Stress urinary incontinence (SUI) is a common disorder in women that has a negative impact on quality of life. Pregnancy and childbirth are considered important risk factors that directly affect the pelvic floor during pregnancy and labour, increasing the risk of pelvic floor dysfunction, with prevalence rates of SUI in the postpartum period ranging from 30 to 47% during the first 12 months.
ObjectiveTo determine the effectiveness of pelvic floor muscle training (PFMT) in the prevention of SUI in women during the antenatal and postnatal period by reviewing and evaluating the available scientific literature.
MethodsThis is a systematic review, using only randomised controlled trials. We searched the databases Pubmed, Scopus, Cochrane and PEDro. We reviewed 7 prospective studies in English and Portuguese, which included 1,401 pregnant women of legal age who underwent PFMT to prevent SUI.
ResultsThe results allowed us to establish that PFMT is used for pelvic floor muscles and that this intervention, applied with the appropriate methodology, can prevent or cure SUI.
ConclusionsThe application of PFMT in an early stage of pregnancy has positive effects on the continence capacity after delivery.
La incontinencia urinaria de esfuerzo es una alteración común en las mujeres que repercute de forma negativa en la calidad de vida. El embarazo y el parto son considerados factores de riesgo importantes, afectando directamente el suelo pélvico durante el embarazo y el trabajo de parto, aumentando el riesgo de disfunciones del suelo pélvico, encontrándose tasas de prevalencia de IUE en el postparto del 30al 47% durante los primeros 12 meses.
ObjetivoDeterminar la efectividad del entrenamiento del suelo pélvico (EMSP) en la prevención de la incontinencia urinaria de esfuerzo (IUE) en mujeres, durante el periodo prenatal y el posparto, mediante la revisión y la evaluación de la literatura científica disponible.
MétodosRevisión sistemática, que usó como objeto de estudio exclusivamente Ensayos Controlados Aleatorios. Se realizaron búsquedas en las bases de datos Pubmed, Scopus, Cochrane y PEDro. Se evaluaron 7 estudios prospectivos en idiomas inglés y portugués, que incluyeron 1.401 mujeres embarazadas sometidas a EMSP, para prevenir la IUE.
ResultadosLos resultados permitieron identificar que el EMSP se utiliza para prevenir la IUE en los músculos del suelo pélvico.
ConclusionesAplicación del EMSP en una fase temprana del embarazo tienen efectos positivos sobre la capacidad de continencia después del parto.
According to the WHO, urinary incontinence (UI) is defined as “the involuntary loss of urine which causes a hygienic and/or social problem, and that can be objectively demonstrated”.1 At present, a large number of authors consider pregnancy, obstetric vaginal trauma, episiotomy, and the use of forceps to be the main risk factors for stress urinary incontinence (SUI) in women, causing irreversible anatomical lesions in the pelvic floor, reducing the capacity of the muscles to support the pelvic organs, and producing alterations in the function of the pudendal nerve.2
Additional factors that may be involved with SUI in women are hormonal changes, increased pressure on abdominal and pelvic floor muscles due to fetal development, gestational diabetes, and increased body mass index (BMI); an increase of every five units of BMI increases the risk of postpartum SUI prevalence from 30 to 64% during the first 12 months.3 However, the reported prevalence of SUI during the gestational period ranges from 18.6% to 75%.4
Studies have been carried out involving the participation of physiotherapy and professionals specialized in the area of pelvic floor rehabilitation through the use of biofeedback, TENS electrostimulation, vaginal cones,5,6 as well as supporting the importance of pelvic floor muscle training (PFMT) to correct the functions of the pelvic floor muscles and inhibit UI.7,8 PFMT is indicated in pregnant women during the prenatal and postnatal period, except in cases of high-risk pregnancy. Even so, controversy does exist regarding its application during gestation or after the puerperium. The objective of this review is to determine the effectiveness of PFMT in the prevention of SUI in pregnant women during the prenatal and postpartum period, as a tool that seeks to eliminate the causes of the pathology, detect asymptomatic dysfunction, and be used for early treatment in order to interrupt progression.
