Hepatic encephalopathy (HE) is a neuropsychiatric syndrome characterized by changes in cognitive function, behavior, and personality, as well as by transient neurological symptoms and electroencephalographic changes, which occur in the context of acute or chronic liver failure. Cirrhosis is the main disease associated to HE, and it is known that its incidence is increasing worldwide. As a cause of mortality, cirrhosis is ranked 14 worldwide, but 10 in developed countries. It has been demonstrated that the incidence of liver disease is increasing, in part because of the ascending prevalence of NAFLD, HCV, HCC, as well of alcohol consumption. The real incidence of cirrhosis in Latin America is unknown, although in some Latin American countries that provided national data, cirrhosis death rates were between 5 and 17/100,000 for men and 3 and 5/100,000 for women. Disability, quality of life, and social aspects should be considered when assessing the impact of a disease. In this context, preliminary estimates of the global burden of disease attributable to chronic liver disease seem to be substantial. Hepatic encephalopathy, a main complication of liver failure, occurs in 30-45% of patients as overt encephalopathy, but when subclinical or minimal hepatic encephalopathy (MHE) is considered, estimates of the incidence of encephalopathy vary from 20 to 60%. In USA, the 2009 NIH Report on the Costs of Digestive Diseases stated that liver disease was the second most costly disease in direct and indirect costs (13.1 billion dollars). Although the economic cost of HE has not been assessed, it is obvious that the economic impact of HE on daily activities of living is extremely high, as the costs of diminished work performance and lost wages are substantial.
Hepatic encephalopathy (HE) is a neuropsychiatric syndrome characterized by changes in cognitive function, behavior, and personality, as well as by transient neurological symptoms and characteristic electroencephalographic patterns, which occur in the context of acute or chronic liver failure.1 The most common clinical pattern is a progressive decline in the level of consciousness, which presents clinically as confusion, inability to perform simple activities, delirium, and even coma.2 Frequently, a precipitating factor can be identified (e.g., constipation, gastrointestinal bleeding, electrolytic disturbances, infections), and treatment of HE includes correction of the precipitating factor.3
Once the precipitating condition is resolved, the encephalopathy usually disappears, and the patient recovers his or her previous state. However, in patients with severe liver dysfunction, this entity may be chronic, burdening the patient with a severe disability.
Chronic encephalopathy has three clinical patterns:1,4
- •
Chronic recurrent encephalopathy: frequent episodes of acute encephalopathy.
- •
Chronic persistent encephalopathy: persistent neurological manifestations. These patients sometimes present with mild Parkinsonism, characterized by bradykinesia, ataxia, and dysarthria. On other occasions and in association with damage to the basal ganglia, extrapyramidal signs develop.
- •
Subclinical or minimal encephalopathy: this entity is of high importance, as it is associated with deterioration in work activities and other activities such as driving. Other changes are constructional apraxia, reduced visuospatial capacity, and a delayed choice reaction. It is usually not detected unless psychometric tests are conducted.
There is evidence demonstrating that the incidence of cirrhosis is increasing; this increase is associated with increasing alcohol consumption, a high incidence of non alcoholic teatohepatitis (NASH), and a high prevalence of hepatitis B and hepatitis C infections.5,6 Consequently, it is expected that more cases of decompensated cirrhosis will be diagnosed in the near future, including cases of HE.
Chronic Liver Disease in Latin AmericaSeveral researchers have demonstrated that liver disease will affect a large proportion of the population of Latin America in the future because of the high prevalence of alcohol consumption and the increasing prevalence of overweight, obesity, and diabetes5,6 (Figure 1).
