The aim of this work is to evaluate the initial experience with water vapor thermal therapy (WVTT) for benign prostatic hyperplasia (BPH) in Spanish university hospitals, as well as to describe the differences in technique and follow-up between centers.
Materials and MethodsThis retrospective observational multicenter study collected baseline characteristics, surgical, postoperative and follow-up data at 1, 3, 6, 12 and 24 months, including validated questionnaires, flowmetric variations, complications, and the need for pharmacological or surgical treatment following the procedure. Possible triggers for postoperative acute urinary retention (AUR) were also analyzed.
ResultsA total of 105 patients were included. No differences were observed between the groups with and without AUR with respect to catheterization time (5 and 4.3 days respectively, P=.178), or prostate volume (47.9g and 41.4g respectively, P=.147). The mean improvement at 3, 6, 12 and 24 months in terms of peak flow was 5.3, 5.2, 4.2 and 3.8ml/s, respectively. As for ejaculation, an improvement was observed after 3 months of follow-up and was maintained over time.
ConclusionsMinimally invasive treatment for BPH with WVTT shows good functional outcomes at 24 months follow-up, without significant impairment of sexual function and a low incidence of complications. There are minor inter-hospital variations, mainly in the immediate postoperative period.
El objetivo de este trabajo es conocer experiencia inicial con la terapia térmico con vapor de agua (TTVA) para hiperplasia benigna de próstata en los hospitales universitarios españoles, así como describir las diferencias en cuanto a técnica y a seguimiento observadas entre los centros.
Materiales y métodoEste estudio multicéntrico observacional retrospectivo recogió características basales, datos quirúrgicos, postoperatorios y seguimiento a los 1, 3, 6, 12 y 24 meses, incluyendo cuestionarios validados, variaciones flujométricas, complicaciones y la necesidad de tratamiento farmacológico u quirúrgico tras el procedimiento. También se analizaron los posibles desencadenantes de retención aguda de orina (RAO) en el postoperatorio.
ResultadosSe incluyeron un total de 105 pacientes. No se observaron diferencias entre los grupos con y sin RAO con respecto a tiempo de sondaje (5 y 4.3 días respectivamente, P=.178), ni volumen prostático (47.9g y 41.4g respectivamente, P=.147). La mejoría media a los 3, 6, 12 y 24 meses en cuanto de flujo máximo fue de 5.3, 5.2, 4.2 y 3.8ml/s, respectivamente. En cuanto a la eyaculación, se observa una mejoría en la misma a partir de los 3 meses de seguimiento que se mantiene en el tiempo.
ConclusionesEl tratamiento mínimamente invasivo de HBP con TTVA presenta buenos resultados funcionales a 24 meses de seguimiento, sin afectación significativa de la función sexual y con una baja incidencia de complicaciones. Existen pequeñas variaciones principalmente en cuanto a postoperatorio inmediato en entre los hospitales participantes en el estudio.
Bladder outlet obstruction (BOO) caused by benign prostatic hyperplasia (BPH) is one of the most common urinary disorders in the aging male.1 Minimally invasive treatments constitute a growing alternative in the treatment armamentarium of BOO.2,3
Water vapor thermal therapy (WVTT, Rezūm System, Boston Scientific, Marlborough, MA) uses radiofrequency current to generate thermal energy in the form of water vapor (540 calories/mL H2O). The water vapor travels through cell interstices until it meets the tissue plane boundary between prostatic zones. Consequently, it denatures cell membranes and produces prostate tissue necrosis.4,5
There is good quality evidence on the safety and effectiveness of the treatment effect on BPH symptoms in the medium term, and on the potential preservation of sexual function of this treatment compared to pharmacological treatment for BPH.6–8
The aims of this work are to obtain information on the initial experience with WVTT in Spanish university hospitals, to describe the evolution and complications of the patients after the intervention, and to determine the differences of treatment protocols among the participating centers.
Materials and methodsStudy design and patient selectionWe conducted a multicenter, retrospective, observational study including 6 Spanish public university hospitals. The study was approved by the Drug Research Ethics Committee of the main researcher's center (C2022/13). We included the first patients undergoing WVTT in each hospital participating in the study, who were not catheterized at the time of the intervention, with prostate volumes between 30 and 80ml and with maximum flow (Qmax)<15ml/s on uroflowmetry with a voided volume>150ml.