MethodsDesignA systematic review was carried out. We specifically sought randomized controlled trials (RCTs) in English, Spanish, and Portuguese that investigated the effectiveness of pelvic floor muscle training (PFMT) to prevent SUI. The inclusion criteria for the review required that women were intervened during the pregnancy and/or postpartum period, whose interventions were protocols or exercise programs for strengthening and rehabilitation of the pelvic floor, that evaluated the strength of the pelvic floor musculature, the capacity for continence before or after childbirth, and that these interventions had a comparative with a control group or other therapies on the same variables to be treated. The exclusion criteria were studies in sportswomen, postmenopausal women, or women with underlying pathologies such as osteoporosis, diabetes, women with high-risk pregnancies, and those studies where the therapy was directed by a professional other than a physiotherapist.
A computerized search of the PubMed databases was performed using the following search terms: (((“Urinary Incontinence, Stress”[Mesh]) AND “Postpartum Period”[Mesh]) AND “prevention and control” [Subheading]) AND “Pelvic Floor”[Mesh] AND “Female”[Mesh]) AND “Exercise Therapy”[Mesh]. The advanced search in PEDro used the terms “Urinary Incontinence, Stress, Postpartum Prevention, Control, Female, Care, Exercise, Pregnancy, Methods, Pelvic Floor”. The terms implemented for the search in the Cochrane database were: Urinary Incontinence, Stress OR Postpartum Period OR Prevention OR Prenatal Care OR Pelvic Floor Training OR Pregnancy. Finally, for the Scopus database the terms used were: “Urinary Incontinence, Stress AND Exercise Therapy/Methods AND Prenatal Care/Methods AND Postpartum Period AND Exercise Therapy AND Control & Prevention”.
