Liver abscess due to perforation of the gastrointestinal tract by a foreign body is a rare and possibly fatal event. Diagnosing this pathology is complicated by the lack of specific symptoms and unfamiliarity of ingestion by the patient and low clinical suspicion of this disease. In the case of liver abscess unresponsive to aspiration and administration of antibiotics, this hypothesis must be made, despite its low incidence. This case report describes and illustrates a case of liver abscess secondary to fish bone ingestion with consequent piercing of the lesser gastric curvature, diagnosed by computed tomography and specific anamnesis. Laparoscopy was performed to extract the foreign body, without complications; the patient is currently asymptomatic and does not present any abnormal physical examination findings. We believe this represents the first case report of a successful laparoscopic treatment in South America for the removal of an ingested foreign body associated with pyogenic liver abscess.
Intra-abdominal abscesses secondary to perforation of the gastrointestinal tract by foreign body ingestion are not uncommon in clinical practice. However, secondary hepatic abscesses to foreign body ingestion are rare: only sixty cases have been described in the literature to date.1–3 It is a potentially serious condition that is a major diagnostic and therapeutic challenge, presenting high risk and leading to death in some cases. The difficulty in recognizing this condition is due to the non-specificity and variability of possible symptoms, the difficulty of evidence of the foreign body through conventional imaging and the low clinical suspicion inherent to its rarity. This study presents a case of perforation of the lesser gastric curvature after fish bone ingestion, with involvement of the left lobe of the liver and consequent formation of pyogenic hepatic abscess.
Case PresentationA 44-year-old female patient, with no history of previous disease, was admitted to the emergency department of the Hospital de Clinicas de Porto Alegre presenting intense and uninterrupted epigastric pain for two weeks, associated with fever (38.5 to 39 °C) for six days. She had sought treatment in various hospitals in recent days and was discharged with symptomatic medications for pain relief. She denied nausea or vomiting and had no allergies to medications. She had laboratory tests from other hospitals, in which the only alteration presented was a white blood cell count with neutrophilic leukocytosis.
On physical examination, the patient was in good general condition, alert, lucid, anicteric, acyanotic, eupneic and febrile. Examination of the cardiovascular and respiratory systems did not show any abnormal findings. Her abdomen was soft, depressible, painful on epigastric palpation. There were no signs of peritoneal irritation and also no signs of liver failure or portal hypertension.
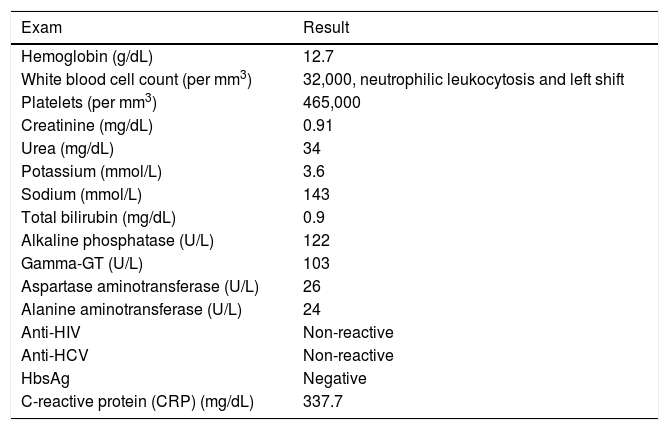
The plan included laboratory tests (Table 1), abdominal ultrasound, hepatitis B, hepatitis C and HIV serology, as well as prescription of symptomatic medication, hydration and empiric antibiotic therapy with piperacillin-tazobactam, aiming for adequate coverage of gram-negative pathogens and anaerobes.
Patient’s Laboratory Tests Results.
| Exam | Result |
|---|---|
| Hemoglobin (g/dL) | 12.7 |
| White blood cell count (per mm3) | 32,000, neutrophilic leukocytosis and left shift |
| Platelets (per mm3) | 465,000 |
| Creatinine (mg/dL) | 0.91 |
| Urea (mg/dL) | 34 |
| Potassium (mmol/L) | 3.6 |
| Sodium (mmol/L) | 143 |
| Total bilirubin (mg/dL) | 0.9 |
| Alkaline phosphatase (U/L) | 122 |
| Gamma-GT (U/L) | 103 |
| Aspartase aminotransferase (U/L) | 26 |
| Alanine aminotransferase (U/L) | 24 |
| Anti-HIV | Non-reactive |
| Anti-HCV | Non-reactive |
| HbsAg | Negative |
| C-reactive protein (CRP) (mg/dL) | 337.7 |
Abdominal ultrasound showed a probable liver abscess located in the left lobe, involving segment II. There was no bile ducts dilatation, and other organs had no evidence of abnormalities. To further elucidate the investigation, the emergency team requested an abdominal CT. Meanwhile, the patient remained clinically stable.