VariablesFollow-up data were collected at 1, 3, 6, 12, and 24 months. These included baseline characteristics, IPSS (International Prostate Symptom Score), International Index of Erectile Function (IIEF), Male Sexual Health Questionnaire-Ejaculatory Dysfunction (MSHQ-EjD) scores, uroflowmetry findings, complications, and the need for pharmacological or surgical retreatment following the procedure.
We performed a detailed analysis of the possible causes of acute urinary retention (AUR) after bladder catheter (BC) removal, comparing baseline prostate volume, number of intraprostatic injections and BC days between patients who presented postoperative AUR and those who did not.
ProcedureThe specific intra and postoperative protocols were defined by each participating center. Prostate volume and the presence of prostate median lobe confirmed by transabdominal or transrectal ultrasound, the number of intraprostatic injections per procedure, postoperative treatment, and time to bladder catheter (BC) removal were collected.
Statistical analysisFor quantitative variables, measures of central tendency and dispersion were provided. In addition, normality tests were performed using the Shapiro-Wilk test. Valid percentages were shown in the case of qualitative variables.
Sociodemographic and clinical data were compared based on patients AUR status (with and without postoperative AUR) with the Mann-Whitney U test Changes in the main study variables (IIEF, MSHQ, IPPS and Qmax) were analyzed using the Wilcoxon test. In addition, patient characteristics were compared according to the hospital of origin using the Kruskal-Wallis test. The R Studio (V2.5) statistical program was used. Statistical significance was determined as a value of P<.05.
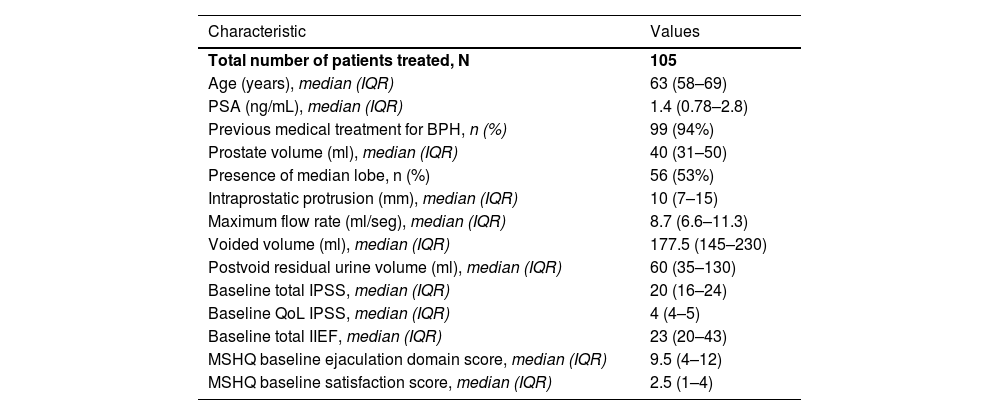
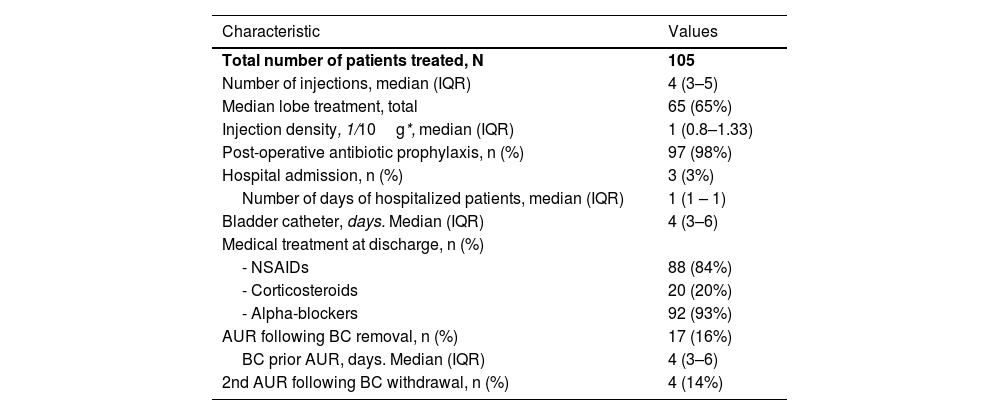
ResultsBaseline characteristicsA total of 105 patients treated with WVTT between 1/1/2019 and 1/7/2022 were included in the study. Baseline characteristics are collected in Table 1. Intra and postoperative data are reported in Table 2. Ninety-four percent of patients (99 in total) were receiving treatment for BPH prior to surgery, 93 with α-blockers, 43 with 5 α-reductase inhibitors (I5AR), 2 with IPDE5 and 2 with phytotherapy. The median mean number of intraprostatic injections was 4 (RIC: 3–5) with a median injection density of 1 per 10g prostate volume (RIC: 0.8–1.33).