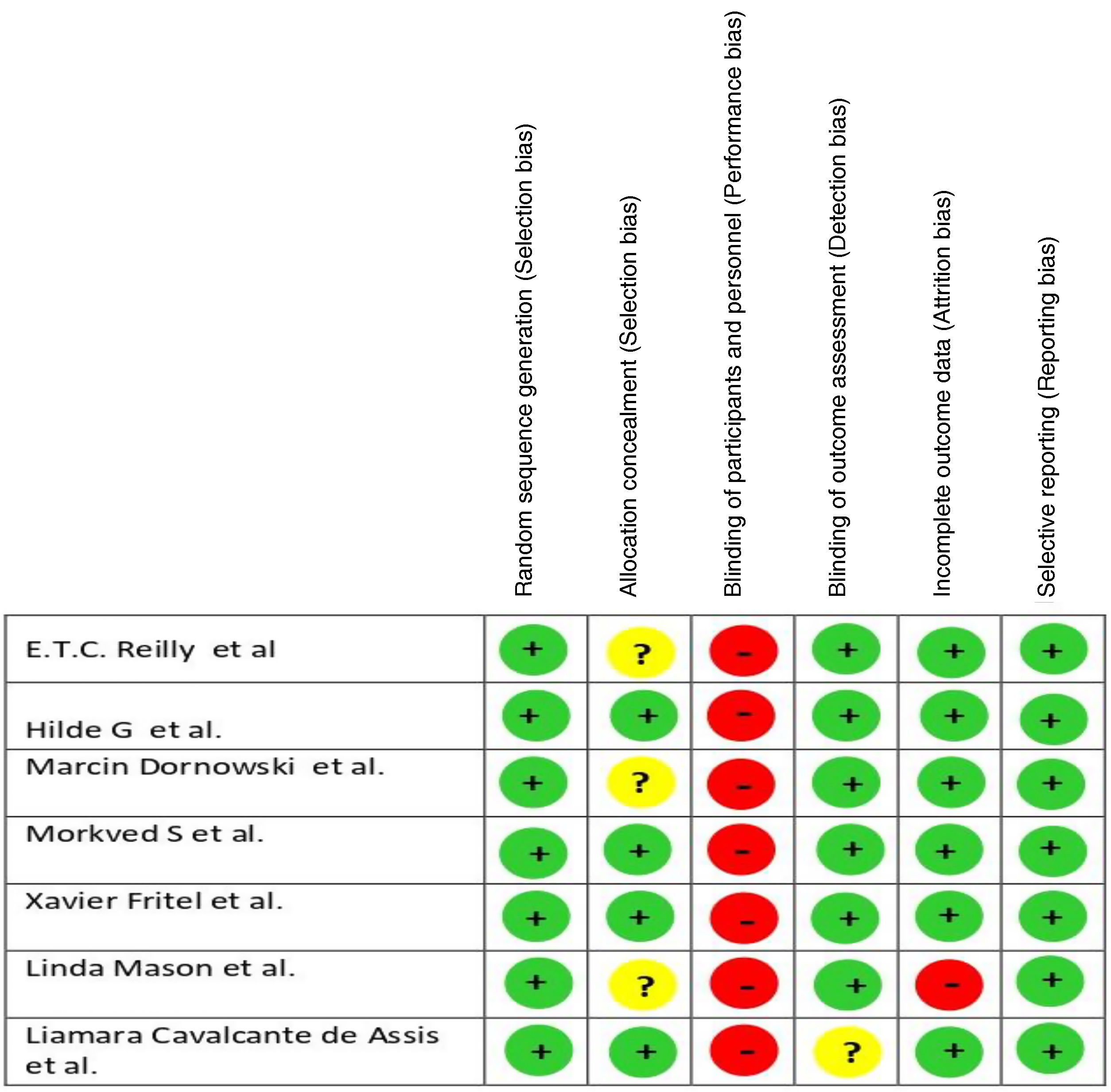
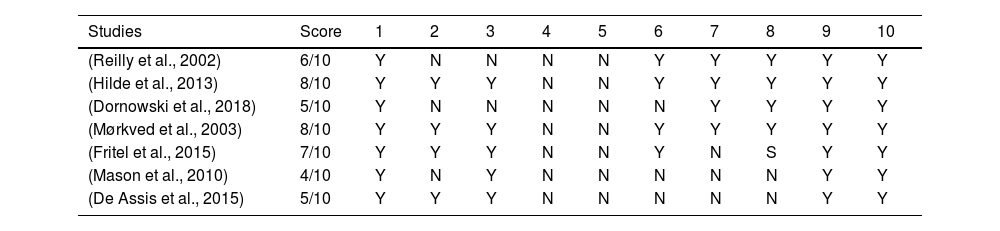
Quality assessmentThe methodological limitations of each of the trials were considered. The PEDro scale was used to quickly identify trials that tend to be internally valid and have sufficient statistical information to guide clinical decision making9 (“PEDro Statistics – PEDro”). The risk of bias in the RCTs was assessed following the Cochrane Handbook of Systematic Reviews of Interventions Version 5.1.0.10
All studies were assessed for possible sources of selection bias, performance bias, detection bias, attrition bias, and reporting bias. The risk of bias among studies was described and judged in categories of low, unclear, and high risk of bias, according to criteria established by Cochrane.10 Two investigators rated and scored each trial individually; disagreements were resolved by consensus or by a third reviewer.
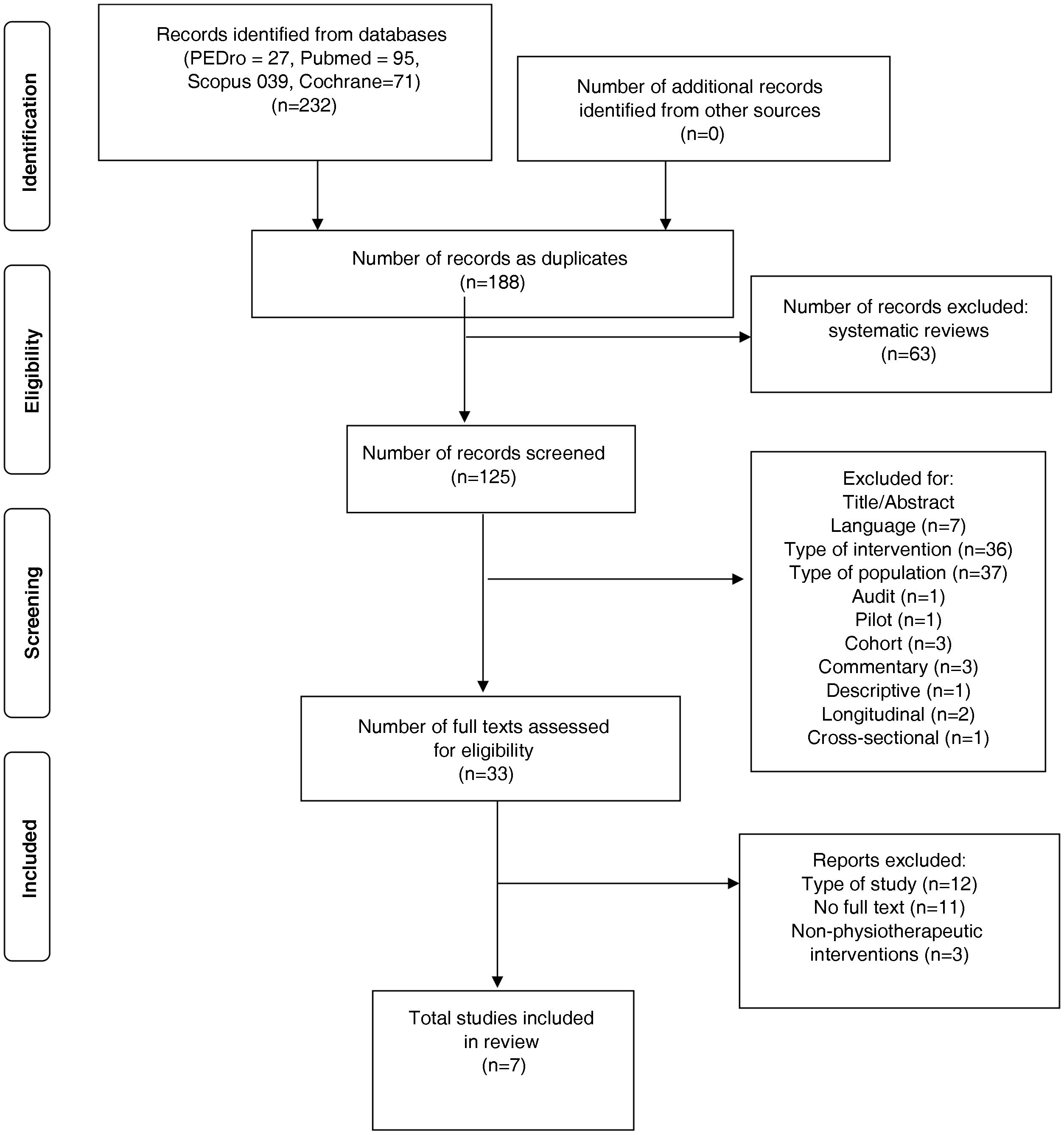
Study selectionThe electronic search identified 232 studies, among which 7 randomized controlled trials were selected because they met the previously defined criteria. A PRISMA diagram of the search results, including the reasons for exclusion, is shown in Fig. 1.
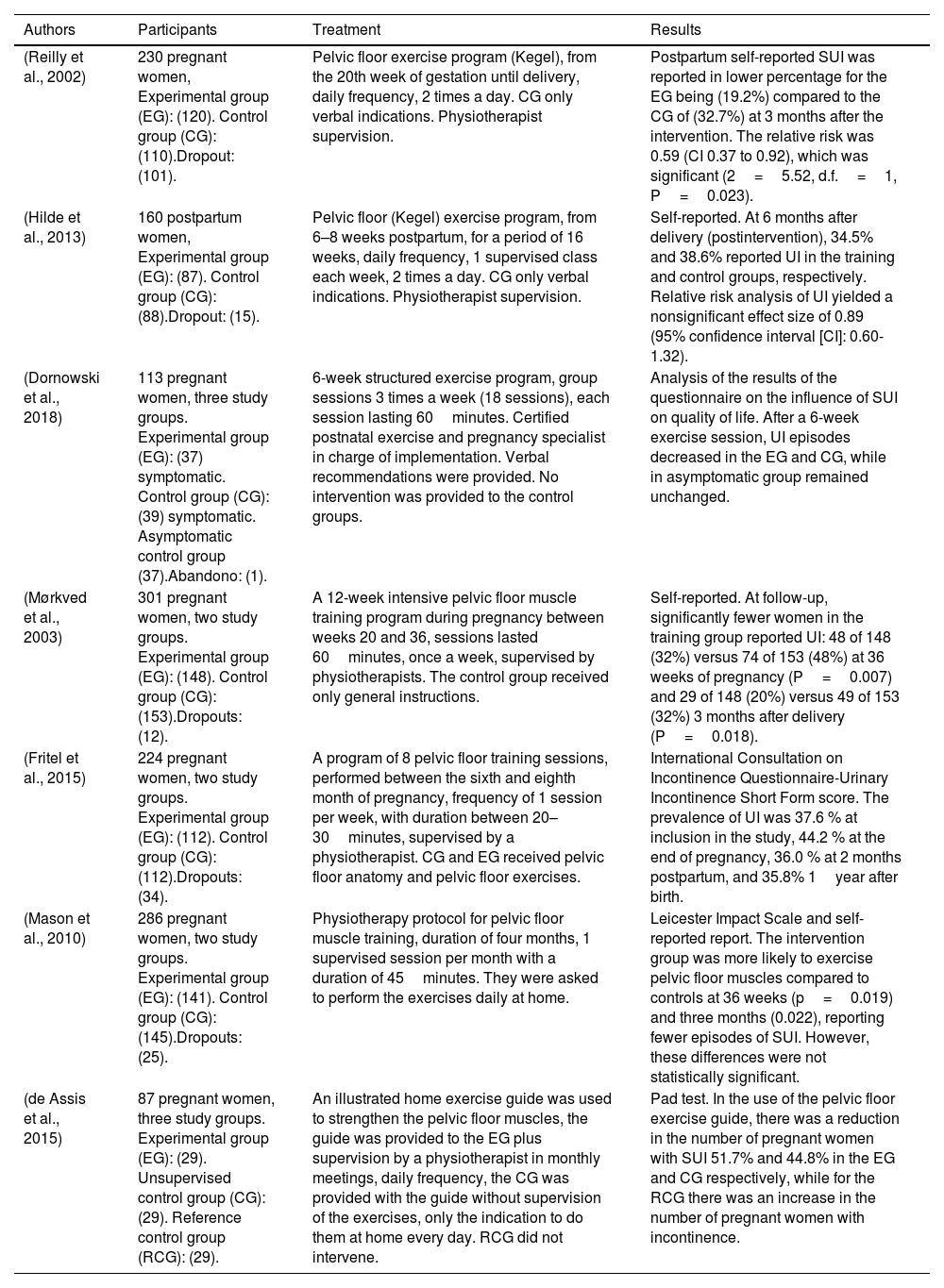
Description of the studiesTable 1 summarizes the included studies (n=7). A summary of the interventions and results of each of the seven included studies is presented.
Summary of the included studies (n=7).
| Authors | Participants | Treatment | Results |
|---|---|---|---|