Abdominal CT at the second day showed the presence of a heterogeneous lesion with hypodense areas, located in segments II and III of the liver and measuring about 9.5 x 7.2 x 6.8 cm.
After surgical evaluation, the patient underwent percutaneous puncture of the abscess guided by ultrasound, draining 10 mL of purulent material, which was sent for culture. A drain was placed and left after the procedure. Bacterioscopic exam revealed many gram-positive cocci in clusters, as well as gram-positive and gram-negative bacilli. At this time, four days after her arrival, the patient was afebrile and reported substantial pain improvement. The emergency department decided to change the treatment to cefepime + metronidazole.
On the 7th day, bacteriological exam revealed isolation of Group C beta-hemolytic Streptococcus and Streptococcus sp (viridans group). Due to the possibility of infectious endocarditis and pyogenic liver abscess resulting from hematogenous seeding from the systemic circulation, and considering the absence of results of blood culture at that time, a transthoracic echocardiography was requested.
On the 8th day, transthoracic echocardiogram showed no structural alterations. A transesophageal echocardiography was not undertaken due to the low probability of an infectious endocarditis; moreover, test results showed negative blood cultures. Another abdominal CT was performed after seven days of treatment, which showed partial reduction of the abscess, measuring 7.5 x 7.0 x 6.1 cm at the time.
On the 12th day, the patient was transferred to the inpatient unit, where she was under the care of our team. After discussing about the case with the Infection Control Committee of the institution, antibiotic therapy was switched to intravenous amoxicillin-clavulanate. A consultation was requested to the gastroenterology team, in order to decide whether an investigation of hepatobiliary disease and malignancy (colorectal neoplasia) should be done; afterwards, a plan was traced including a magnetic resonance cholangiography and colonoscopy. Two days later, the patient remained clinically stable, having been afebrile for more than seven days. Blood tests showed decreasing C-Reactive Protein (34.1), tending to normal, as well as a normal white blood cell count and differential. The percutaneous drain was removed, without intercurrences.
On the 18th day, a new abdominal CT elucidated the etiology of the liver abscess: it showed a hyperdense linear structure, suggestive of a foreign body, perforating the lesser gastric curvature and reaching the left hepatic lobe, measuring about 2.5 cm (Figures 1 and 2). Following this finding, a new directed interview was then performed with the patient, who confirmed she had eaten “fish stew” about three weeks before the day she sought the Emergency Department of our hospital. She informed that it occurred on Good Friday, a fact that helped her recall the occurrence. She stated that abdominal pain began just after that meal. However, she thought it was due to food poisoning, not associating the fact directly to the current clinical situation and, therefore, did not mention this event before, despite the intensity of the pain.
Thus, our team cancelled the requests for magnetic resonance cholangiography and colonoscopy. A retrospective review of the first CT was then performed and the foreign body was barely visible, perhaps due to tomographic angle and thickness of the cuts. An upper gastrointestinal endoscopy was performed in order to remove the foreign body; however, it was not identified during the procedure, which prevented its extraction.
