Choledochal cysts (CC) are rare congenital dilatations of the extrahepatic bile duct (EBD) occasionally associated with involvement of the intrahepatic segment. Malignant degeneration is the most feared complication due to its silent presentation and prognostic implications.1
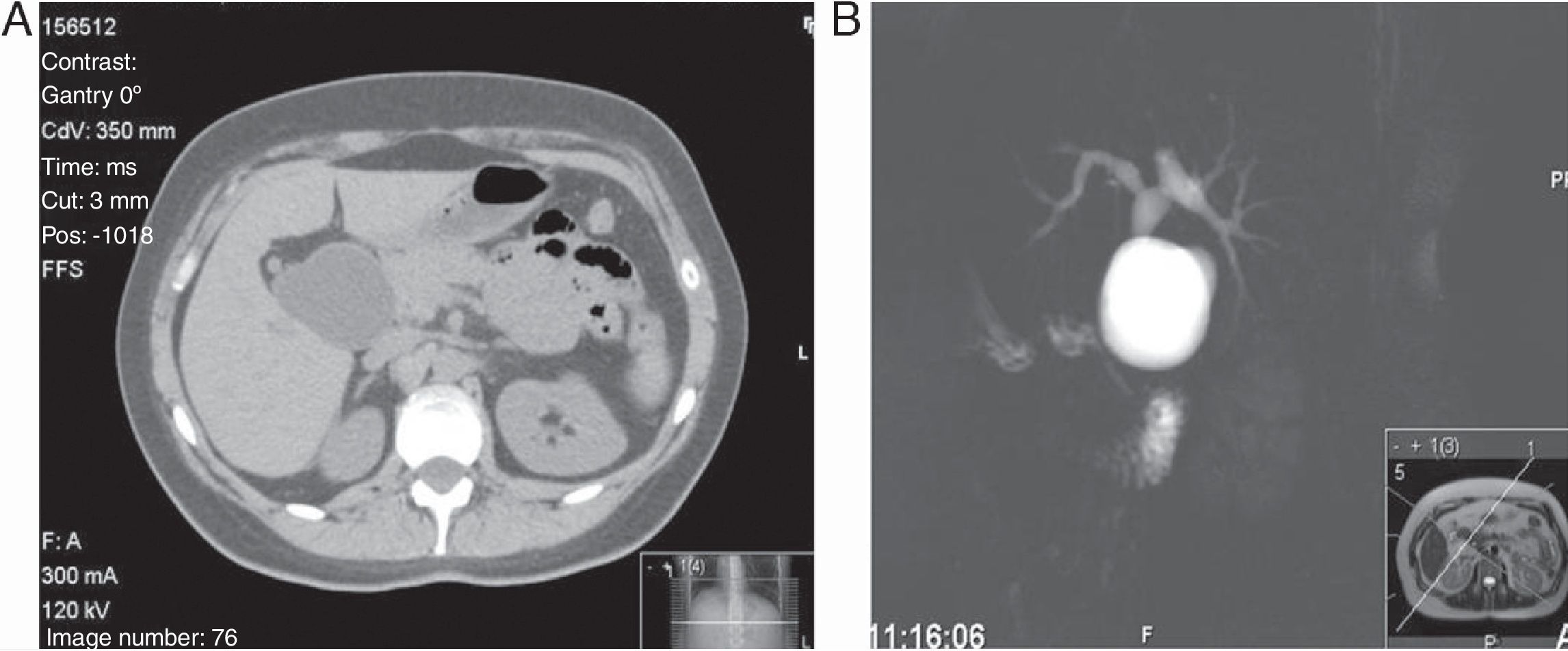
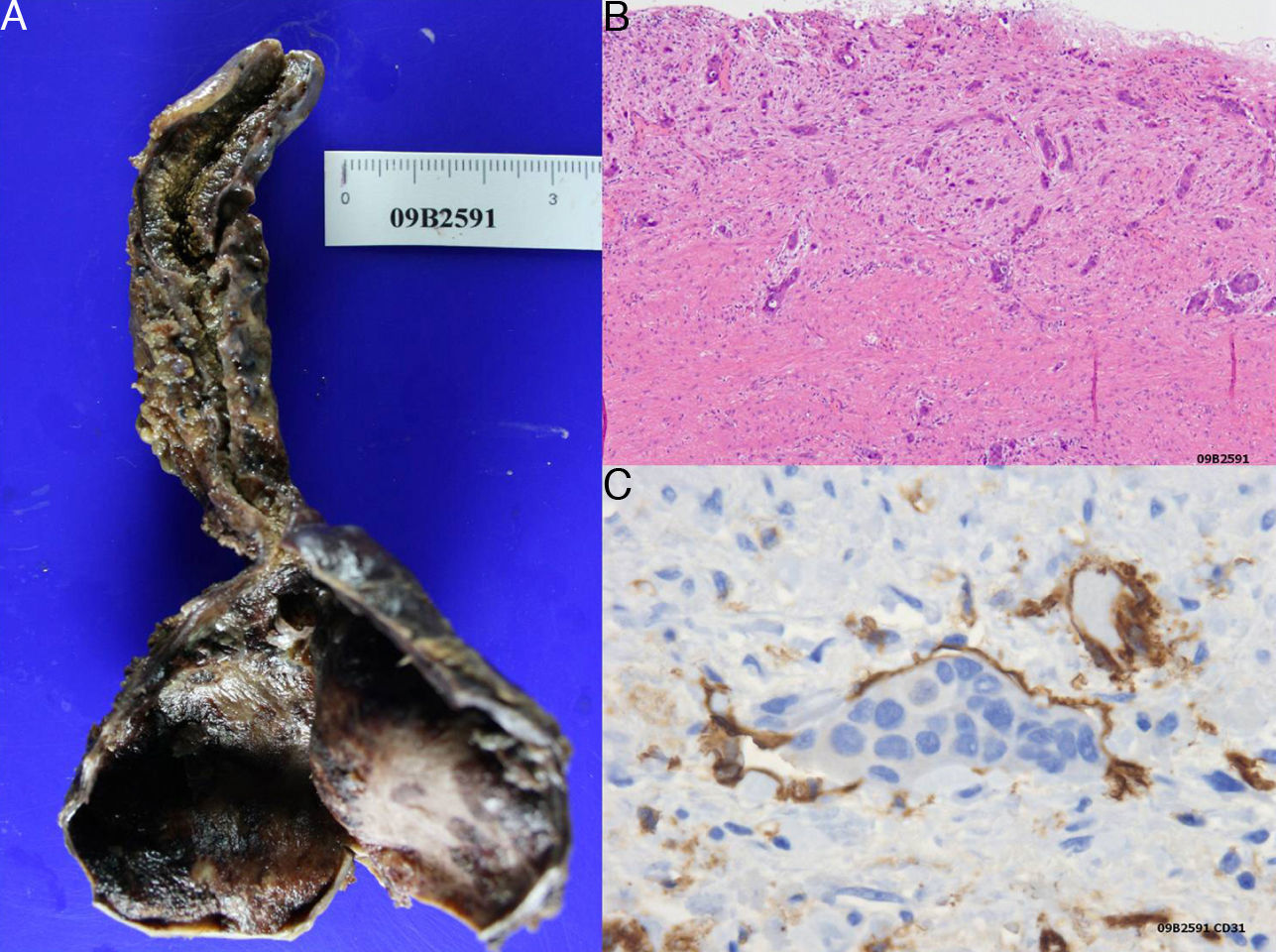
A 38-year-old female was studied because of epigastric pain, nausea, and vomiting. Blood tests showed normal amylase and liver function tests and an abdominal ultrasound scan showed dilatation of the EBD. A CT scan and an MRI cholangiography confirmed the saccular dilation associated with 4 small biliary cysts of the intrahepatic bile duct (Fig. 1). The patient was operated on, and a dilatation of 3cm was found from the confluence of hepatic biliary radicals which extended to 1cm of the intrapancreatic bile duct. With the diagnosis of a CC type Ia, the resection of the whole EBD, cholecystectomy and reconstruction with Roux-en-Y hepaticojejunostomy were performed. The macroscopic histological study (Fig. 2A) reported a CC wall with an erosive appearance without tumour projections and, in continuity, an atrophic gallbladder. Microscopically, traces of malignant cells were observed infiltrating the wall (Fig. 2B). The lymphatic permeation of the neoplasm was demonstrated by the marker CD-31, which confirmed the intravascular location of the tumour cells (Fig. 2C).
