Cholelithiasis is the most common hospital diagnosis of the digestive system, and its treatment, if symptomatic, is laparoscopic cholecystectomy. There is a growing need for comprehensive determination of postoperative outcomes and the efficiency of healthcare facilities. The “textbook outcome”(TO) indicates the quality of care commonly used in oncological procedures, obtained by adding several postoperative parameters, which informs whether a perfect result has been obtained. The main objective of this study is to determine the TO for cholecystectomy and to see the factors that influence its achievement.
MethodsRetrospective observational unicentric cohort study on patients who underwent cholecystectomy between 2018–2020. We defined TO as those patients who met the following premises: Clavien-Dindo complications < III, postsurgical stay less than the 75th percentile (<3 days), and no readmissions or mortality in the first ninety days. Perioperative characteristics were analyzed, and the patients were divided into two groups according to whether or not they achieved TO. We defined criteria for difficult cholecystectomy according to the operative report.
ResultsThe percentage of TO was 72% (342/475) (82.6% in elective surgery and 60.5% in urgent surgery). The univariate analysis showed that the following factors are associated with achieving TO: female sex, age <63 years, ASA risk < III, elective surgery, laparoscopic approach, and not difficult cholecystectomy. After multivariate analysis ASA < III (OR 2.39 CI95% 1.37–4.16), elective surgery (OR 2.77 CI95% 1.64–4.67), laparoscopic approach (OR 5.71 CI95% 2.89–11.30) and not to be difficult cholecystectomy (OR 0.42 CI95% 0.259–0.71) remained statistically significant.
ConclusionsThe TO is a healthcare quality tool that is simple to perform, easily interpretable, and helpful for evaluating quality in healthcare and comparing centers. It applies not only to oncological procedures but also to cholecystectomy.
La colelitiasis es el diagnóstico hospitalario más común del sistema digestivo, y su tratamiento si es sintomática es la colecistectomía laparoscópica. Existe una necesidad creciente de una determinación exhaustiva de los resultados postoperatorios y la eficiencia de los centros sanitarios. El “textbook outome”(TO), es un indicador de calidad asistencial utilizado habitualmente en procedimientos oncológicos, obtenido al sumar varios parámetros postoperatorios, que informa si se ha obtenido un resultado perfecto. El objetivo principal de este estudio es determinar el TO para colecistectomía, y ver los factores que influyen en su consecución.
MétodosEstudio observacional unicéntrico de cohortes retrospectivo sobre pacientes intervenidos de colecistectomía entre 2018-2020. Definimos TO como aquellos pacientes que cumplieron las siguientes premisas: complicaciones Clavien-Dindo < III, estancia postquirúrgica menor del percentil 75(<3 días), y no reingresos ni mortalidad en los primeros noventa días. Se analizaron las características perioperatorias, dividiendo los pacientes en dos grupos según la consecución o no de TO. Definimos unos criterios de colecistectomía difícil según informe operatorio.
ResultadosEl porcentaje de TO global fue 72% (342/475) (82.6% en cirugía programada y 60.5% en cirugía urgente). El análisis univariante demostró que los siguientes factores se asocian a la consecución de TO: sexo femenino, edad<63 años, riesgo ASA < III, cirugía electiva, abordaje laparoscópico y no ser colecistectomía difícil. Tras el análisis multivariante se mantiene significativo el riesgo ASA < III (OR 2.39 IC95% 1.37–4.16), la cirugía electiva (OR 2.77 IC95% 1.64-4.67), el abordaje laparoscópico (OR 5.71 IC95% 2.89-11.30) y no ser colecistectomía difícil (OR 0.42 IC95% 0.259-0.71).
ConclusionesEl TO, es una herramienta de calidad asistencial sencilla de realizar, fácilmente interpretable y útil para evaluar la calidad en la atención sanitaria y comparar centros, aplicable no solo en procedimientos oncológicos sino también en la colecistectomía.