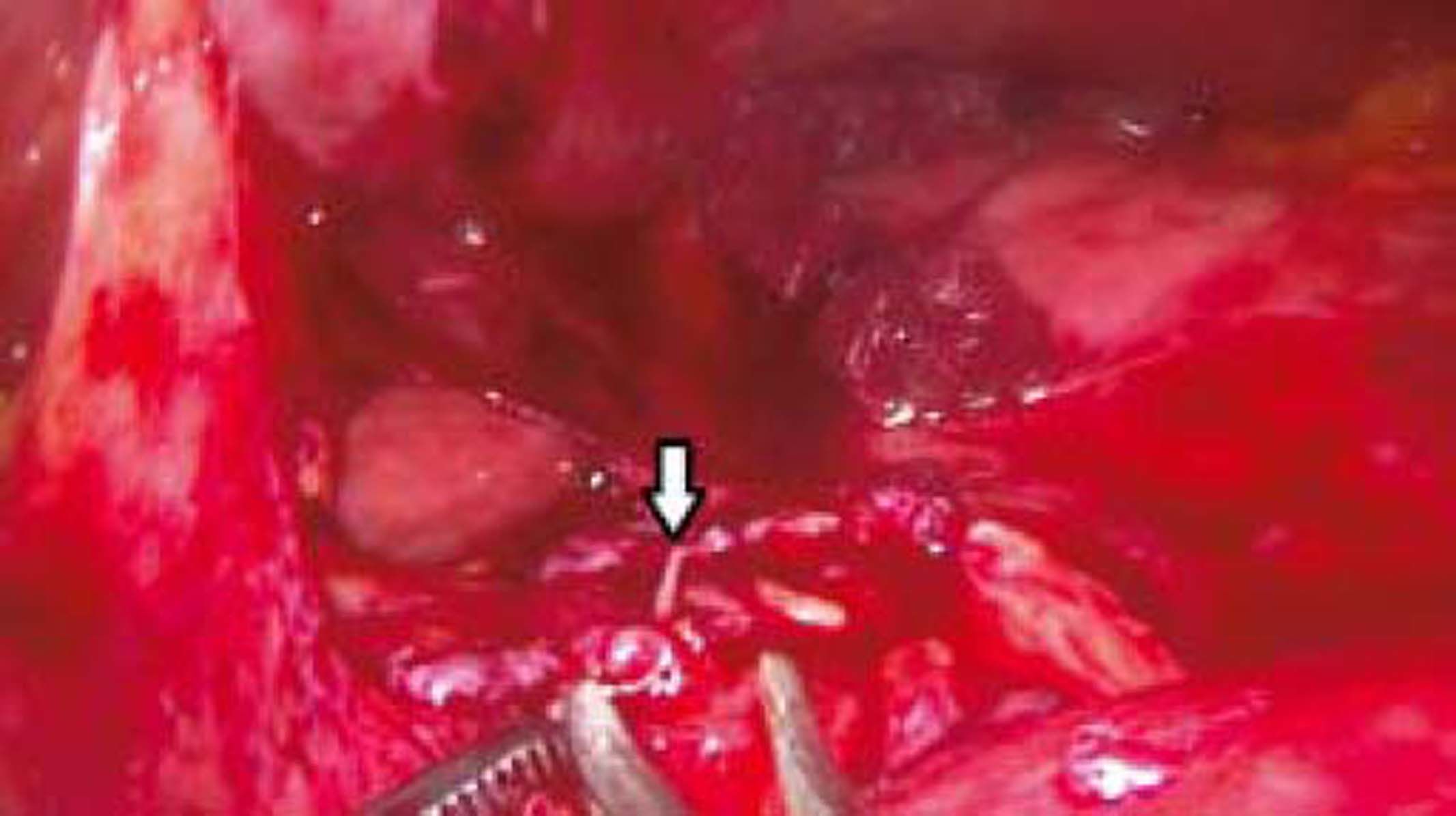
After literature review and discussions about the case, foreign body removal through surgery was planned, in order to avoid persistence and/or abscess recurrence. The patient was successfully subjected to laparoscopy for removal of the foreign body, with no intercurrences (Figures 3-5).