The patient did not accept adjuvant therapy and is currently asymptomatic 24 months later.
Cystic dilation of the biliary tract, described by Vater in 1723, has an incidence 10 times higher in Eastern countries and is more common in women (3–4/1).1,2
An anomalous union of the pancreatic and bile ducts seems to be the main aetiological factor. According to this theory, a congenital malformation of the bile duct end and the duct of Wirsung in the duodenum forming a long, common canal would favour the reflux of proteolytic enzymes, producing dilation and malignant degeneration in the bile duct wall. Recently, hypotheses based on distal obstruction due to sphincter dysfunction or the presence of abnormal ganglion cells in the bile duct have emerged.3,4
The Alonso-Lej morphological classification, modified by Todani, distinguishes 5 types of CC: type I (60%) is a dilation of the extrahepatic biliary tract which can be cystic (Ia), segmentary (Ib) or fusiform (Ic). Type II or bile duct diverticulum and type III or choledochocele are rarer (2%–5%). Type IV (30%) displays multiple cystic dilatations in the whole duct (IVa) or only of the extrahepatic biliary tract (IVb). Lastly, type V or Caroli's disease is a cystic involvement of the intrahepatic bile ducts that may be diffuse or segmental.1,4,5
Clinically, they normally manifest during the first decade of life.1,5,6 Around 80% of patients will develop complications such as calculus, pancreatitis, recurrent cholangitis, cystic rupture, secondary biliary cirrhosis or malignant degeneration.6,7
CC carries a risk of developing carcinoma that is 20–30 times higher than the normal population, and as such it is considered to be a premalignant condition, especially in types I and IV. The most common cancer is adenocarcinoma (73%–84%) followed by anaplastic carcinoma (10%), undifferentiated (5%–7%) and squamous cell (5%). It is predominantly located in the EBD and gallbladder and in unusual cases develops in intrahepatic and pancreatic segments. Its incidence increases with age from 0.7% in the first decade to 14% at 20 years old, with a mean survival of 6–21 months. In the presence of the anomalous union of the pancreatic and bile duct union without dilation of the duct, the place with the highest stasis is the gallbladder with a carcinoma incidence of 25%–40%.7–9
Faced with the appearance of suggestive symptoms, the first diagnostic technique should be ultrasound.7 CT scan is preferable in cases of intrahepatic dilatations or with distal involvement and in some cases may establish the existence of the malignancy showing a cystic mass or an increased thickness of the cystic wall. MRI cholangiography is the gold standard technique with close to 100% sensitivity and it can precisely define any anomaly in the biliopancreatic union. Lastly, ERCP is not used nowadays as a diagnostic technique and is reserved for therapeutic purposes (CC type III).7,10
Treatment depends on the type of cyst; complete resection of the bile duct including the intrapancreatic bile duct, cholecystectomy and reconstruction through Roux-en-Y hepaticojejunostomy is the treatment of choice. For type II, extraction of the cyst and cholecystectomy is advised. In type III endoscopic sphincterotomy in cysts under 2cm may be effective given their low rate of malignisation, while in the rest, transduodenal resection with reimplantation of the pancreatic duct is necessary. The management of type V cysts depends on the extension of the disease and the presence of liver damage.10 The only curative option for biliary cancer is surgery. The following procedures are recommended: radical exeresis of the tract, generalised vascular “cleaning” and a radical pancreatoduodenectomy if it involves the intrapancreatic duct and a partial hepatectomy when the tumour is located in the intrahepatic bile duct dilatations.9 In locally resectable tumours without distant metastasis an en bloc liver, gallbladder, and EBD resection may be attempted, followed by liver transplantation. Adjuvant treatment with gemcitabine and cisplatin seems promising, as well as radiotherapy in selected cases. The follow-up should be strict since recurrences reach 0.7%.10
Please cite this article as: Pastor Pérez P, et al. Carcinoma de la vía biliar sobre quiste de colédoco. Cir Esp. 2013;91:57–9.