Gallbladder diseases are the most common hospital diagnosis in gastroenterology, with high annual health care costs.1 Among these, the most frequent is biliary lithiasis, whose prevalence in the general population is 20%, with 50% being asymptomatic, but with theoretical potential to cause severe clinical symptoms.2
Cholecystectomy as a treatment for biliary lithiasis is a procedure frequently performed in surgical units. The laparoscopic approach has become the gold standard, since it is feasible, safe, with very low morbidity and a mortality rate of less than 0.1%.3
Today, there is a growing demand, both in the health care sector and among the population itself, for improving knowledge of the results, the effectiveness and efficiency of health centres, and to establish which hospitals provide exemplary care and results. In 2013, Kolfschoten et al.4 proposed a new tool termed the textbook outcome (TO), as a new indicator of quality of care. This tool, which is currently being used mainly in oncological procedures, is obtained by adding together several parameters for desired short-term results in postoperative care: no serious postoperative complications, no prolongation of postoperative hospital stay, no mortality and no readmissions. To be classified as a TO, all the aforementioned parameters must be met, obtaining the percentage of patients for whom all the ideal postoperative health outcomes have been achieved.4
The main objective of this study was to determine the TO for cholecystectomy globally, as well as the characteristics and risk factors that influence its achievement, since there is very little information on determining this in cholecystectomy patients. As secondary objectives, we have divided the sample according to cases of emergency or scheduled surgery to study the differences.
Material and methodsA single-centre retrospective study of patients undergoing cholecystectomy between January 2018 and December 2020 in a tertiary hospital. Patient data was obtained from hospital medical records and clinical reports. Approval of the study was carried out by the hospital's research, ethics, and biosafety committees. (CEIM PI2022-093).
The inclusion criteria were as follows: patients undergoing cholecystectomy in the study period. Exclusion criteria were considered: cholecystectomy combined with other surgical procedures, active oncological disease of any kind at the time of operation, findings of malignancy in the surgical specimen, and scheduled readmissions in the first ninety days postoperatively for other unrelated pathologies.
Several variables were recorded after analysing the histories of the selected patients:
- -
Preoperative variables or data were collected on age, sex, and comorbidities of the patient, according to the American Anesthesiologists Association (ASA) scale,5 existing type of biliary pathology, and previous ERCP.
- -
The following surgical data was gathered: biliary pathology requiring cholecystectomy (cholelithiasis, cholecystitis, pancreatitis of biliary origin, cholangitis of biliary origin, simple choledocholithiasis, gallbladder polyps and others), the surgery performed, the type of surgery (emergency or scheduled), the route of approach (open/laparoscopic/conversion) and the technical difficulty of the surgery, taken from the surgical protocol followed by the surgeon (description indicative of a difficult surgery, depending on the appearance of one or more of the following intraoperative findings: difficult dissection of the hepatic hilum; scleroatrophic or gangrenous vesicle; plastron or perivesicular abscess; firm adhesions; poor visualisation of the structures of the hepatocystic triangle; unusual anatomy of the cystic duct; Mirizzi syndrome; surgical bleeding with the need for haemostatics and/or drainage, or any other specific characteristic of the intraoperative period that increased the usual operating time or difficulty of the surgery).
- -
Postoperative outcomes: postoperative complications, following the Clavien-Dindo classification6; readmissions, following the classification of Rana et al.7 (causes arising from biliary surgery, non-biliary surgery, and non-surgical causes) taking ninety days or mortality as the cut-off point.
TO is defined as patients who met the following conditions: complications of less than III according to the Clavien-Dindo classification (defined as: any complication requiring a surgical, radiological, or endoscopic procedure; serious complications requiring admission to the ICU; or death), postoperative stay below the 75th percentile (<3 days), and no readmissions or mortality in the first ninety days after surgery, setting this limit of ninety days to take into account any complications and late readmissions.
The statistical analysis was run using the IBM® SPSS 25 Statistics programme. The non-normal distribution of quantitative variables was verified using the Kolmogorov-Smirnov normality test, which were presented as median and interquartile range. To facilitate statistical analysis, quantitative variables were recoded into categorical qualitative variables, using the median as a cut-off point. As regards the qualitative variables, these were expressed in the form of percentages. Two cohorts were created in terms of achievement of TO. For comparison of the groups, the Chi-square (χ²) statistical test or Fisher’s exact test was used, through the creation of contingency tables. Finally, a logistic regression analysis (univariate and multivariate analyses) was run to predict the outcome of our categorical variables, based on other independent or predictor variables, to thus detect risk or protective factors for the probability of occurrence of an event, which we express in the form of Odds Ratio (OR) and their corresponding 95% confidence intervals (95% CI). A degree of significance of p < 0.05 was considered as statistically significant.
