We report a case of rhombencephalitis infection by Listeria monocytogenes in a 66-year-old man with cirrhosis. The CSF analysis indicated L. monocytogenes as the most likely pathogen. Blood and CSF culture were positive to L. monocytogenes and MRI findings were suggestive of rhomboencephalitis. The treatment was started empirically and then modified when the culture results were available. The patient had a full clinical recovery without neurologic sequelae. Clinicians should remember that L. monocytogenes most often presents as acute bacterial meningitis, particularly in the elderly, the immunosuppressed, and those with malignancies. L. monocytogenes CNS the infections may present as acute bacterial meningitis, meningoencephalitis, or acute encephalitis.
Listeria monocytogenes, an aerobic, Gram-positive, food-borne pathogenic bacterium displays “tumbling motility” on wet-drop preparations and produces hemolytic colonies on blood Agar. It is a major bacterial cause of neuroinvasive infection. Listeria mostly infects elderly, Immunosuppressed individuals, pregnant women, fetuses and neonates. It is characterized by a high mortality rate, with clinical features including most frequently acute bacterial meningitis, less commonly as meningo-encephalitis and least commonly as acute encephalitis, septicemia, and in some cases gastroenteritis, abortion, and perinatal infections.1–3
Neurolisteriosis, present as isolated meningitis, encephalitis or rhombencephalitis, is observed in elderly people or in patients with either primary or secondary immunodeficiency following antineoplastic chemotherapy, immunosuppressive treatment prescribed for bone marrow, stem cell, or organ transplantation, or in the context of chronic debilitating diseases (diabetes and cirrhosis).4,5
We present a case of rhombencephalitis due to Listeria monocytogenes in a cirrhotic patient, whose diagnosis was based on clinical findings, blood culture, CSF and magnetic resonance. The differential diagnostic aspects are discussed, including the importance of Neurolisteriosis in cirrhotic patients.
Case ReportA 66-year-old man was brought to the emergency room with sudden deterioration of his mental status and the antecedent of intermittent fevers and low intensity headache in the previous month. He had no history of focal sensory or motor impairments. The patient’s medical history included type 2 diabetes mellitus, arterial hypertension and cryptogenic cirrhosis. The family reported the antecedent of consumption of unpasteurized products.
During the physical examination, the patient appeared in distress. Head and neck examination were significant for nuchal rigidity. Cardiopulmonary examination was unremarkable. Bowel sounds were normal. Abdominal tenderness and ascites were present. Neurologic examination showed a state of stupor (Glasgow coma scale of 11/15) with no focal neurological defects. The patient developed a serious neurological deterioration, dropping to a Glasgow coma scale of 8/15, a major reason to continue the treatment on the Critical Care Unit with invasive airway management.
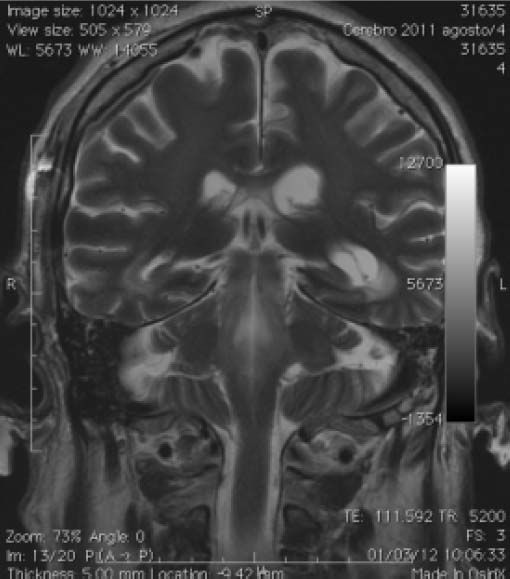
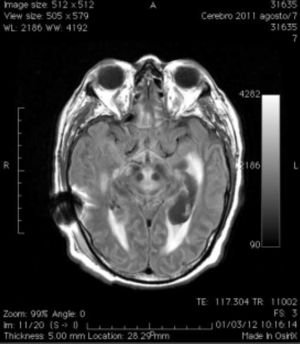
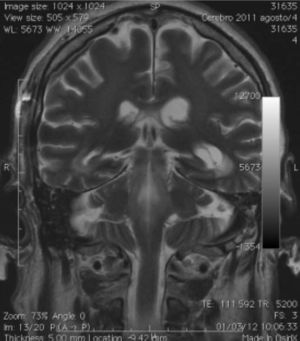
A magnetic resonance imaging of the head, revealed both, lateral and third ventricles dilated and transependymal migration of spinal fluid (Figure 1). Post-contrast T1-weighted magnetic resonance imaging of the cranium revealed an enlarged area in the spinal medulla, cerebellar peduncle and cerebral fissures. It also showed hypertensive hydrocephalus, requiring surgical management (Figure 2).
A lumbar puncture was performed, the cerebrospinal fluid (CSF) appeared xanthochromic. The white blood cell count 2,600 mm3, RBC count 1,000 mm3, crenocytes 0, 32 mg, total protein 148 mg/dL, glucose 48 mg/dL and negative Gram stain and KOH.