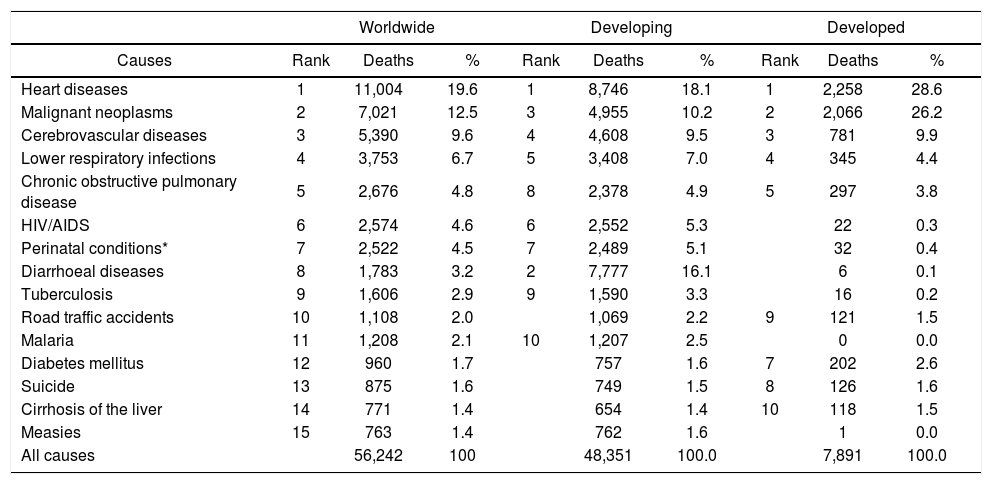
The incidence of liver disease is increasing worldwide. As a cause of mortality, cirrhosis is ranked 14 worldwide, but 10 in developed countries7 (Table 1). In the USA, the incidence of liver disease appears to be increasing, in part because of the increasing prevalence of NAFLD, HCV, and HCC.8,9 In 1998, chronic liver disease and cirrhosis were the 10th most frequent causes of mortality in the USA, accounting for 1.1% of all deaths.10,11
Leading causes of death worldwide and in developing and developed countries (2001) (Thousands).
| Worldwide | Developing | Developed | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Causes | Rank | Deaths | % | Rank | Deaths | % | Rank | Deaths | % |
| Heart diseases | 1 | 11,004 | 19.6 | 1 | 8,746 | 18.1 | 1 | 2,258 | 28.6 |
| Malignant neoplasms | 2 | 7,021 | 12.5 | 3 | 4,955 | 10.2 | 2 | 2,066 | 26.2 |
| Cerebrovascular diseases | 3 | 5,390 | 9.6 | 4 | 4,608 | 9.5 | 3 | 781 | 9.9 |
| Lower respiratory infections | 4 | 3,753 | 6.7 | 5 | 3,408 | 7.0 | 4 | 345 | 4.4 |
| Chronic obstructive pulmonary disease | 5 | 2,676 | 4.8 | 8 | 2,378 | 4.9 | 5 | 297 | 3.8 |
| HIV/AIDS | 6 | 2,574 | 4.6 | 6 | 2,552 | 5.3 | 22 | 0.3 | |
| Perinatal conditions* | 7 | 2,522 | 4.5 | 7 | 2,489 | 5.1 | 32 | 0.4 | |
| Diarrhoeal diseases | 8 | 1,783 | 3.2 | 2 | 7,777 | 16.1 | 6 | 0.1 | |
| Tuberculosis | 9 | 1,606 | 2.9 | 9 | 1,590 | 3.3 | 16 | 0.2 | |
| Road traffic accidents | 10 | 1,108 | 2.0 | 1,069 | 2.2 | 9 | 121 | 1.5 | |
| Malaria | 11 | 1,208 | 2.1 | 10 | 1,207 | 2.5 | 0 | 0.0 | |
| Diabetes mellitus | 12 | 960 | 1.7 | 757 | 1.6 | 7 | 202 | 2.6 | |
| Suicide | 13 | 875 | 1.6 | 749 | 1.5 | 8 | 126 | 1.6 | |
| Cirrhosis of the liver | 14 | 771 | 1.4 | 654 | 1.4 | 10 | 118 | 1.5 | |
| Measies | 15 | 763 | 1.4 | 762 | 1.6 | 1 | 0.0 | ||
| All causes | 56,242 | 100 | 48,351 | 100.0 | 7,891 | 100.0 | |||
Source: Lopez AD, Mathers CO, Ezzati M, et al. Global and regional burden of disease and risk factors, 2001: Systematic analysis of population health data. Lancet 2006; 367(9524): 1747-57.
Alcohol was responsible for at least 10% of disability-adjusted life years (DALYs) in the Americas in 2002, which is much higher than the global impact of alcohol on DALYs (4.4%) (Expert Committee in Alcohol. WHO Report N° 944, 2006). In addition, an epidemiological analysis by the World Health Organization identified alcohol as the main risk factor for morbidity in the Americas, but ranked it fourth on a global scale5 (Figure 2).