ResultsA total of 535 patients were reviewed during the period selected. After applying the exclusion criteria, our sample was finally composed of 475 patients.
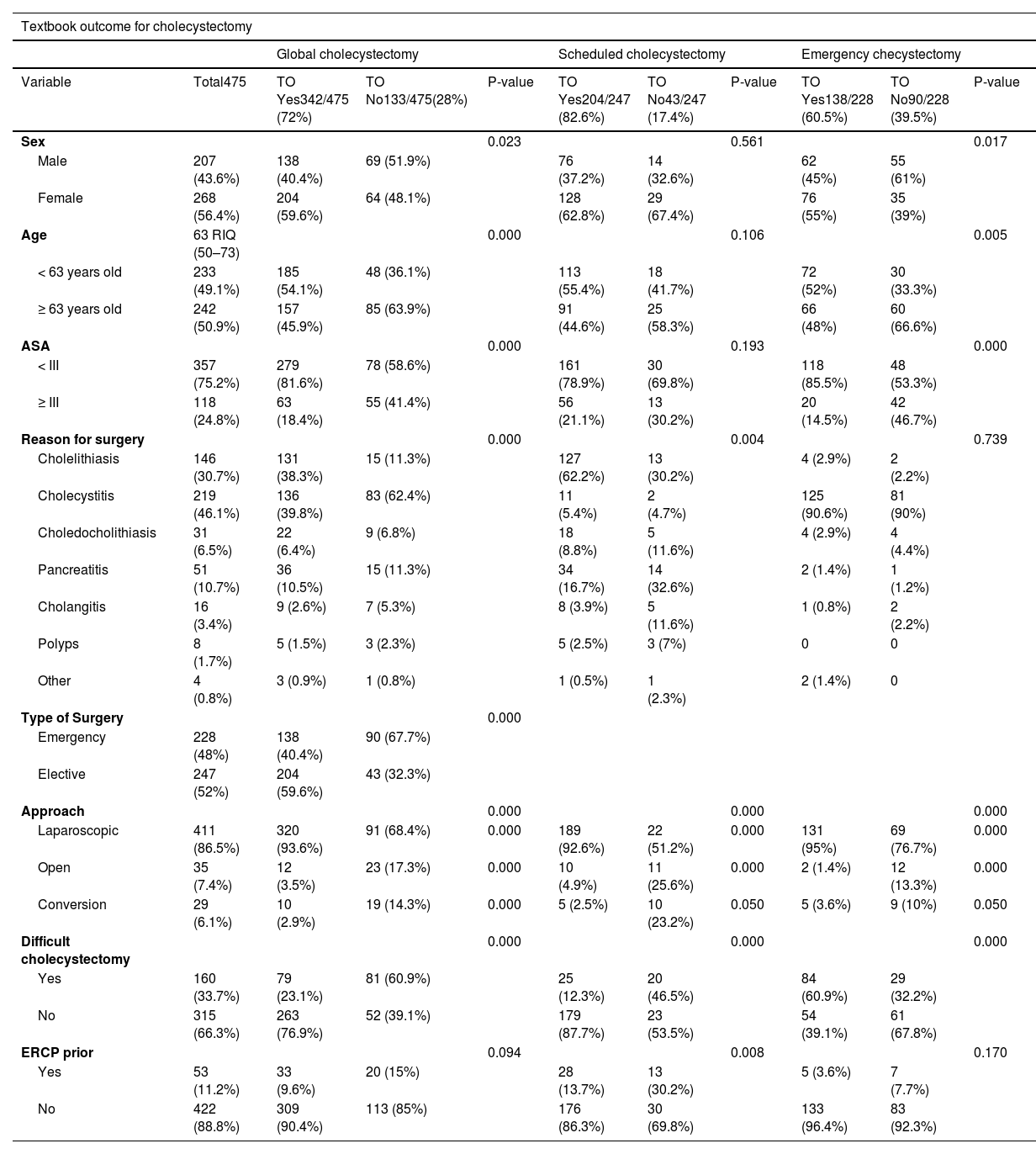
Regarding the characteristics of the sample (Table 1), it was made up of 207 men (43.6%) and 268 women (56.4%). The median age of the patients was 63 years (interquartile range (IQR) 50–73), with a minimum age of 17 years and a maximum of 93 years. According to the ASA scale, most patients (48%) had an ASA II, and up to 75.2% had an ASA below III. The most frequent pathology for which cholecystectomy was indicated was cholecystitis (46.1%), followed by cholelithiasis (30.7%). The type of surgery performed was elective in 52% of the cases. The most frequently used approach was laparoscopic in 86.5% of the procedures. The total conversion rate was 6.1%. A total of 53 patients (11.2%) underwent ERCP prior to cholecystectomy. Of the total, 160 patients (33.7%) had a difficult cholecystectomy according to our classification.