Baseline characteristics of patients undergoing water vapor thermal therapy.
| Characteristic | Values |
|---|---|
| Total number of patients treated, N | 105 |
| Age (years), median (IQR) | 63 (58–69) |
| PSA (ng/mL), median (IQR) | 1.4 (0.78–2.8) |
| Previous medical treatment for BPH, n (%) | 99 (94%) |
| Prostate volume (ml), median (IQR) | 40 (31–50) |
| Presence of median lobe, n (%) | 56 (53%) |
| Intraprostatic protrusion (mm), median (IQR) | 10 (7–15) |
| Maximum flow rate (ml/seg), median (IQR) | 8.7 (6.6–11.3) |
| Voided volume (ml), median (IQR) | 177.5 (145–230) |
| Postvoid residual urine volume (ml), median (IQR) | 60 (35–130) |
| Baseline total IPSS, median (IQR) | 20 (16–24) |
| Baseline QoL IPSS, median (IQR) | 4 (4–5) |
| Baseline total IIEF, median (IQR) | 23 (20–43) |
| MSHQ baseline ejaculation domain score, median (IQR) | 9.5 (4–12) |
| MSHQ baseline satisfaction score, median (IQR) | 2.5 (1–4) |
PSA, Prostate Specific Antigen; IIEF, International Index of Erectile Function Questionnaire; MSHQ-EjD, Male Sexual Health Questionnaire-Ejaculatory Dysfunction; IPSS, International Prostate Symptom Score; QoL, Quality of Life, QoL section of the IPSS; IQR, interquartile range.
Surgical and postoperative data of water vapor thermal therapy.
| Characteristic | Values |
|---|---|
| Total number of patients treated, N | 105 |
| Number of injections, median (IQR) | 4 (3–5) |
| Median lobe treatment, total | 65 (65%) |
| Injection density, 1/10g*, median (IQR) | 1 (0.8–1.33) |
| Post-operative antibiotic prophylaxis, n (%) | 97 (98%) |
| Hospital admission, n (%) | 3 (3%) |
| Number of days of hospitalized patients, median (IQR) | 1 (1 – 1) |
| Bladder catheter, days. Median (IQR) | 4 (3–6) |
| Medical treatment at discharge, n (%) | |
| - NSAIDs | 88 (84%) |
| - Corticosteroids | 20 (20%) |
| - Alpha-blockers | 92 (93%) |
| AUR following BC removal, n (%) | 17 (16%) |
| BC prior AUR, days. Median (IQR) | 4 (3–6) |
| 2nd AUR following BC withdrawal, n (%) | 4 (14%) |
NSAIDs, Non-steroidal anti-inflammatory drugs; AUR, Acute urinary retention; BC, Bladder catheter.
In total, 3 patients (3%) presented complications that required hospitalization. In all cases, hospitalization was only for one day and the reasons were fever in one case, and vasovagal symptoms in 2 cases (Clavien-Dindo I-II). After discharge, 7 patients (6.7%) presented urinary tract infection requiring additional antibiotic treatment and 2 patients (1.9%) presented hematuria requiring manual bladder washout.
The median bladder catheterization time after the procedure was 4 days (ICR: 3–6), and this duration was determined by each hospital. Seventeen patients (16%) presented AUR after the first bladder catheter removal, and 4 patients (3.8%) presented a second episode of AUR. No differences were observed between the groups with and without AUR regarding median catheterization time (5 and 4.3 days respectively, P=.178), prostate volume (47.9g and 41.4g respectively, P=.147), or the number of intraprostatic injections (5.25 and 4.5 respectively, P=.266).
Flowmetry and IPSS evolutionThe number of patients that were followed up at 3, 6, 12 and 24 months was 105, 86, 75 and 60, respectively. Follow-up included uroflowmetry, IPSS questionnaire, and the quality-of-life section of the IPSS questionnaire (QoL). As for the evaluation of sexual function, 4 hospitals used with the IIEF questionnaire and 2 used the MSHQ-EjD.