| (Reilly et al., 2002) | 230 pregnant women, Experimental group (EG): (120). Control group (CG): (110).Dropout: (101). | Pelvic floor exercise program (Kegel), from the 20th week of gestation until delivery, daily frequency, 2 times a day. CG only verbal indications. Physiotherapist supervision. | Postpartum self-reported SUI was reported in lower percentage for the EG being (19.2%) compared to the CG of (32.7%) at 3 months after the intervention. The relative risk was 0.59 (CI 0.37 to 0.92), which was significant (2=5.52, d.f.=1, P=0.023). |
| (Hilde et al., 2013) | 160 postpartum women, Experimental group (EG): (87). Control group (CG): (88).Dropout: (15). | Pelvic floor (Kegel) exercise program, from 6–8 weeks postpartum, for a period of 16 weeks, daily frequency, 1 supervised class each week, 2 times a day. CG only verbal indications. Physiotherapist supervision. | Self-reported. At 6 months after delivery (postintervention), 34.5% and 38.6% reported UI in the training and control groups, respectively. Relative risk analysis of UI yielded a nonsignificant effect size of 0.89 (95% confidence interval [CI]: 0.60-1.32). |
| (Dornowski et al., 2018) | 113 pregnant women, three study groups. Experimental group (EG): (37) symptomatic. Control group (CG): (39) symptomatic. Asymptomatic control group (37).Abandono: (1). | 6-week structured exercise program, group sessions 3 times a week (18 sessions), each session lasting 60minutes. Certified postnatal exercise and pregnancy specialist in charge of implementation. Verbal recommendations were provided. No intervention was provided to the control groups. | Analysis of the results of the questionnaire on the influence of SUI on quality of life. After a 6-week exercise session, UI episodes decreased in the EG and CG, while in asymptomatic group remained unchanged. |