Baseline characteristics of the sample and comparison depending on achievement of TO after cholecystectomy (overall programmed and emergency).
| Textbook outcome for cholecystectomy | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Global cholecystectomy | Scheduled cholecystectomy | Emergency checystectomy | ||||||||
| Variable | Total475 | TO Yes342/475 (72%) | TO No133/475(28%) | P-value | TO Yes204/247 (82.6%) | TO No43/247 (17.4%) | P-value | TO Yes138/228 (60.5%) | TO No90/228 (39.5%) | P-value |
| Sex | 0.023 | 0.561 | 0.017 | |||||||
| Male | 207 (43.6%) | 138 (40.4%) | 69 (51.9%) | 76 (37.2%) | 14 (32.6%) | 62 (45%) | 55 (61%) | |||
| Female | 268 (56.4%) | 204 (59.6%) | 64 (48.1%) | 128 (62.8%) | 29 (67.4%) | 76 (55%) | 35 (39%) | |||
| Age | 63 RIQ (50–73) | 0.000 | 0.106 | 0.005 | ||||||
| < 63 years old | 233 (49.1%) | 185 (54.1%) | 48 (36.1%) | 113 (55.4%) | 18 (41.7%) | 72 (52%) | 30 (33.3%) | |||
| ≥ 63 years old | 242 (50.9%) | 157 (45.9%) | 85 (63.9%) | 91 (44.6%) | 25 (58.3%) | 66 (48%) | 60 (66.6%) | |||
| ASA | 0.000 | 0.193 | 0.000 | |||||||
| < III | 357 (75.2%) | 279 (81.6%) | 78 (58.6%) | 161 (78.9%) | 30 (69.8%) | 118 (85.5%) | 48 (53.3%) | |||
| ≥ III | 118 (24.8%) | 63 (18.4%) | 55 (41.4%) | 56 (21.1%) | 13 (30.2%) | 20 (14.5%) | 42 (46.7%) | |||
| Reason for surgery | 0.000 | 0.004 | 0.739 | |||||||
| Cholelithiasis | 146 (30.7%) | 131 (38.3%) | 15 (11.3%) | 127 (62.2%) | 13 (30.2%) | 4 (2.9%) | 2 (2.2%) | |||
| Cholecystitis | 219 (46.1%) | 136 (39.8%) | 83 (62.4%) | 11 (5.4%) | 2 (4.7%) | 125 (90.6%) | 81 (90%) | |||
| Choledocholithiasis | 31 (6.5%) | 22 (6.4%) | 9 (6.8%) | 18 (8.8%) | 5 (11.6%) | 4 (2.9%) | 4 (4.4%) | |||
| Pancreatitis | 51 (10.7%) | 36 (10.5%) | 15 (11.3%) | 34 (16.7%) | 14 (32.6%) | 2 (1.4%) | 1 (1.2%) | |||