Pharmacological treatment was started empirical ly with ceftriaxone 2 g IV every 12 h and ampicillin 2 g IV every 4 h. Listeria monocytogenes was isolated from blood and CSF cultures; ceftriaxone was then discontinued. Ampicillin was continued for a total of 4 weeks of therapy. After 9 days in the hospital the patient woke up, and during the tenth day the patient was fully alert and oriented with no residual neurologic dysfunction. Full recovery was achieved after 1 month. Magnetic resonance imaging scans performed on days 30 and 60 documented the resolution of abnormalities.
DiscussionListeria monocytogenes has been linked to sporadic episodes as well as severe outbreaks of infections worldwide.6–9 The vast majority of human listeriosis cases occur following consumption of contaminated food.10 Although relatively rare (the annual incidence rate ranges from 1 to 10 cases per million), listeriosis has an important impact on public health given that it is responsible for the highest hospitalization and mortality rates amongst food-borne.11 In listeriosis the fatality rate ranges from 24 to 52% despite adequate antimicrobial treatment.12
Listeria monocytogenes neuroinfection generally develops as meningitis/meningoencephalitis, usually associated with bacteremia. Meningitis prevails in newborns, seniors and patients with immunosuppressive disorders or other concurrent conditions.13 Less common central nervous system manifestations include abscesses in the cerebrum or cerebellum; in addition in up to 24% of the patients encephalitis targets the brainstem (Rhombencephalitis).14–16 Rhombencephalitis was first described in 1957 by Eck as an unusual form of listeriosis.17 In contrast to meningitis; it appears to occur predominantly in previously healthy patients without any predisposing conditions.18 The condition is fatal if not treated during the early stages, and survivors commonly have significant neurological sequelae.
Listeria monocytogenes can cause meningitis, meningoencephalitis, or abscess formation in the central nervous system. Rhombencephalitis is a particular form of listerial encephalitis that affects primarily the brain stem and cerebellum (rhombencephalon). Listerial infection is often misdiagnosed because the prodromal symptoms are nonspecific and meningeal signs are uncommon. The CSF in listerial infection typically reveals an increased leukocyte count, usually with the predominance of polymorphonuclear cells, increased protein, and normal glucose levels. Due to the fact that L. monocytogenes is only sensitive to certain antibiotics it is important to establish an early microbiological diagnosis. L monocytogenes is difficult to isolate from the CSF but are often readily cultured from blood. In addition to the microbiological diagnosis, MR imaging is extremely important in demonstrating the predilection of the listerial infection for the brain stem and cerebellum.
One should always suspect listerial rhombencephalitis in the presence of an acute onset of progressive cranial nerve dysfunction and ataxia, CSF leukocytosis with polymorphonuclear cell predominance with normal glucose levels, and MR findings of brain stem (primarily pontomedullary) and cerebellar lesions. The early performance of MRI in the course of the disease would strongly support listerial rhombencephalitis in conjunction with the spinal fluid results which is essential in choosing the appropriate antibiotic treatment while awaiting culture confirmation. Early treatment can decrease the morbidity and mortality of this pathogen.
L. monocytogenes is a common cause of central nervous system (CNS) infections, especially in immunosuppressed patients, infants and seniors. Listerial rhombencephalitis is a rare and severe infection of the brainstem that is reported to have high mortality and frequent serious sequelae for survivors.19
However, in patients with cirrhosis one of the most common causes of the of Listeria monocytogenes infection is peritonitis. When searching for information related to rhomboencephalitis due to listeria in patients with cirrhosis it is shocking to find there are few publications related to this topic.20–25
Some recommendations could be made to improve the prognosis in patients with cirrhosis and bacterial meningitis. Meningitis should be suspected in every patient with cirrhosis who is in a febrile coma. If lumbar puncture has to be delayed because a computed tomographic scan of the head is to be done (papilledema or focal neurological deficit), or if no causative agent can be identified on CSF Gram stain, empirical antimicrobial therapy should be started straightaway because of the risks of delay.26 Given the wide variety of pathogens encountered in patients with cirrhosis, ampicillin plus a third-generation cephalosporin should be recommended, in sufficient doses.27
ConclusionsEncephalitis due to L. monocytogenes remains as an important public health issue, particularly in the elderly, infants, immunosuppressed, and those with malignancies. For patients with a clinical diagnosis of rhomboencephalitis and acute bacterial meningitis, recognition of the symptoms caused by listerial infection plays a vital role in allowing early diagnosis, treatment and ensures an optimal patient outcome without neurologic sequelae. An urgent MRI brain scan is indicated for patients with progressive disabling brainstem signs, being the imaging study of choice. Studies of CSF often only reveal mild abnormalities. Ampicillin with or without an aminoglycoside remains the best treatment for meningitis caused by L. monocytogenes. When treating patients allergic to penicil lin, the use of co-trimoxazole has demonstrated to be the best alternative therapy. Respiratory failure and continuous monitoring in an intensive care unit is required to prevent fatal respiratory arrest.