| (Mørkved et al., 2003) | 301 pregnant women, two study groups. Experimental group (EG): (148). Control group (CG): (153).Dropouts: (12). | A 12-week intensive pelvic floor muscle training program during pregnancy between weeks 20 and 36, sessions lasted 60minutes, once a week, supervised by physiotherapists. The control group received only general instructions. | Self-reported. At follow-up, significantly fewer women in the training group reported UI: 48 of 148 (32%) versus 74 of 153 (48%) at 36 weeks of pregnancy (P=0.007) and 29 of 148 (20%) versus 49 of 153 (32%) 3 months after delivery (P=0.018). |
| (Fritel et al., 2015) | 224 pregnant women, two study groups. Experimental group (EG): (112). Control group (CG): (112).Dropouts: (34). | A program of 8 pelvic floor training sessions, performed between the sixth and eighth month of pregnancy, frequency of 1 session per week, with duration between 20–30minutes, supervised by a physiotherapist. CG and EG received pelvic floor anatomy and pelvic floor exercises. | International Consultation on Incontinence Questionnaire-Urinary Incontinence Short Form score. The prevalence of UI was 37.6 % at inclusion in the study, 44.2 % at the end of pregnancy, 36.0 % at 2 months postpartum, and 35.8% 1year after birth. |
| (Mason et al., 2010) | 286 pregnant women, two study groups. Experimental group (EG): (141). Control group (CG): (145).Dropouts: (25). | Physiotherapy protocol for pelvic floor muscle training, duration of four months, 1 supervised session per month with a duration of 45minutes. They were asked to perform the exercises daily at home. | Leicester Impact Scale and self-reported report. The intervention group was more likely to exercise pelvic floor muscles compared to controls at 36 weeks (p=0.019) and three months (0.022), reporting fewer episodes of SUI. However, these differences were not statistically significant. |