| Cholangitis | 16 (3.4%) | 9 (2.6%) | 7 (5.3%) | 8 (3.9%) | 5 (11.6%) | 1 (0.8%) | 2 (2.2%) | |||
| Polyps | 8 (1.7%) | 5 (1.5%) | 3 (2.3%) | 5 (2.5%) | 3 (7%) | 0 | 0 | |||
| Other | 4 (0.8%) | 3 (0.9%) | 1 (0.8%) | 1 (0.5%) | 1 (2.3%) | 2 (1.4%) | 0 | |||
| Type of Surgery | 0.000 | |||||||||
| Emergency | 228 (48%) | 138 (40.4%) | 90 (67.7%) | |||||||
| Elective | 247 (52%) | 204 (59.6%) | 43 (32.3%) | |||||||
| Approach | 0.000 | 0.000 | 0.000 | |||||||
| Laparoscopic | 411 (86.5%) | 320 (93.6%) | 91 (68.4%) | 0.000 | 189 (92.6%) | 22 (51.2%) | 0.000 | 131 (95%) | 69 (76.7%) | 0.000 |
| Open | 35 (7.4%) | 12 (3.5%) | 23 (17.3%) | 0.000 | 10 (4.9%) | 11 (25.6%) | 0.000 | 2 (1.4%) | 12 (13.3%) | 0.000 |
| Conversion | 29 (6.1%) | 10 (2.9%) | 19 (14.3%) | 0.000 | 5 (2.5%) | 10 (23.2%) | 0.050 | 5 (3.6%) | 9 (10%) | 0.050 |
| Difficult cholecystectomy | 0.000 | 0.000 | 0.000 | |||||||
| Yes | 160 (33.7%) | 79 (23.1%) | 81 (60.9%) | 25 (12.3%) | 20 (46.5%) | 84 (60.9%) | 29 (32.2%) | |||
| No | 315 (66.3%) | 263 (76.9%) | 52 (39.1%) | 179 (87.7%) | 23 (53.5%) | 54 (39.1%) | 61 (67.8%) | |||
| ERCP prior | 0.094 | 0.008 | 0.170 | |||||||
| Yes | 53 (11.2%) | 33 (9.6%) | 20 (15%) | 28 (13.7%) | 13 (30.2%) | 5 (3.6%) | 7 (7.7%) | |||
| No | 422 (88.8%) | 309 (90.4%) | 113 (85%) | 176 (86.3%) | 30 (69.8%) | 133 (96.4%) | 83 (92.3%) | |||
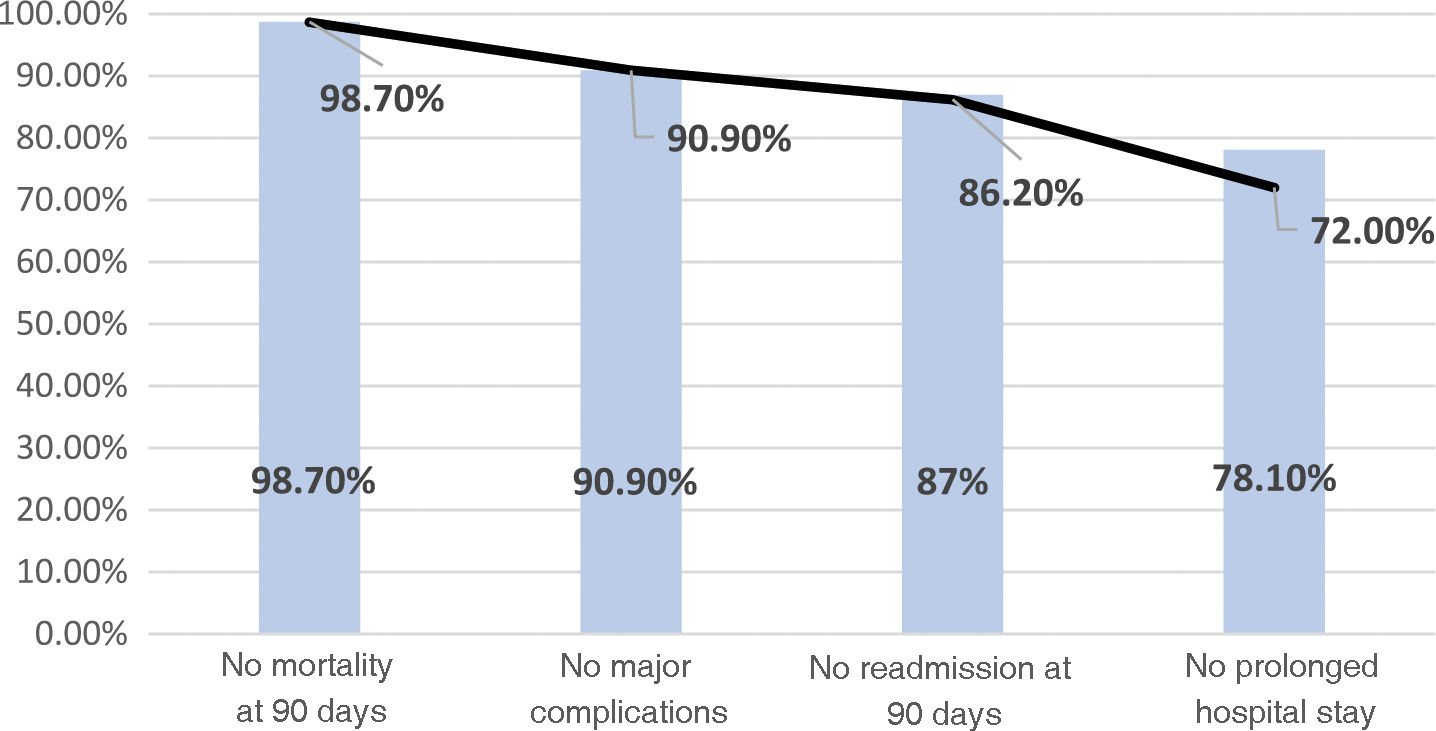
Regarding postoperative outcomes, 43 patients (9.1%) had major complications: ≥ IIIa Clavien-Dindo. The 75th percentile of the postoperative stay was 3 days, with a stay of less than 3 days for 78.1% of the patients. The ninety-day readmission rate was 13.1%, with a mortality rate of 1.3%.
