 42.5% (n = 17) | 47.9% (n = 125) | 53.6% (n = 212) | P = .19 |
| Obesity | 27% (n = 188) | 12.5% (n = 5) | 22.6% (n = 59) | 31.4% (n = 124) | P = .01 |
The n parameter has been rounded in all cases to whole numbers, as it indicates the number of individuals of the sample affected according to the variable.
SD: standard deviation; SES: socioeconomic status.
Patients with low SES had a significantly higher mean age compared to the other 2 SES groups (78.3 ± 9.6 years, low; 70.2 ± 10.9 years, medium; and 61.8 ± 9.1 years, high; P<.02) and a higher percentage of patients over the age of 65.
The number of male amputees tripled that of females, and there was also a significant difference between genders, with a higher proportion of amputations in men, within the low SES.
All CVRF occurred more frequently in low SES, but a significant relationship could only be demonstrated in the case of diabetes (85.8% low, 69.3% medium, 65% high; P<.01) and obesity (31.4% low, 22.6% medium, 12.5% high; P<.01), with no observed statistically significant differences between the different SES in the remaining CVRF.
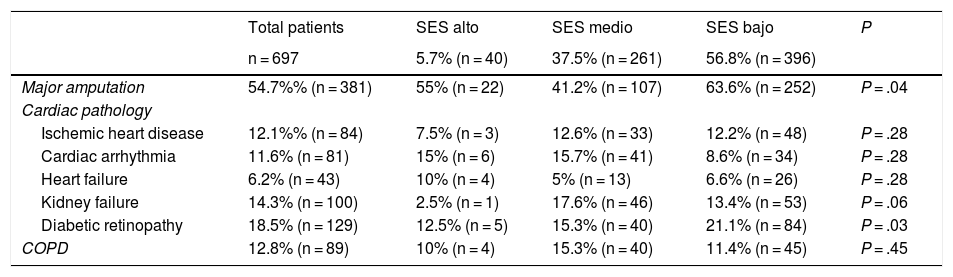
As for the associated comorbidity, there were only significant differences between the different SES in diabetic retinopathy, which was more frequent in low SES (21.1% low, 15.3% medium, 12.5% high; P<.03), as summarized in Table 2. This table also analysed the level of amputation, and a higher proportion of amputation was observed in the low SES group, which was a statistically significant difference (63.6% low, 41.2% medium, 55% high; P<.04).
Comorbidity and major amputation according to socioeconomic level.
| Total patients | SES alto | SES medio | SES bajo | P | |
|---|---|---|---|---|---|
| n = 697 | 5.7% (n = 40) | 37.5% (n = 261) | 56.8% (n = 396) | ||
| Major amputation | 54.7%% (n = 381) | 55% (n = 22) | 41.2% (n = 107) | 63.6% (n = 252) | P = .04 |
| Cardiac pathology | |||||
| Ischemic heart disease | 12.1%% (n = 84) | 7.5% (n = 3) | 12.6% (n = 33) | 12.2% (n = 48) | P = .28 |
| Cardiac arrhythmia | 11.6% (n = 81) | 15% (n = 6) | 15.7% (n = 41) | 8.6% (n = 34) | P = .28 |
| Heart failure | 6.2% (n = 43) | 10% (n = 4) | 5% (n = 13) | 6.6% (n = 26) | P = .28 |
| Kidney failure | 14.3% (n = 100) | 2.5% (n = 1) | 17.6% (n = 46) | 13.4% (n = 53) | P = .06 |
| Diabetic retinopathy | 18.5% (n = 129) | 12.5% (n = 5) | 15.3% (n = 40) | 21.1% (n = 84) | P = .03 |
| COPD | 12.8% (n = 89) | 10% (n = 4) | 15.3% (n = 40) | 11.4% (n = 45) | P = .45 |
The n has been rounded in all cases to whole numbers, as this indicates the number of individuals of the sample affected according to the variable.
COPD: chronic obstructive pulmonary disease; SES: socioeconomic status.