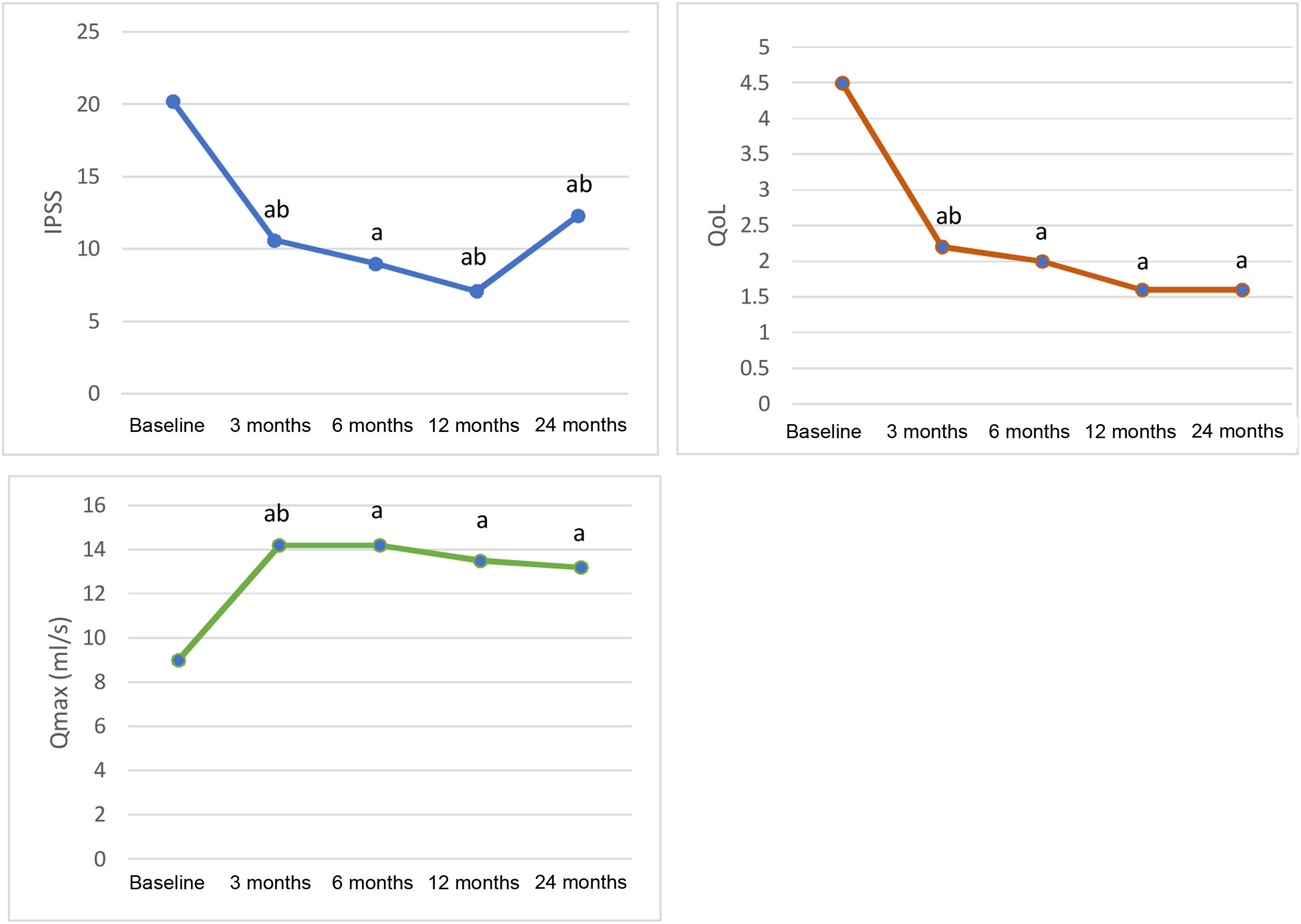
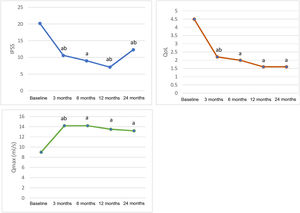
Fig. 1 shows the evolution of Qmax, IPSS and QoL values. A statistically significant improvement from baseline was observed in all 3 parameters, which was maintained over time. The mean improvement at 3, 6, 12 and 24 months for Qmax was 5.3, 5.2, 4.2 and 3.8ml/s, respectively (from baseline P<.05), for IPSS was 9.2, 11.2, 13.1, 7.1 points, respectively (from baseline P<.05), and for QoL was 2.3, 2.5, 2.9 and 2.9 points, respectively (from baseline P<.05).