In our series, we were able to classify 342 patients (72%) as TO (Fig. 1). As we can see, the patients most likely to achieve these goals were female (59.6% women vs. 40.4% men), under 63 years old (54.1%) and with an ASA < III (81.6%). With respect to the reason for the indication of surgery, we see that the greatest difference was found in terms of acute cholecystitis; 62.4% of the patients who did not achieve a TO were operated on for this indication. On the other hand, surgery performed as emergencies influenced the failure to achieve a TO (40.4% TO in emergencies vs 59.6% TO in elective surgery).
TO chart. We lost 6 patients (1.3%) due to mortality. Cumulative TO after major complications: 90.9% (we lost 33 more patients, 7.8%). Cumulative TO with no readmissions at 90 days: 86.2% (we lost 22 more patients: 4.7%). Cumulative TO after no prolonged stay: 72% (we lost 67 more patients: 14.2%).
Looking now at intraoperative variables, the laparoscopic approach was applied in 93.6% of TOs and, as regards our classification of difficult cholecystectomy, when the surgical procedure was classified as difficult, TOs were achieved by only 23.1% of patients. The only variable for which no statistically significant differences were found between the two groups was the performance of an ERCP prior to the surgery.
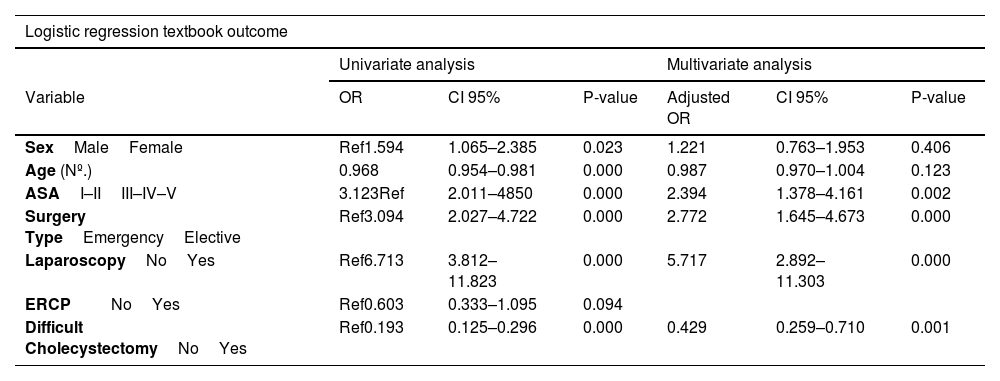
When we analysed these pre- and intraoperative variables by running logistic regression (Table 2) to establish which factors should be classified as risk or protective factors when achieving a TO result, we saw, in a first univariate analysis, that female sex, younger age, ASA < III, elective surgery, laparoscopic approach and the presence of a “not difficult” cholecystectomy were protective factors for achieving this ideal result, or, in other words, these characteristics made them more likely to achieve the TO. However, when we correlated these coefficients with each other by running a multivariate analysis to eliminate possible confounding factors, we saw that sex and age were, in fact, finally not independent factors for the achievement of TO, but rather these factors were: ASA < III (OR 2.39 95% CI 1.37–4.16); elective surgery (OR 2.77 95% CI 1.64–4.67); laparoscopic approach (OR 5.71, 95% CI 2.89–11.30); and “non-difficult” cholecystectomy (OR 0.42, 95% CI 0.259–0.71).
