Both acute and chronic liver disease can manifest on the skin. The appearances can range from the very subtle, such as early finger clubbing, to the more obvious such as jaundice. Identifying these changes early on can lead to prompt diagnosis and management of the underlying condition. In this pictorial review we will describe the skin manifestations of specific liver conditions illustrated with appropriate figures.
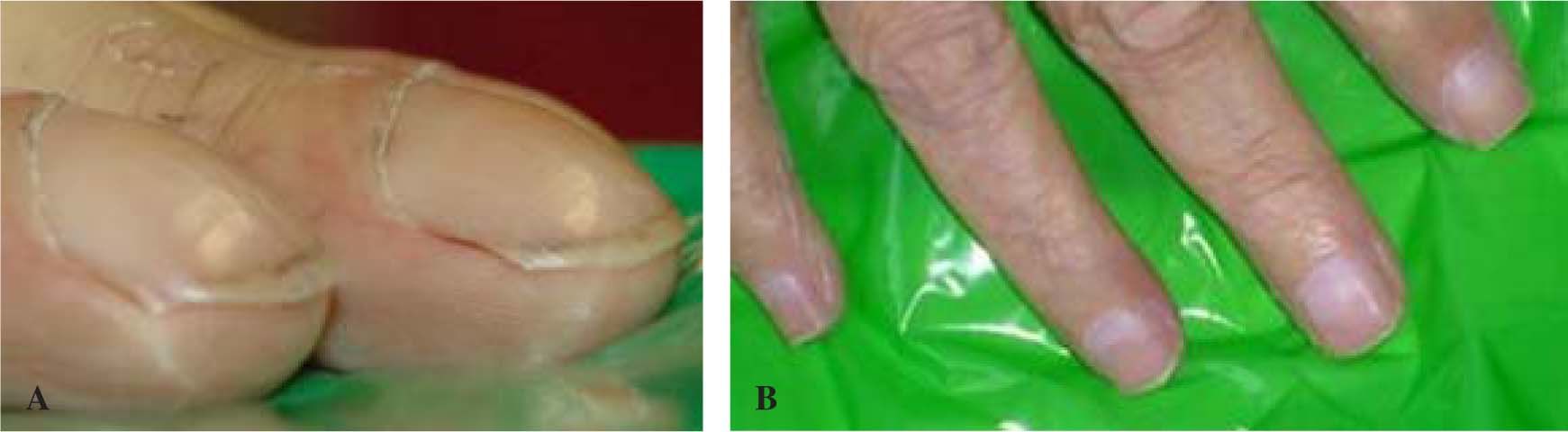
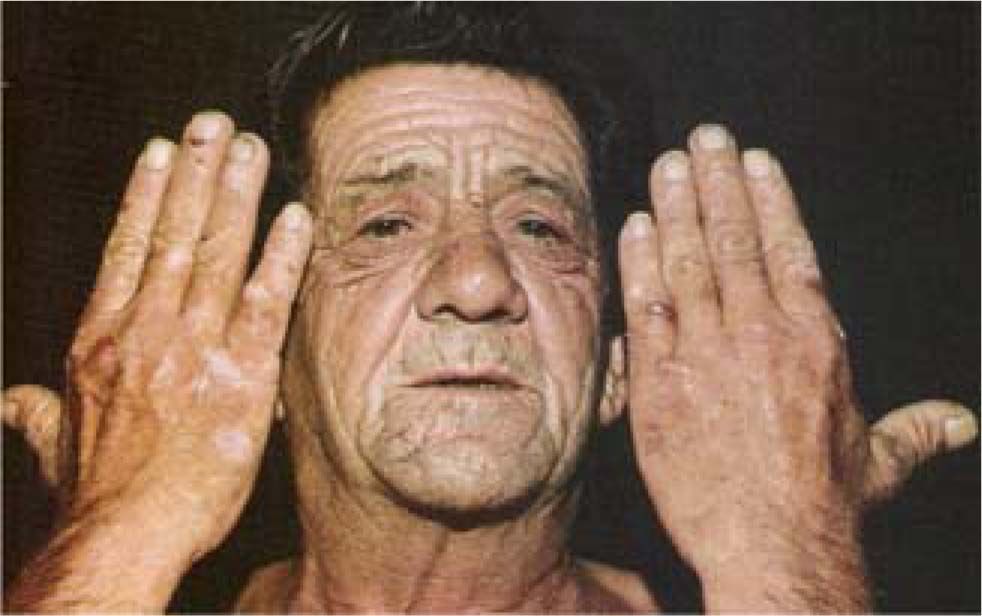
General skin findings in liver diseaseChronic liver disease of any origin can cause typical skin findings. Jaundice, spider nevi, leuconychia and finger clubbing are well known features (Figures 1 a, b and Figure 2). Palmar erythema, “paper-money” skin (Figure 3), rosacea and rhinophyma are common but often overlooked by the busy practitioner. More subtle signs include scratch marks, loss of axillary hair and gynaecomastia. Ascites can lead to striae (Figure 4) and an umbilical hernia (Figure 5).