Evolution of peak flow (Qmax), IPSS and QoL scores.
IPSS: International Prostate Symptom Score. QoL: Quality of Life, QoL section of the IPSS. Qmax: Maximum flow rate measured in mL/s by uroflowmetry. aP<.05 vs. baseline visit (Wilcoxon Test). bP<.05 vs. previous visit (Wilcoxon Test).
The median lobe was treated in 65 patients (62%). Only 5 patients with the median lobe identified in preoperative ultrasound did not receive treatment for it. These 5 patients showed a mean Qmax improvement at 6 months of 3.16ml/s, somewhat lower than the overall mean.
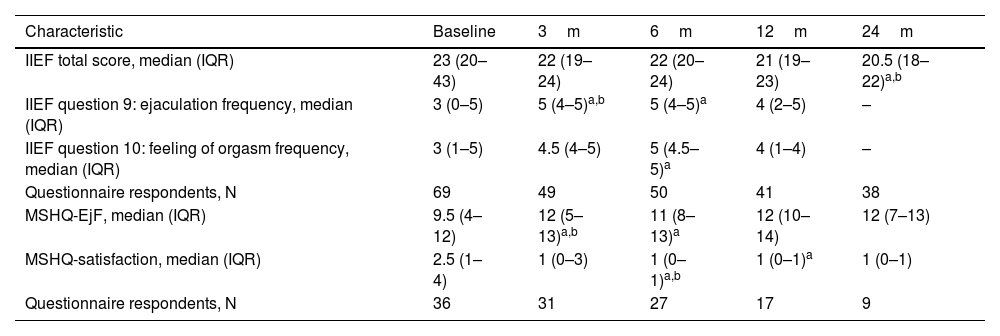
Sexual functionTable 3 shows the evolution of sexual function assessed by the IIEF and/or MHSQ-EjD questionnaires. Although the total IIEF scores show a slight decrease after 12 months of follow-up, the specific questions on ejaculation show an improvement after 3 months, which is sustained over time. In patients evaluated with the MSHQ-EjF questionnaire, a positive evolution was also observed in ejaculation, with higher values from the 3rd month of follow-up, with a peak at 12 months and remaining above baseline values at 24 months.
Sexual function evaluation following water vapor thermal therapy.
| Characteristic | Baseline | 3m | 6m | 12m | 24m |
|---|---|---|---|---|---|
| IIEF total score, median (IQR) | 23 (20–43) | 22 (19–24) | 22 (20–24) | 21 (19–23) | 20.5 (18–22)a,b |
| IIEF question 9: ejaculation frequency, median (IQR) | 3 (0–5) | 5 (4–5)a,b | 5 (4–5)a | 4 (2–5) | – |
| IIEF question 10: feeling of orgasm frequency, median (IQR) | 3 (1–5) | 4.5 (4–5) | 5 (4.5–5)a | 4 (1–4) | – |
| Questionnaire respondents, N | 69 | 49 | 50 | 41 | 38 |
| MSHQ-EjF, median (IQR) | 9.5 (4–12) | 12 (5–13)a,b | 11 (8–13)a | 12 (10–14) | 12 (7–13) |
| MSHQ-satisfaction, median (IQR) | 2.5 (1–4) | 1 (0–3) | 1 (0–1)a,b | 1 (0–1)a | 1 (0–1) |
| Questionnaire respondents, N | 36 | 31 | 27 | 17 | 9 |
IIEF, International Index of Erectile Function Questionnaire; MSHQ-EjD, Male Sexual Health Questionnaire-Ejaculatory Dysfunction; IQR, Interquartile range.
Twenty-four months after treatment, 6 patients (10%) had undergone surgical retreatment, all of them treated by transurethral resection of the prostate, without complications. Medical treatment with α-blockers and I5AR went from 89% and 41% of patients, respectively, to a minimum of 22% and 5% at 6 months and 30% and 8% at 24 months, respectively.