Logistic regression analysis for the achievement of TO after global cholecystectomy.
| Logistic regression textbook outcome | ||||||
|---|---|---|---|---|---|---|
| Univariate analysis | Multivariate analysis | |||||
| Variable | OR | CI 95% | P-value | Adjusted OR | CI 95% | P-value |
| SexMaleFemale | Ref1.594 | 1.065–2.385 | 0.023 | 1.221 | 0.763–1.953 | 0.406 |
| Age (Nº.) | 0.968 | 0.954–0.981 | 0.000 | 0.987 | 0.970–1.004 | 0.123 |
| ASAI–IIIII–IV–V | 3.123Ref | 2.011–4850 | 0.000 | 2.394 | 1.378–4.161 | 0.002 |
| Surgery TypeEmergencyElective | Ref3.094 | 2.027–4.722 | 0.000 | 2.772 | 1.645–4.673 | 0.000 |
| LaparoscopyNoYes | Ref6.713 | 3.812–11.823 | 0.000 | 5.717 | 2.892–11.303 | 0.000 |
| ERCPNoYes | Ref0.603 | 0.333–1.095 | 0.094 | |||
| Difficult CholecystectomyNoYes | Ref0.193 | 0.125–0.296 | 0.000 | 0.429 | 0.259–0.710 | 0.001 |
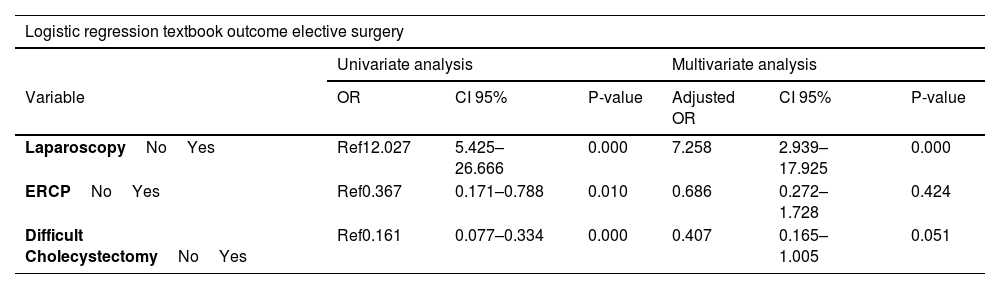
If we divide the sample according to scheduled and emergency surgery (Table 1), we see that the TO gives us percentages of 82.6% and 60.5% respectively. After applying multivariate analysis (Table 3), in elective surgery the laparoscopic approach and “non-difficult” cholecystectomy were independent factors for achieving this TO. In the case of emergency surgery, ASA < III, laparoscopic approach and “not difficult” cholecystectomy were statistically significant.
Logistic regression analysis for achievement of TO after scheduled and emergency cholecystectomy.
| Logistic regression textbook outcome elective surgery | ||||||
|---|---|---|---|---|---|---|
| Univariate analysis | Multivariate analysis | |||||
| Variable | OR | CI 95% | P-value | Adjusted OR | CI 95% | P-value |
| LaparoscopyNoYes | Ref12.027 | 5.425–26.666 | 0.000 | 7.258 | 2.939–17.925 | 0.000 |
| ERCPNoYes | Ref0.367 | 0.171–0.788 | 0.010 | 0.686 | 0.272–1.728 | 0.424 |
| Difficult CholecystectomyNoYes | Ref0.161 | 0.077–0.334 | 0.000 | 0.407 | 0.165–1.005 | 0.051 |
| Logistic regression textbook outcome emergency surgery | ||||||
|---|---|---|---|---|---|---|
| Univariate analysis | Multivariate analysis | |||||
| Variable | OR | CI 95% | P-value | Adjusted OR | CI 95% | P-value |
| SexManWoman | Ref1.926 | 1.122–3.307 | 0.017 | 1.815 | 0.984–3.348 | 0.057 |
| Age (No.) | 0.967 | 0.950–0.985 | 0.000 | 0.991 | 0.970–1.013 | 0.437 |
| ASAI–IIIII–IV–V | 5.162Ref | 2.751–9.687 | 0.000 | 3.442 | 1.641–7.220 | 0.001 |
| LaparoscopyNoYes | Ref5.696 | 2.307–14.061 | 0.000 | 3.519 | 1.290–9.603 | 0.014 |
| Difficult cholecystectomyNoYes | Ref0.306 | 0.175–0.534 | 0.000 | 0.459 | 0.246–0.856 | 0.014 |
The “textbook outcome” is being used increasingly as a tool to measure the quality of care of surgical procedures. To date, this is being used mainly in oncological surgeries with high morbidity and mortality.8 However, it is an indicator that brings together the main results measured after surgery (major complications, postoperative stay, readmissions and mortality), and is therefore easily extrapolated to other procedures with lower morbidity and mortality, such as cholecystectomy, and can be an easy marker for the general population to understand. This new marker of quality of care would not only serve patients as a basis for the choice of hospital for their pathology, representing the chances of the best possible result, but also the doctors and researchers themselves, gathering information on the frequency in which their surgical treatments and techniques were successful. This opens up the possibility of promoting improvements; for hospital management, since they could adopt TO to apply selective hiring; and for health inspectors, as this principle could guide medical surveillance programmes.