| (de Assis et al., 2015) | 87 pregnant women, three study groups. Experimental group (EG): (29). Unsupervised control group (CG): (29). Reference control group (RCG): (29). | An illustrated home exercise guide was used to strengthen the pelvic floor muscles, the guide was provided to the EG plus supervision by a physiotherapist in monthly meetings, daily frequency, the CG was provided with the guide without supervision of the exercises, only the indication to do them at home every day. RCG did not intervene. | Pad test. In the use of the pelvic floor exercise guide, there was a reduction in the number of pregnant women with SUI 51.7% and 44.8% in the EG and CG respectively, while for the RCG there was an increase in the number of pregnant women with incontinence. |
The methodological quality score of the included trials ranged from 8 to 4 with a mean of 6.1. The criteria met by each of the included trials are shown in Table 2.
PEDro scale criteria and ratings for the included studies (n=7).
| Studies | Score | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| (Reilly et al., 2002) | 6/10 | Y | N | N | N | N | Y | Y | Y | Y | Y |
| (Hilde et al., 2013) | 8/10 | Y | Y | Y | N | N | Y | Y | Y | Y | Y |
| (Dornowski et al., 2018) | 5/10 | Y | N | N | N | N | N | Y | Y | Y | Y |
| (Mørkved et al., 2003) | 8/10 | Y | Y | Y | N | N | Y | Y | Y | Y | Y |
| (Fritel et al., 2015) | 7/10 | Y | Y | Y | N | N | Y | N | S | Y | Y |
| (Mason et al., 2010) | 4/10 | Y | N | Y | N | N | N | N | N | Y | Y |
| (De Assis et al., 2015) | 5/10 | Y | Y | Y | N | N | N | N | N | Y | Y |
Note. N: (No) Y: (Yes). 1: Random sequence generation; 2: Allocation concealment; 3: Homogeneous groups; 4: Blinding of patients; 5: Blinding of therapists; 6: Blinding of outcome assessment; 7: Results from more than 85% of subjects; 8: Intention to treat analyses; 9: Between-group comparisons; 10: Point measures for at least one key outcome.