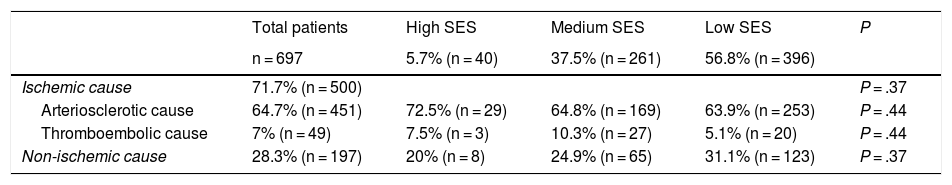
The analysis of the causes of amputation is summarized in Table 3, where no difference is observed between the different SES in terms of the general causes: ischemic and non-ischemic.
Distribution of the causes for amputation of the study population, according to socioeconomic level.
| Total patients | High SES | Medium SES | Low SES | P | |
|---|---|---|---|---|---|
| n = 697 | 5.7% (n = 40) | 37.5% (n = 261) | 56.8% (n = 396) | ||
| Ischemic cause | 71.7% (n = 500) | P = .37 | |||
| Arteriosclerotic cause | 64.7% (n = 451) | 72.5% (n = 29) | 64.8% (n = 169) | 63.9% (n = 253) | P = .44 |
| Thromboembolic cause | 7% (n = 49) | 7.5% (n = 3) | 10.3% (n = 27) | 5.1% (n = 20) | P = .44 |
| Non-ischemic cause | 28.3% (n = 197) | 20% (n = 8) | 24.9% (n = 65) | 31.1% (n = 123) | P = .37 |
The n parameter has been rounded in all cases to whole numbers, as this indicates the number of individuals of the sample affected according to the variable.
SES: socioeconomic status.
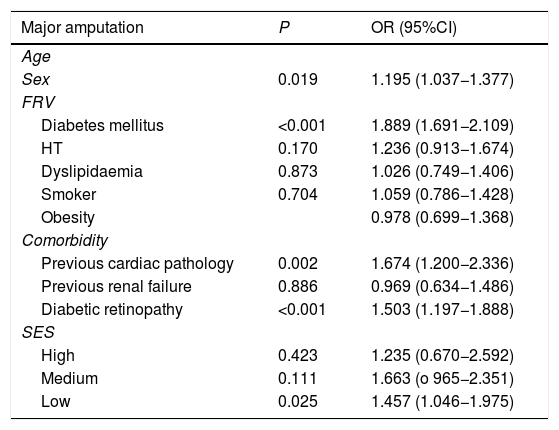
Table 4 shows the results of the multivariate logistic regression study carried out, where the variables that most favour the possibility of undergoing a major amputation include: female gender, diabetes, previous heart disease, diabetic retinopathy and a low SES, which were independent predictors of major amputation.
Stepwise logistic regression model with predictive character of the practice of a major amputation of the study population.
| Major amputation | P | OR (95%CI) |
|---|---|---|
| Age | ||
| Sex | 0.019 | 1.195 (1.037−1.377) |
| FRV | ||
| Diabetes mellitus | <0.001 | 1.889 (1.691−2.109) |
| HT | 0.170 | 1.236 (0.913−1.674) |
| Dyslipidaemia | 0.873 | 1.026 (0.749−1.406) |
| Smoker | 0.704 | 1.059 (0.786−1.428) |
| Obesity | 0.978 (0.699−1.368) | |
| Comorbidity | ||
| Previous cardiac pathology | 0.002 | 1.674 (1.200−2.336) |
| Previous renal failure | 0.886 | 0.969 (0.634−1.486) |
| Diabetic retinopathy | <0.001 | 1.503 (1.197−1.888) |
| SES | ||
| High | 0.423 | 1.235 (0.670−2.592) |
| Medium | 0.111 | 1.663 (o 965−2.351) |
| Low | 0.025 | 1.457 (1.046−1.975) |
95% CI: 95% confidence interval; SES: socioeconomic status; OR: odds ratio.
This retrospective descriptive clinical study on lower extremity amputation due to non-traumatic causes in a public hospital Angiology and Vascular Surgery Service is representative of how patient SES is associated with health status. Specifically, it shows how a low SES favours a more unfavourable clinical profile in the patient with NLEA, with a higher frequency of CVRF and a greater probability of major amputation.
Most of the research on the relationship between SES and health status has been conducted with mortality data, but there is clear evidence about the difference in the frequency of health problems between different socioeconomic groups.