Regarding what has been described in the current literature on TOs in cholecystectomy, we see agreement regarding certain factors that are unfavourable when classifying TO, such as age, as described in the article by Iseda et al.,9 in which case this would be >70 years, 7 years older than in our results; and also the ASA classification, as in the article by Lucocq et al.,10 where the higher the ASA classification, the lower the achievement of a TO result, comparing this with our study where ASA ≥ III cases were the ones that achieved least TOs. In this last article, the indication of cholecystectomy for acute cholecystitis was also described as an unfavourable factor, which was consistent with our results. However, the performance of a previous ERCP also appeared to have an influence, in contrast to our analysis.
In another article by the same author,11 where morbidity after emergency vs. elective cholecystectomy was analysed, it was shown that emergency laparoscopic cholecystectomy was positively correlated with the appearance of adverse outcomes when compared to elective laparoscopic cholecystectomy, a fact that agrees with our series where scheduled surgery achieved a higher percentage of TO.
Regarding sex, there are no articles that relate cause, however, in our series female sex, in a first univariate analysis, was favourable for achievement of a TO. On another point, the approach chosen was studied, in our research, as a factor to be analysed, although in the two articles mentioned,9,10 the approach was a criterion of the definition of TO itself, where this necessarily had to be a “laparoscopic cholecystectomy without converting to open surgery” in order to be classified as a TO. In our study, after analysing this variable, we saw that the laparoscopic route was indeed more likely to achieve a TO.
Finally, in recent years many surgical groups have tried to define what is considered to be a difficult cholecystectomy. Two of the most recent examples are: the Delphi project carried out in 202112 by Spanish experts, where an attempt was made to reach a consensus on which perioperative factors were considered difficult in this procedure; and the “Nassar scale”13 as a preoperative scale to predict a difficult cholecystectomy. Nevertheless, we found a lack of consensus and studies in the current literature that individually related each possible predictor of difficulty with postoperative outcomes. We believe, however, that this is a parameter to be included in any study on cholecystectomy outcomes.
As limitations of the study, as this was a retrospective study, the collection of certain parameters such as complications, specifically minor complications, is sensitive to bias and difficult to record correctly if these parameters are not collected prospectively. In our case, these were systematically recorded in the hospital discharge report. In contrast, our variable “difficult cholecystectomy”, although this could be a subjective variable and dependent upon the surgeon, the exhaustive review of operating room reports in order to classify the procedure as difficult, was undertaken by one single person to avoid any type of bias.
ConclusionsIn conclusion, in our series, the percentage of textbook outcomes (TOs) for cholecystectomy was 72% (82.6% in elective surgery and 60.5% in emergency surgery). The factors that led us to achieve this, in line with the statistical analysis carried out were: female sex, age under 63 years, ASA < III risk, elective surgery and laparoscopic approach, in addition to cholecystectomy in which no intraoperative findings related to a difficult surgical procedure were detected, according to our classification. We believe that TO is a tool for quality care that is easy to perform, easily interpretable and useful for evaluating the quality of health care, as well as comparison of centres, applicable not only in oncological procedures but also in cholecystectomy.
Conflict of interestThis research has not received any specific support from public sector agencies, commercial or non-profit organisations. The authors have no conflict of interest.