Gross clubbing in patient with alcohol-related liver cirrhosis (Koulaouzidis A, Said E. Clubbing in a patient with liver disease. Saudi Med J 2007 Mar; 28: 481-2, with permission). B. (ammendum) - Terry’s nails or half-and-half nails/associated with hypoalbuminaemia in patient with cirrhosis.
Xanthelasmas are collections of lipid-laden histiocytes deposited in the upper and lower eyelids (Figure 6). They can be florid and are usually idiopathic. There is a firm connection between PBC and hypercholesterolemia, which can explain the tendency of these patients to develop both xanthelasmas and cutaneous xanthomas (5%) (Figure 7).1 Other disease-associated skin manifestations, but not as frequent, include the sicca syndrome and vitiligo.2 Melanosis and xerodermia have been reported. PBC may also rarely present with a cutaneous vasculitis (Figure 8 and Figure 9).3-5
Dupuytren’s contracture was described initially by the French surgeon Guillaume Dupuytren in the 1830s. Although it has other causes, it is considered a strong clinical pointer of alcohol misuse and its related liver damage (Figure 10).6 Therapy options other than surgery include simvastatin, radiation, N-acetyl-L-cysteine.7,8 Facial lipodystrophy is commonly seen as alcohol replaces most of the caloric intake in advanced alcoholism (Figure 11).
Porphyria cutanea tarda (PCT) is the commonest of the porphyrias and results from deficiency of the enzyme uroporphyrinogen decarboxylase (UROD).9 The terms porphyrin and porphyria are derived from the Greek word “noρϕνρóς” which means purple. The blistering rash develops in sun-exposed areas and increased local hair growth eventually appears (Figure 12). Alcohol remains the best known trigger factor -especially in patients with concurrent HCV infection-and complete abstinence is advisable.
Viral hepatitisHCV association with extrahepatic manifestations can occur in one third of patients with chronic infection and is generally seen in the late stages of the disease.10 Cryoglobulinemia, polyartiritis nodosa (Figure 8), leucocytoclastic vasculitis (Figure 13), urticaria and porphyria cutanea tarda (Figure 12) are the classic skin manifestations of chronic HCV and less frequently HBV infection.11,12
HemochromatosisIron is deposited in multiple organs including the skin. ‘Slate grey’ skin is often used to describe the typical skin manifestation of hemochromatosis. The term “bronze diabetes” was also used to describe the classic presentation. With the advent of blood testing for the diagnosis of hemochromatosis the term has become obsolete. Multiple organ involvement is seen less commonly now that genetic screening of relatives is commonplace. Treatment with venesection in the presymptomatic stage of the disorder is advocated.
ConclusionThe skin is the largest organ in the body and if examined too briefly this will lead to subtle changes that can be missed. In the modern era, where laboratory and radiological investigations are close at hand, the art of clinical medicine is practiced less often. Identifying these fascinating clinical signs not only aids in making a diagnosis but provides satisfaction to the clerking physician.