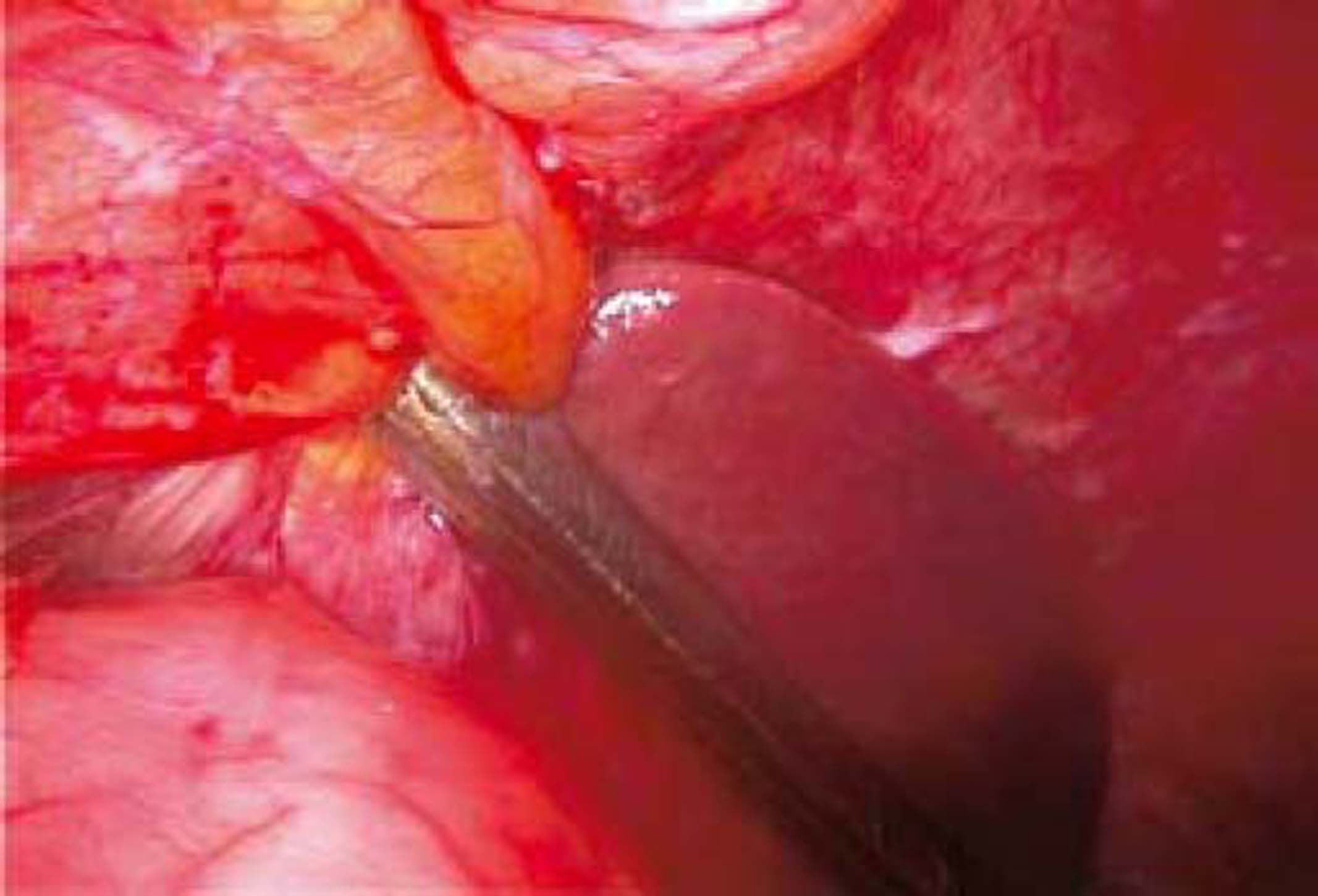
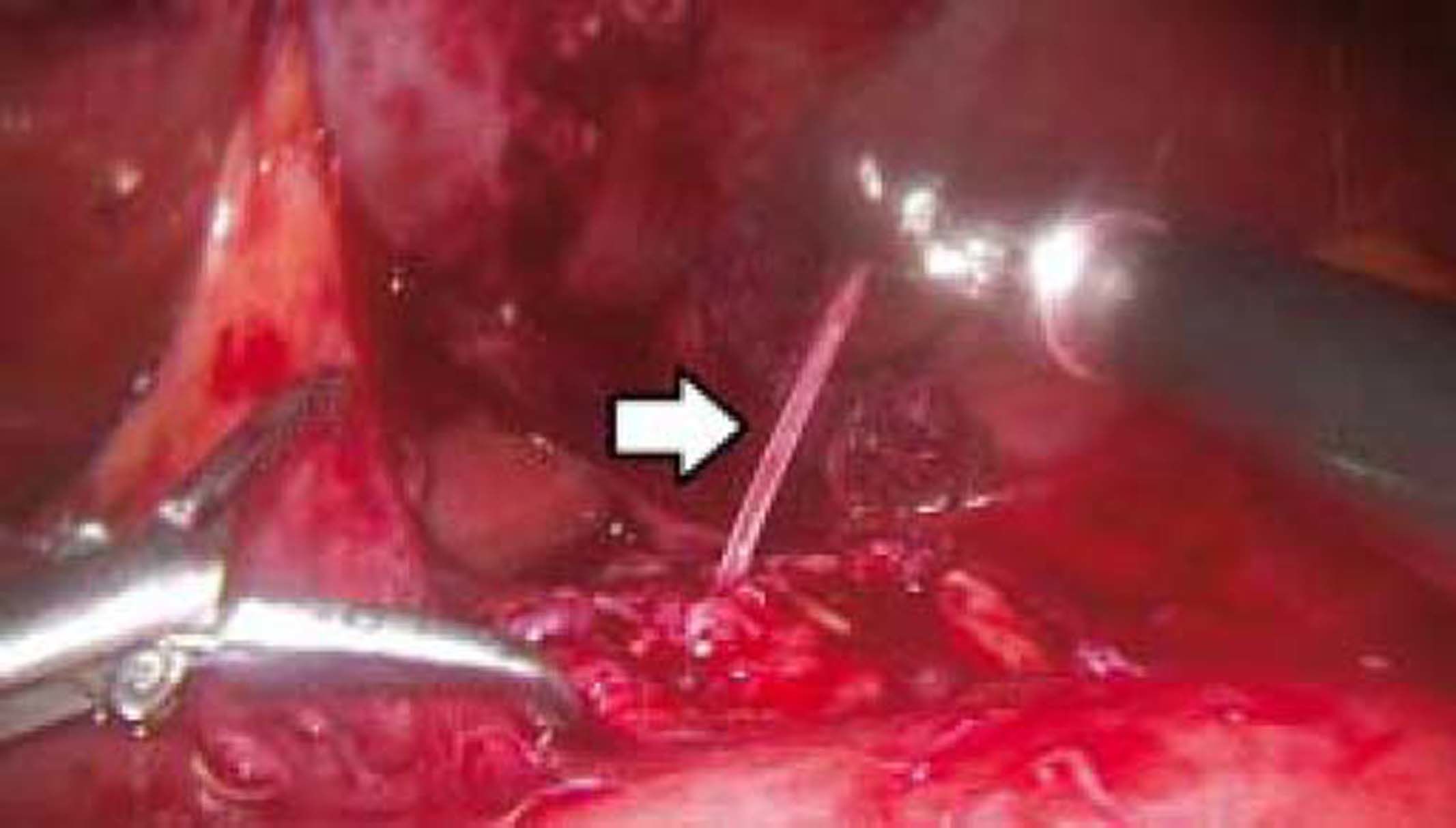
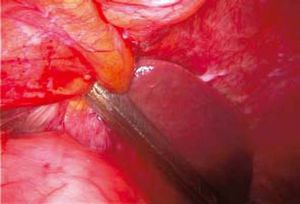
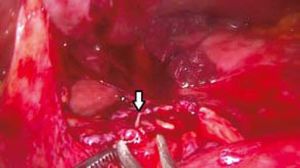
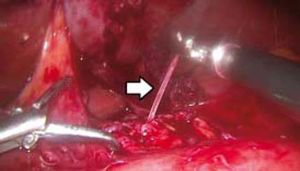
The surgical procedure involved left supraumbilical incision with laparoscopic pneumoperitoneum, puncture with a 10 mm trocar and introduction of a 30 mm optical. Afterwards, three 10 mm trocars were placed under direct vision. Multiple areas of adherence between the gastric antrum and the posterior part of the left hepatic lobe (segments III and IVB) were identified. Subsequently, dissection of the adhesions was performed, which revealed the presence of gross scar tissue at the level of the lesser gastric curvature. Debridement was then performed; the foreign body was found perforating the lesser gastric curvature. It was removed by traction, and interrupted X sutures were placed at the perforation site, together with protective omentopexy. At the end of the procedure, methylene blue solution was used to test for leaks, which did not occur. Finally, the cavity was washed and reviewed, portals were closed and bandages were done. It was confirmed that the foreign body was a fish bone, as expected (Figure 6).
The patient was discharged two days after surgery, in good general condition, afebrile and without abdominal pain, with prescription of oral amoxicillin-clavulanate for two weeks, in order to complete six weeks of antibiotic therapy.
She returned for review consultation 15 days after hospital discharge, asymptomatic and presenting no abnormalities in physical examination. The patient continues in outpatient follow-up, experiencing an uneventful outcome, without new signs or symptoms.