Viral hepatitis is a great problem globally. Estimated numbers of HBV- and HCV-infected subjects worldwide are staggering (370 million and 130 million, respectively).12 In South America, the hepatitis virus is endemic to the Amazon region.13 However, national hepatitis B vaccination programs will probably decrease its prevalence in the future. Chronic hepatitis C is a major problem worldwide. In Latin America, its prevalence varies between countries, ranging from 0.5 to 3%, but it is higher than 3% in certain areas of Brazil and Mexico.14,15
The incidence of cirrhosis in Latin America is unknown. Chile and Mexico had exceedingly high rates (about 60/100,000 men and 15/100,000 women) in the late 1980s; in other Latin American countries that provided national data, cirrhosis death rates were between 5 and 17/100,000 for men and 3 and 5/100,000 for women over the same period.16
In the period 2000-2002, Mexico and Argentina had the highest rates of mortality from cirrhosis in men, with 56.52 and 13.9 per 100,000, respectively.17 When age is taken into consideration, the prevalence of mortality associated with cirrhosis in men aged 35-64 years is even higher, at 117.41 and 27.94 per 100,000 in Mexico and Argentina, respectively. All the countries evaluated in that report showed a subtle decrease in the frequency of this entity during the period analyzed, except in Cuba, where it is increasing.17 Mendez, et al., recently demonstrated that the incidence of cirrhosis in Mexico has been increasing steadily since 2002.18
Disability, quality of life, and social aspects should be considered when assessing the impact of a disease. In this context, preliminary estimates of the global burden of disease attributable to chronic liver disease seem to be substantial, and this is associated with the complications of cirrhosis.19,20
Burden of Hepatic Encephalopathy in Latin AmericaThe principal complications of cirrhosis are variceal bleeding, ascites, and encephalopathy. The latter occurs in 30-45% of patients as overt encephalopathy, but when subclinical or minimal hepatic encephalopathy (MHE) is considered, estimates of the incidence of encephalopathy vary from 20 to 60%. Differences in the estimated prevalence of encephalopathy are caused by differences in the type and number of tests used (psychometric or electrophysiological), as well as by differences between test populations (etiology, severity of liver disease, and comorbidities).21-27
Although the total direct and indirect costs of HE have not been formally quantified, the 2009 NIH Report on the Costs of Digestive Diseases (USA) stated that liver disease was the second most costly disease in direct and indirect costs (13.1 billion dollars). This suggests that liver disease and its complications, including HE-related hospitalization and ambulatory management, are associated with substantial costs19,21-23 (Table 2).
Liver disease in the USA: number and age-adjusted rates of ambulatory care visits and hospital discharges as first-listed and all-listed diagnoses according to age.
| Ambulatory care visits | Hospital discharges | |||||||
|---|---|---|---|---|---|---|---|---|
| First-Listed Diagnosis | All-Listed Diagnosis | First-Listed Diagnosis | All-Listed Diagnosis | |||||
| Number in thousands | Rate per 100,000 | Number in thousands | Rate per 100,000 | Number in thousands | Rate per 100,000 | Number in thousands | Rate per 100,000 | |
| Under 15 | - | - | - | - | 2 | 2 | 9 | 14 |
| 15-44 | 346 | 275 | 490 | 389 | 35 | 28 | 153 | 122 |
| 45-64 | 665 | 941 | 1,374 | 1,944 | 102 | 144 | 365 | 517 |
| 65+ | 358 | 996 | 503 | 1,385 | 47 | 129 | 233 | 640 |
Adapted from Everhart JE. Liver Disease. In: The burden of digestive diseases in the United States. Chapter 21. US Department of Health and Human Services, Public Health Service, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases. Washington, DC: US Government Printing Office, 2008; NIH Publication No. 09-6443.
In recent years, MHE has attracted much attention in relation to its effects on motor activities, mainly driving and daily work activities. It is also important because it may be a predictor of overt encephalopathy. In addition, MHE is associated with a high Child-Pugh score, portal hypertension, and an adverse prognosis.27-31
Although the economic cost of HE has not been assessed, it is obvious that the economic impact of HE on daily activities of living is extremely high, as the costs of diminished work performance and lost wages are substantial.32
ConclusionsThere are no data on HE in Latin America. Data on the prevalence and incidence of cirrhosis are not accurate, but the high prevalence of overweight, diabetes, and alcoholism suggests that liver disease and its complications will increase in the future.
Considering these facts, the study and diagnosis of HE are of great importance for practicing gastroenterologists and hepatologists. It is important to expand research in this field and to develop better therapeutic strategies to improve the quality of life and survival of HE patients and to decrease the cost of treating HE.