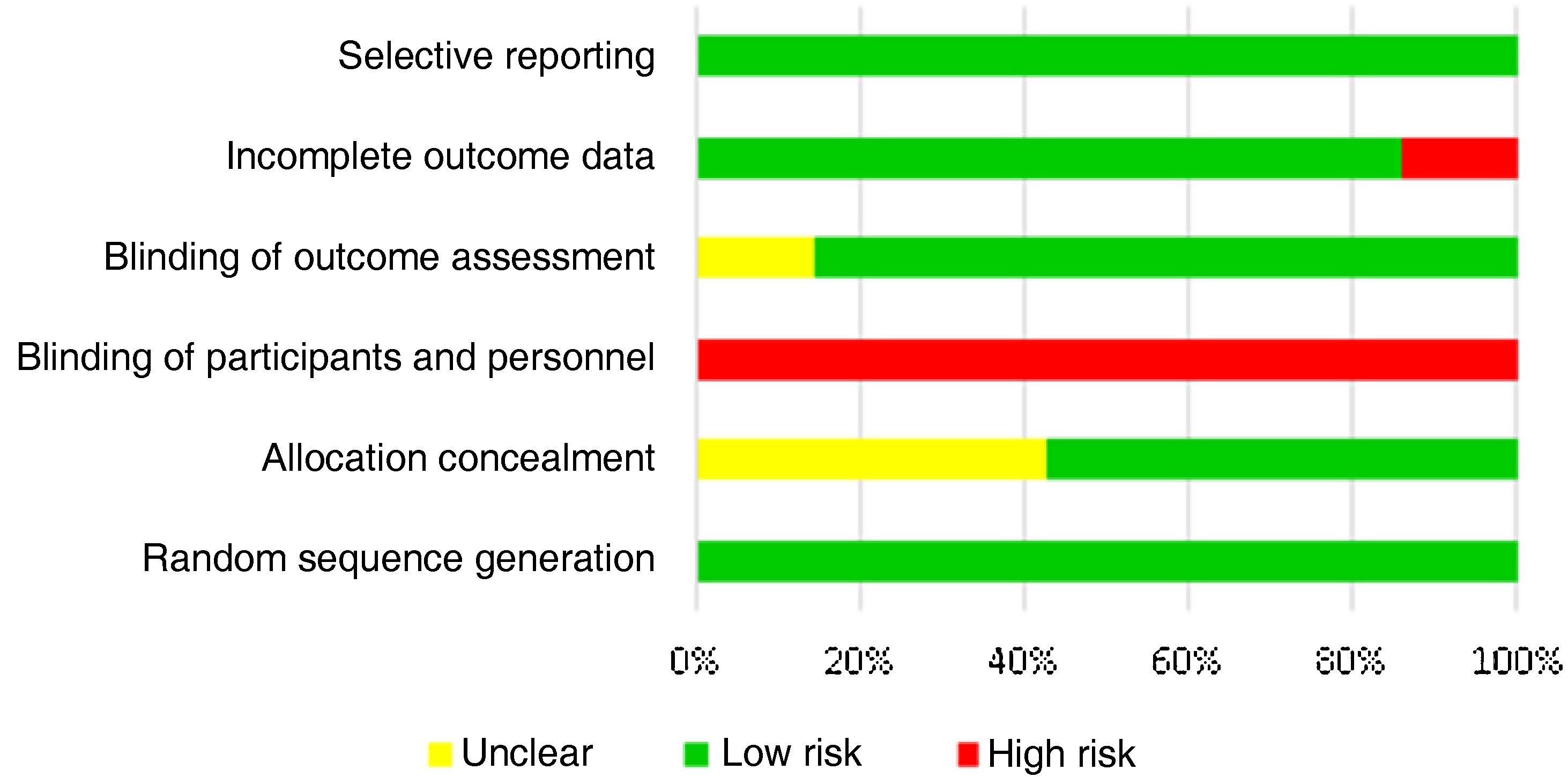
The summary of the risk of bias assessment is presented in Fig. 2. Overall, the included studies were at low risk of bias, mainly observational, with respect to the influence of PFMT on urinary incontinence in pregnancy or the puerperium. Fig. 3 shows the authors’ judgments on each element of risk of bias presented as percentages in all included studies.
ResultsIn the description of interventions, significant improvements were found for SUI after the application of pelvic floor training after childbirth.11,12 However, three studies13–15 did not demonstrate significant differences in self-reported UI after intervention. Regarding objective measurement of UI, two studies used the pad test for which no significant differences were found between the experimental and control groups.13,14 In contrast, three studies11,12,15 did not use this test for similar reasons (to avoid inducing urinary tract infections).
On the other hand, the strength of the pelvic floor muscles before and after the intervention was measured with various instruments (perineometer, manometer, Laycock scale, electromyography). Therefore, the improvements observed in the intervention group in terms of strength parameters were significant in three articles.11–13 However, in one study no clinically significant differences were reported although there was an increase in strength.14 Only one study did not take into account the assessment of pelvic muscle strength for its analysis even though a previous evaluation was taken into account for the verification of adequate contraction.15 The studies demonstrated significant improvements associated with early intervention from the prenatal period, starting with a pelvic floor strengthening exercise program where participants came to decrease the risk of presenting stress urinary incontinence.