DiscussionMost ingested foreign bodies pass through the gastrointestinal tract uneventfully, generally within a week.3–6 The incidence of gastrointestinal perforation by ingestion of foreign bodies is low and is usually caused by sharp or pointed objects. It is estimated that the formation of liver abscess due to perforation by foreign body in the digestive tract is an even rarer complication: there are only a few cases reported in the literature. The first case was described in 1898; since then other 59 cases were published.1–3 Fish bones are usually the most frequently isolated causal agents, followed by toothpicks and by chicken bones.1,4,6–8
We presented a case of pyogenic liver abscess secondary to perforation of the gastrointestinal tract by a fish bone. In similar situations, the foreign body generally pierces the duodenum or the stomach, which determines left lobe predominance in migrated foreign body liver abscess.1 Typically, the patient has fever and abdominal pain, as occurred in this report. Jaundice occurs in a low percentage of the patients, and may be associated with an episode of cholangitis.5,8 Mortality from liver abscess is significant, although it has declined substantially in recent studies, ranging from 11% to 31%.8Streptococcus is the most frequently isolated germ; however, in about half the cases the etiologic agent is unknown.7,8 Treatment consists of surgery, abscess drainage and removal of the foreign body, recommended to prevent recurrence of this condition.1,4–8 Most patients have nonspecific symptoms. Foreign body liver migration can be silent for a long time, and it is usually discovered only when there is infection or abscess. Therefore, the diagnosis by clinical history is intricate: the level of suspicion is low both because of the frequent patient’s unawareness of the foreign body ingestion and the nonspecific symptoms, which may resemble various causes of abdominal pain, such as renal abscess, subphrenic abscess, acute cholecystitis, acute appendicitis, cholangitis, pleurisy, lung abscess and general serious infectious diseases.2 The diagnosis through conventional radiology is not common and performing an abdominal CT scan can be of great value.
In this report, the third abdominal CT showed the foreign body perforating the lesser gastric curvature, whose nature was confirmed in a new interview with the patient.
When an early diagnosis is established and after the surgical removal of the foreign body and abscess drainage, patients usually present good outcomes. A good prognosis is observed once the foreign body is removed and the liver abscess resolved. However, there are reports of fatal liver abscess after foreign body migration, due to sepsis in patients not previously diagnosed; sometimes, the object may only be revealed in autopsy.4 The case highlights the importance of early diagnosis due to the high level of severity of the etiology.
In the case presented in this report, laparoscopy was performed in order to remove the foreign body. According to available data, the rate of resolution without removal of the foreign body is 9.5%.1 On the other hand, once established the correct diagnosis and performed interventions, cure is achieved in virtually all cases: 46 of the 47 cases reported treated by surgery were successful, mostly by laparotomy, and only two by laparoscopy.1
Minimally invasive liver resection has been expanded over the past two decades. Although most major hepatectomies are still performed as an open surgical procedure, a laparoscopic approach is considered the gold standard treatment for lesions located on the left lateral segment of the liver (II and III).9 In addition to that, the operating field is magnified by laparoscopic view, which provides a better identification of small vessels and other structures. As a matter of fact, laparoscopic surgery was chosen in this case as a less invasive option for the fish bone retrieval.
Therefore, foreign body migration from the gastrointestinal tract to the liver is a rare cause of pyogenic liver abscess, but increasingly recognized as a cause of treatment failure and recurrence. Late diagnosis is a concern due to the high severity index, which highlights the need for consideration of this hypothesis. Early diagnosis is challenging due to the lack of specific symptoms, the patient’s unawareness about the ingestion and low suspicion of this condition by the healthcare team.
In refractory cases to aspiration and administration of antibiotics, foreign body migration must be considered as a potential cause of pyogenic liver abscess, despite its rarity. Conventional radiological exams do not usually provide useful information in these cases. Abdominal CT scans may be helpful, as well as a more comprehensive anamnesis, which should include question about recent fish or chicken meals and use of toothpicks. During abscess drainage surgeries, a thorough investigation should be adopted.
Successful treatments include surgery in virtually all cases previously reported. Laparotomy is the most commonly used technique. After extensive research, we believe this is the first case report of a successful treatment of a pyogenic liver abscess secondary to foreign body migration by laparoscopic surgery in South America.
Grant Support and Financial DisclosuresUniversidade Federal do Rio Grande do Sul; Associate Professor.
Conflict of InterestsAll the authors declare no conflict of interests.