Abstracts of the 2022 Annual Meeting of the ALEH
More infoPatients with nonalcoholic fatty liver disease (NAFLD) are at increased cardiovascular risk, and there is a higher prevalence of this disease in patients with coronary heart disease (CHD). However, the evidence in favor of NAFLD as a risk factor for CHD is scarce. This study aimed to determine the prevalence of NAFLD in patients with CHD and to assess whether significant CHD is associated with NAFLD and liver fibrosis.
Materials and MethodsObservational, analytical study in adult patients with coronary angiography for suspected coronary artery disease between July 2021-July 2022. The number of affected coronary vessels and the presence of significant CHD (stenosis >50%) were determined. In addition, FibroScan® was performed to evaluate steatosis and liver fibrosis up to 6 months after the coronary study, considering the presence of fibrosis at F>0. Descriptive statistics, Fisher's exact test and logistic regression models were reported for inferential analysis.
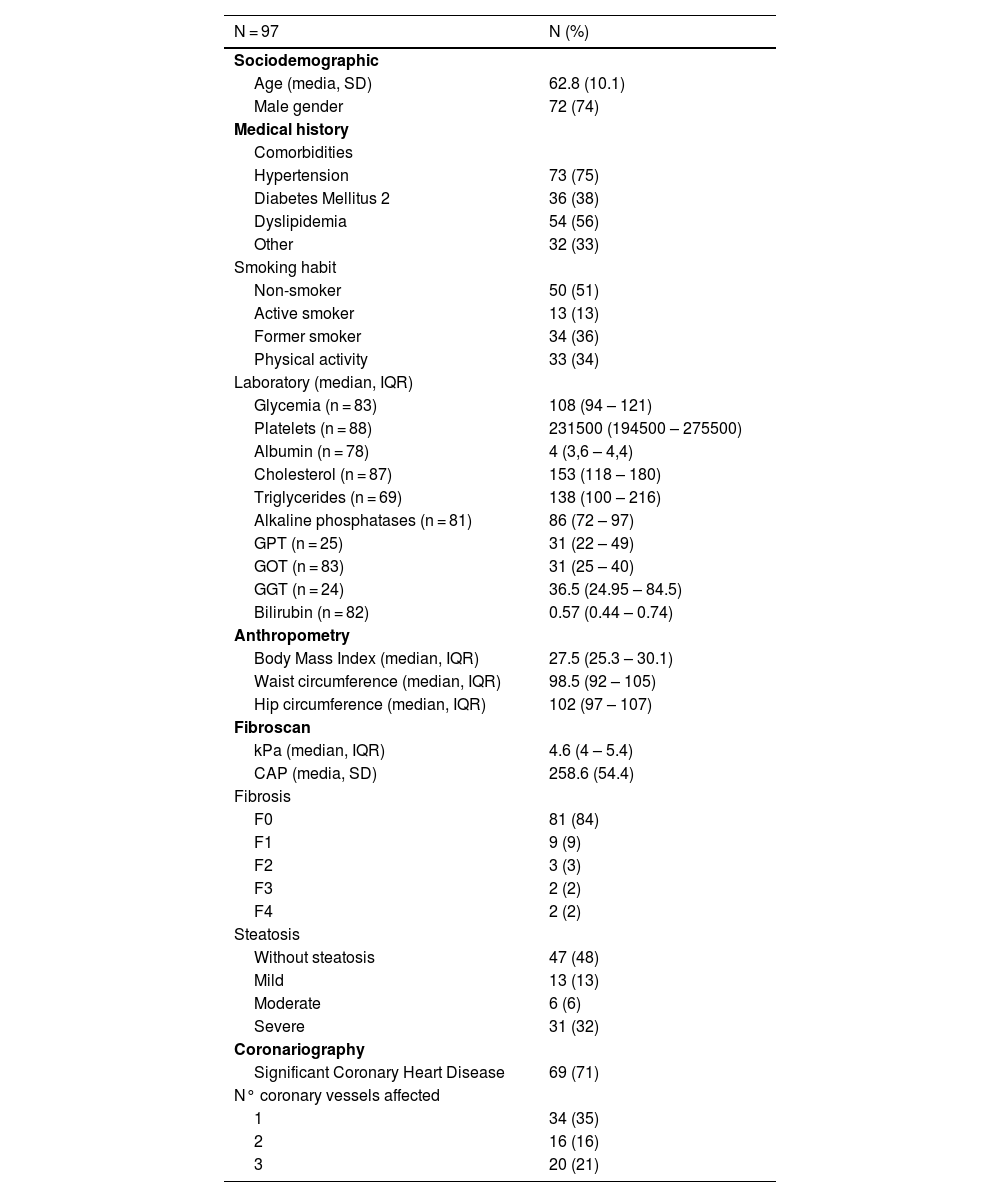
ResultsNinety-seven patients were included, 73% male, age 63 ± 10 years (Table 1). 71% presented significant CHD, with 37% multivessel disease (2 or more). The prevalence of NAFLD was 38%, with no differences between those with and without CHD (43% vs. 36%, p=0.646). In turn, 16% of patients presented some degree of fibrosis, linearly associated with the number of vessels involved (OR=1.8, p=0.022), with an even higher risk in patients with two or more vessels involved (OR=3.5, p=0.027).
ConclusionsThere is a high prevalence of NAFLD in patients with CHD, with no differences between patients with significant stenosis vs not. Patients with multivessel disease have higher odd of presenting some degree of fibrosis. Although the presence of confounders should be evaluated in other studies, these data support the search for NAFLD and fibrosis in patients with CHD.
Table 1. Characterization of the patients included in the project