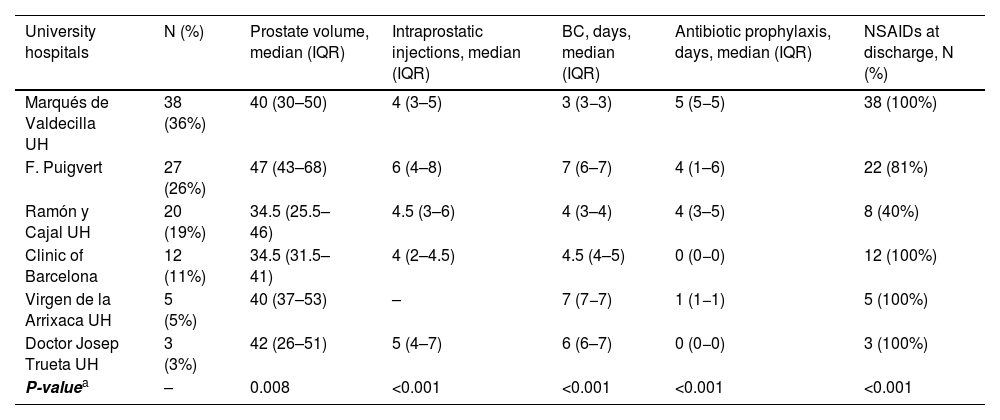
Technical variations among hospitalsInter-hospital variations are shown in Table 4. Catheterization time varied from a median of 3.2 days to a median of 7 days. The median baseline prostate volume ranged from 34.5 to 47g (P=.008). The median number of injections per procedure were between 4 and 6 (P<.001). In 3 of the 6 hospitals, antibiotic prophylaxis was prescribed for a median of 4–5 days; in the remaining 3, no antibiotic prophylaxis was prescribed or was prescribed only for 1 day (P<.001). Except for 1 hospital, all hospitals prescribed nonsteroidal anti-inflammatory drugs (NSAIDs) at discharge in the majority of patients. One hospital performed cystoscopy before each case; the other hospitals did not report this systematic practice.
Inter-hospital variations in surgical and postoperative management.
| University hospitals | N (%) | Prostate volume, median (IQR) | Intraprostatic injections, median (IQR) | BC, days, median (IQR) | Antibiotic prophylaxis, days, median (IQR) | NSAIDs at discharge, N (%) |
|---|---|---|---|---|---|---|
| Marqués de Valdecilla UH | 38 (36%) | 40 (30–50) | 4 (3–5) | 3 (3−3) | 5 (5−5) | 38 (100%) |
| F. Puigvert | 27 (26%) | 47 (43–68) | 6 (4–8) | 7 (6–7) | 4 (1–6) | 22 (81%) |
| Ramón y Cajal UH | 20 (19%) | 34.5 (25.5–46) | 4.5 (3–6) | 4 (3–4) | 4 (3–5) | 8 (40%) |
| Clinic of Barcelona | 12 (11%) | 34.5 (31.5–41) | 4 (2–4.5) | 4.5 (4–5) | 0 (0−0) | 12 (100%) |
| Virgen de la Arrixaca UH | 5 (5%) | 40 (37–53) | – | 7 (7−7) | 1 (1−1) | 5 (100%) |
| Doctor Josep Trueta UH | 3 (3%) | 42 (26–51) | 5 (4–7) | 6 (6–7) | 0 (0−0) | 3 (100%) |
| P-valuea | – | 0.008 | <0.001 | <0.001 | <0.001 | <0.001 |
IQR, Interquartile range; NSAIDs, Non-steroidal anti-inflammatory drugs; BC, Bladder catheter.
