Cochlear damage is frequent in long-term aminoglycosides therapy or chemotherapeutic treatments with platinum-based agents. Despite its prevalence, it is currently underestimated and underdiagnosed. A monitoring protocol is vital to the early detection of cochleotoxicity and its implementation is widely encouraged in every hospital unit. Our aim was to elaborate a cochleotoxicity monitoring protocol for patients treated with platinum compounds or aminoglycosides antibiotics.
MethodsPubMed® database was searched using terms relevant to drug cochleotoxicity in order to identify the most adequate protocol. Several articles and guidelines influenced our decision.
ResultsThere is no consensus on a universal monitoring protocol. Its formulation and application rely heavily on available resources and personnel. High-frequency audiometry and otoacoustic emissions play an important role on early detection of cochleotoxicity caused by aminoglycoside antibiotics and platinum compounds.
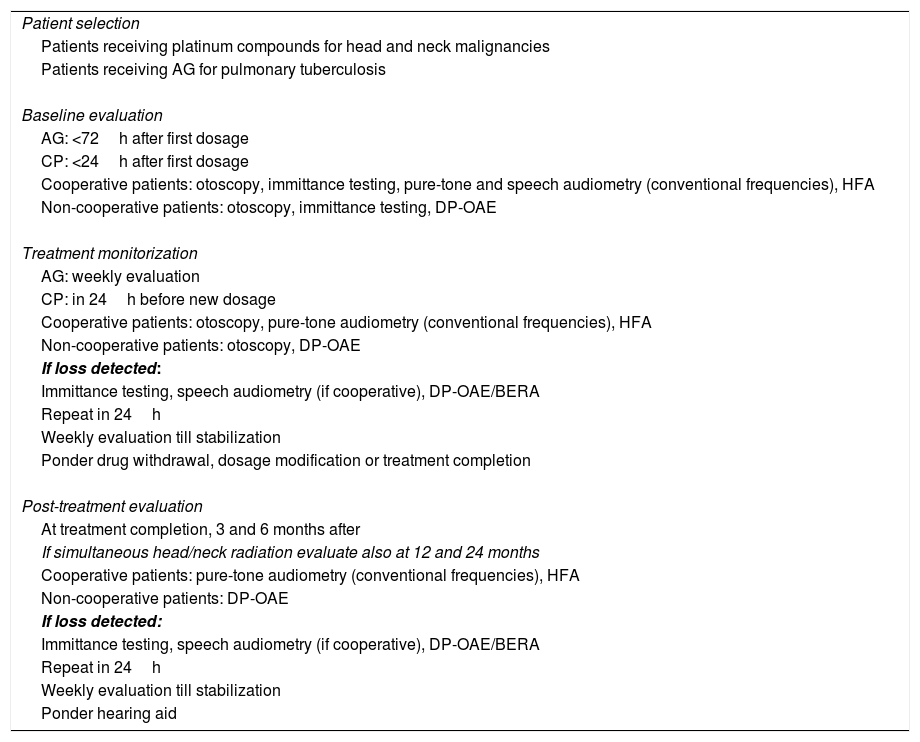
ConclusionA cochleotoxicity monitoring protocol consisting on an initial evaluation, treatment follow-up and post-treatment evaluation is proposed.
El daño coclear es frecuente en la terapia de aminoglucósidos a largo plazo, o en tratamientos quimioterapéuticos con agentes a base de platino. A pesar de su prevalencia, actualmente está subestimado y subdiagnosticado. Un protocolo de monitorización es vital para la detección temprana de la ototoxicidad, por lo que se incita a su implementación en todas las unidades hospitalarias. Nuestro objetivo fue elaborar un protocolo de monitorización de la cocleototoxicidad para pacientes tratados con compuestos de platino o antibióticos aminoglucósidos.
MétodosSe realizaron búsquedas en la base de datos PubMed® utilizando términos relevantes para la cocleototoxicidad de los fármacos con el fin de identificar el protocolo más adecuado. Varios artículos y directrices influyeron en nuestra decisión.
ResultadosNo hay consenso sobre un protocolo de monitoreo universal. Su formulación y aplicación dependen en gran medida de los recursos y el personal disponibles. La audiometría de alta frecuencia y las emisiones otoacústicas desempeñan un papel importante en la detección temprana de la cocleototoxicidad causada por los antibióticos aminoglucósidos y los compuestos de platino.
ConclusiónSe propone un protocolo de monitorización de la cocleototoxicidad, consistente en una evaluación inicial, seguimiento del tratamiento y evaluación postratamiento.