A low SES is associated with a wide range of health problems. This negative relationship seems to appear consistently in terms of chronic problems, such as diabetes, obesity or early mortality.17,18
The association of a lower social class with higher morbidity and mortality due to chronic disease is a well-known fact. However, socioeconomic class is currently not considered as a risk factor for these diseases, despite the fact that the results of the latest research18,19 support the contrary.
The study presented here concurs with the publications by Stringhini et al.,19,20 who concluded that socioeconomic factors should be included among the risk factors influencing public health.
When it comes to facing a transcendental surgical procedure such as lower extremity amputation, there is a tendency to have an individualistic view of genetic factors or life habits, without taking into account the circumstances of the patient’s social group. The results of this study reinforce the concept of a negative association between vascular risk and low SES, specifically in the subgroup of amputee patients, and support the idea that SES should be considered a risk factor when contemplating this type of surgical intervention.
This study also demonstrates the association between 2 CVRF – diabetes and obesity – and the low SES of the amputee patient. This result agrees with scientific publications stating that people with low SES generally have more health problems, are more overweight and more frequently have diabetes.21,22
Diabetes, which is considered ‘an epidemic of our time’, is a fundamental vascular risk factor, accounting for 70% of lower extremity (LE) amputations. Diabetic patients have a risk of LE amputation that is 15–45 times higher than non-diabetic patients.23–25
It is relevant that this study found a higher frequency of diabetes, a determining risk factor in this type of surgical event, in the lowest socioeconomic stratum.
Currently, efforts are being joined against this CVRF in order to reduce the incidence of NLEA through the implementation of multidisciplinary diabetic foot teams.26,27 Despite the positive results of these multidisciplinary units, these are not quite as optimal as they should be. It is a multi-focus yet more individual patient approach, but once again a measure lacking a global vision of this health problem, as it is a prevention strategy that does not consider the important impact of socioeconomic status on the clinical profile of amputee patients, as this clinical study shows.
In accordance with a recent Spanish study,28 this study also confirms the influence of low SES on major lower extremity amputation, showing more frequency of this level of amputation and greater predisposition in patients from this socioeconomic stratum.
In Spain, the fact that SES is still not considered a definite risk factor for certain chronic diseases, despite the results of scientific publications providing conflicting results, may be due to the obvious lack of information and the lack of health statistics by social class.
When it comes to associating a vascular problem, such as NLEA, with a social factor and more specifically with the patient’s SES, studies and statistics, at the national and international level, the data is also very limited.
The distribution of social classes in Spain has changed considerably in recent years, highlighting the increase in the low SES stratum.29–31 In accordance with the conclusions of the studies previously mentioned in this paper, as well as the results of our study, it is precisely this growing stratum that has a negative association with patient health status, which is undoubtedly a cause for concern.
LimitationsAs this is a cross-sectional observational study, there has been no follow-up, and the relevant information has been limited to the specific period of the study. The association between variables has been described, but it has not been possible to determine causality.
ConclusionsThe results of this study reinforce the concept that SES is a determinant variable in patient health status. This study shows that low SES determines a more unfavourable vascular risk profile in a specific subgroup of patients with vascular disease, who are non-traumatic lower extremity amputees. A negative association between low SES and 2 CVRF, diabetes and obesity, is also demonstrated in this subgroup of patients, as well as a greater predisposition for major amputation.
These findings support the theories that SES is a fundamental risk factor to include in the study of patient health problems, especially chronic ones. Specifically, this study confirms the important role played by low SES as a risk factor to consider in lower extremity amputation due to non-traumatic causes, a surgical intervention that currently presents a troubling growing trend.
It is possible that, by considering this social variable as a risk factor for this type of surgical procedure, new healthcare strategies could be proposed for primary and secondary prevention, aimed primarily at the most underprivileged social classes, in an attempt to stop the current increase in these surgical events.
Conflict of interestsThe authors declare that they have no conflict of interest.
FundingThis study has received no specific funding from public, commercial, or non-profit organizations.
Please cite this article as: Gutiérrez Fernández M, Carrasco de Andrés D, Salmerón Febres LM, González Herrera L, Jiménez Brobeil S. Impacto del nivel socioeconómico sobre el perfil del paciente amputado de miembro inferior por causa no traumática. Cir Esp. 2021;99:55–61.