DiscussionPFMT is used to strengthen the periurethral muscles to improve the continence mechanism.8 The results of PFMT, however, are mediated by patient variables such as mood, motivation, and degree of health engagement.16,17 Prescription of PFMT during the gestational period reduces the prevalence of SUI in late pregnancy and early postpartum.18,19 In our review we found seven randomized trials investigating the effects of PFMT methods for the prevention of stress urinary incontinence and pelvic floor muscle strength, which provide data confirming the effectiveness of PFMT, but with different periods of application.11–15 It is suggested that interventions with PFMT begin at 20 weeks of gestation, with improvements in pelvic floor muscle strength and SUI20,21 and they conclude that PFMT with a frequency of 3 weekly sessions for 22 weeks during the gestation period is effective for the prevention of SUI.
Nonetheless, in the study by Assis et al., 201512 when starting the intervention from week 18 of gestation, significant improvements were reported at week 23 in an increase in pelvic floor muscle strength and a decrease in SUI. On the other hand, Dornowski et al., 2018,11 while not describing from which week of gestation they perform their intervention, they demonstrate that good results can be obtained after applying a 6-week program. For their part, Fritel et al., 201514 differ in their results with respect to interventions carried out during the gestation period. They employed a PFMT program consisting of 8 sessions between 26 and 34 weeks, with a frequency of one session per week, demonstrating that there was no significant effect. This may be due to patient awareness and the actual practice of PFMT by not complying with the established guidelines and poor adherence to the program that the participants had to follow at home.22,23
All of our findings about PFMT as an intervention for SUI in the seven included trials11–15 suggest that face-to-face supervision by physical therapy professionals specializing in the area of pelvic floor training is important.18,24 Women performing PFMT with verbal and manual instructions on a daily basis had lower self-report of SUI.
Other authors25–28 base their interventions on an PFMT program based on mobile applications or videos, with asynchronous meetings, highlighting that this modality can be a low-cost alternative based on technology that provides good results.
It can be said that PFMT performed during gestation and after delivery is effective for the prevention of SUI and treatment in reducing its symptoms. In addition, there is greater adherence of the participants under close supervision, and no differences were found in the results between group or individual supervision,11,12 demonstrating that both modalities are equally successful, with improvements being found 9 months after childbirth.29
It is worth mentioning that the mixed approaches of individualized follow-up combined with group sessions showed significant improvements in the reduction of SUI.29 However, individualized sessions generate a greater commitment in the participants in the execution of the exercises, which guarantees greater adherence, follow-up control, and a clinically significant increase in the reduction of SUI symptoms and increase in the strength of the periurethral muscles.12–15 In addition, there is a reduction in the prevalence of postpartum SUI after applying an PFMT program with supervision during the gestational period in women11,12,21,29 rather than the application of the same during the postnatal period only.
On the other hand, the lack of adherence to pelvic floor muscle training interventions leads to a high number of dropouts,11,13,14,15,30 so it is suggested that emphasis be placed on fundamental aspects such as patient education, motivation, and adherence. Finally, the PFMT protocols used in the included studies reported no adverse effects, which suggests they are a safe alternative for the prevention of SUI.
ConclusionsThis review has found that the application of PFMT early in pregnancy has positive effects on urinary continence after childbirth. The application of protocols that include individualized instruction and adequate follow-up by a physical therapist allows women to increase adherence to pelvic floor training, as well as possibly promoting motivation and awareness for proper performance of these exercises during interventions and at home.
It is not clear what the optimal dose of PFMT is. However, a training protocol that follows the general principles of strength training, emphasizing near-maximal contractions and at least a 6-week training period, emphasizing strenuous intensity training, may be as effective as a 4-month training at moderate intensity. It is important to develop new studies to determine the intensity, time of application, and number of repetitions of each exercise for the prevention of SUI in late pregnancy and postpartum.
Limitations of the studyThis systematic review has been based on the best possible evidence through RCTs. Even so, it does have limitations. One of them is the heterogeneity in the study variables: type of delivery, duration of incontinence, associated symptoms. Similarly, a variety of instruments were found to measure the study variables and pelvic floor muscle training regimens in terms of intensity, frequency, time, and duration. Another limitation is the possible biases related to the blinding of the therapist and the patient.
Conflict of interestThe authors have no conflict of interest to declare.