Since the first publication on WVTT in 2016, evidence on the efficacy of this technique has been increasing.4 Favorable results have recently been published in Spain.9 Our study differs by only involving public university hospitals, a more restrictive patient selection in terms of prostate volume, excluding patients with bladder catheter at the time of the procedure, and with a longer follow-up time with a larger number of patients during this period. To the best of our knowledge, this is only the second multicenter study with 2 years of follow-up on WVTT.8
The high incidence of treatment for the median lobe in our series (62%) highlights the usefulness of WVTT in these cases without great technical difficulty, in contrast to other minimally invasive treatments.8,10 Although the number of events is too low to draw conclusions, those cases in which the median lobe was identified on previous ultrasound and was not treated at surgery showed a lower-than-average improvement in Qmax at 6 months (3.16 vs. 5.2ml/s). This characteristic was already mentioned by McVary et al. who observed that 70% of the patients in their series who required surgical retreatment had a prostate median lobe that was not initially treated.8
We found no association between catheterization time and incidence of postoperative AUR. The mean initial catheterization time among the 17 patients (16.2%) who presented AUR, and the overall mean catheterization time were similar (5 vs 4.6 days, respectively). Of the 5 hospitals participating in this study, 4 routinely prescribed nonsteroidal anti-inflammatory drugs (NSAIDs) in the postoperative period. In general, the procedure was always performed as day surgery with only 3 of the 105 patients requiring a 1-day hospitalization due to dizziness in 2 cases, and to fever in 1 case.
The different studies published on Rezūm are highly consistent in terms of efficiency values. On the other hand, the variability in rates of one of the complications presented following this technique, AUR after BC withdrawal, is striking. The rates of the studies reviewed vary between 3.7% and 33%.2–7 In an attempt to clarify possible causes, we analyzed the relationship in our series of AUR, with an incidence of 16%, with catheterization time, baseline prostate volume, and the number of intraprostatic injections, without identifying significant differences in these parameters. However, this could be due to the low number of cases present in our series, 17 in total. A notable situation is that of patients who presented AUR in 1 of the hospitals, all had presented AUR before the intervention. However, this association was not observed in the other hospitals.
The mean improvement in IPSS, QoL and Qmax at 12 months (13.1, 2.9, and 4.2ml/s, respectively) is similar to that observed in other studies with follow-up periods between 6 months and 5 years.7
As in other studies, ejaculation is preserved in almost all patients treated with WVTT.7 The improvement in ejaculation observed from baseline in our study is probably due to the combination of this preservation of ejaculation and the cessation of medical treatment for BPH.
The incidence of surgical retreatment at 2 years of follow-up in our series (10%) is higher than that observed by McVary et al., with a surgical retreatment rate at 5 years of 4.4% (although 83% of retreatments were performed in the first 2 years) and that observed by Dixon et al. with a rate of 1.5% at 2 years.4,8 However, in studies with shorter follow-up periods, the retreatment rate is in some cases higher, such as the 2.3% observed by Mollengarden et al. at 6 months follow-up, among others.11–13 We must mention that, in our series, of the 6 cases submitted to surgical retreatment, 4 of them occurred in the first 4 cases performed the same single center. This could raise suspicion of an association with the learning curve or patient selection. It should be mentioned that the absence of complications in retreatment is partly due to one of the advantages of WVTT, which is that it does not hinder subsequent surgery as it does not involve permanent implants.
Reduced treatment with α-blockers and 5ARI was observed at 6 months of therapy, which highlights the progressive nature of functional improvement after WVTT.
Inter-hospital variations were observed mainly in the immediate postoperative treatment and, to a lesser extent, in case selection. Regarding postoperative antibiotic prophylaxis, 50% of the hospitals administered regimens of 4 or more days, and 50% did not include prophylaxis at all or only for 1 day. In 50% of the hospitals, the catheter was left in place for less than 5 days, and 50% for more than 6 days. Regarding prostate volume, number of injections and the NSAID regimen at discharge, 5 of the 6 hospitals presented similar data except for 1 hospital in each case with slightly different data. Although it is not easy to observe significant differences in outcomes with the low number of patients in each center, we believe that the findings of this study may help to optimize protocols between hospitals, thus minimizing unnecessary discomfort and complications and possibly improving procedural outcomes.
The main limitations of this study are the low number of patients in each center, especially considering the technical and follow-up variations among centers, as well as the use of different questionnaires to assess sexual function. Despite being one of the studies with the largest number of patients and the longest follow-up time, only 60 patients had completed the 24-month follow-up at the time of data analysis.
ConclusionsMinimally invasive treatment for BPH with WVTT is effective and has shown good functional outcomes at 24 months of follow-up, without significant impairment of sexual function and a low incidence of complications. There are minor inter-hospital variations, mainly in the immediate postoperative period.
FundingThis research has not received specific support from public sector agencies, commercial sector, or non-profit entities.
Conflict of interestsThe authors declare that they have no conflict of interest.