Most mental disorders have its onset during childhood, but less than one third of affected children seek professional help. The aim of this study is to (1) estimate the lifetime prevalence of mood, anxiety, conduct, and eating disorder diagnoses in 18-year-olds in 2017 and (2) the temporal trends of incidence diagnosis rates in 2009–2017 in children aged 2–18 in Catalonia, Spain.
Material and methodsWe used a registry-based cohort including all children aged 2–18 living in Catalonia in 2009–2017, from the Catalan Health Service. Cases were identified with ICD-9 codes. Lifetime prevalence was calculated for 2017, and annual incidence for 2009–2017. Temporal trends were analyzed with multivariate negative binomial regression models.
ResultsLifetime prevalence of diagnoses was highest for conduct disorders (5.05%), followed by anxiety (4.37%), mood (3.07%), and eating disorders (2.11%). Median age of diagnosis was 16 years for mood, anxiety and eating disorders, and 15 years for conduct disorders. Comorbidity was present in 20.74% of those diagnosed with a mental disorder. Annual incidence rates for all disorders increased in 2011–2013/2014, and then stabilized. However, incidence rate of anxiety diagnoses in 13–18-year-old children doubled between 2016 and 2017.
ConclusionsLifetime prevalence of diagnoses are lower than the expected rates of mental disorders based on interview/survey European studies. Further research is needed into the factors underlying (1) the underdiagnoses of mental disorders in children and (2) the increasing trend of anxiety disorder diagnoses in older children.
Mental disorders, such as mood, anxiety, conduct, and eating disorders are considered leading causes of burden of disease among children and adolescents worldwide.1 Recent evidence on worldwide-pooled prevalence estimates that 13–20% of all children have a mental disorder,2,3 but less than one third of affected children seek professional help.4–6 Because most mental disorders emerge in childhood, early detection and intervention is critical to reduce the burden of disease, as well as to prevent chronic trajectories of mental disorders and negative consequences on physical health and social functioning.7 Epidemiological studies on the prevalence and incidence of mental disorders in children can be divided into (1) registry-based studies that estimate the number of children that have been diagnosed with a mental disorder by a healthcare professional, and (2) interview and/or survey-based studies that estimate how many children within a population fulfill the criteria of a mental disorder, named case-level mental disorders. Studies on case-level mental disorders in children estimate a lifetime prevalence of 6.2–14.4% for mood disorders,8–12 9.9–32.4% for anxiety disorders,8,10–13 9.0–19.1% for conduct disorders,8,11 and 3.5–6.1% for eating disorders.12,14,15 To our knowledge, little evidence is available on the lifetime prevalence of mental disorders among children in Catalonia, although various studies do report on the point prevalence. These studies estimate a prevalence of 2.2–4.1% for mood disorders,16–18 6.6–36.1% for any anxiety disorder,16–18 1.4% for conduct disorders,17 and 1.4% for eating disorders.16,18 However, these studies should be interpreted with caution as some of them were conducted in specific age groups, such as preschoolers, or in specific populations, such as in a Spanish Slum.
Overall, registry-based studies do estimate lower lifetime prevalence of diagnoses than interview/survey based studies.19 In order to implement effective policies aimed at reducing the burden of disease in mental disorders, knowledge is needed on how the number and distribution of mental disorder diagnoses in children compare to the expected number of case-level disorders based on interview/survey-studies. Increasing knowledge on the prevalence of mental disorders in children is available, but evidence on the lifetime prevalence of diagnoses from a large registry-cohort is lacking in Southern-European countries, such as Spain. Additionally, to our knowledge, no recent studies that provide insights into the long-term temporal trends of incidence of diagnoses are currently available, with the exception of two recent studies published on the incidence of Autism Spectrum Disorder20 and Attention Deficit Hyperactivity Disorder21 among children in Catalonia.
Therefore, this study aims to estimate the lifetime prevalence of diagnoses of mood, anxiety, conduct, and eating disorders in children aged 18 in 2017 in a national health registry of Catalonia, Spain. In addition, it aims to estimate the temporal trends of the incidence of diagnoses of mood, anxiety, conduct, and eating disorders between 2009 and 2017 in children aged 2–18 in Catalonia. We selected these four disorders as they are generally considered the most prevalent mental disorders across childhood, together with Autism Spectrum Disorder and Attention Deficit Hyperactivity Disorders, of which recent evidence on the prevalence and incidence in Catalonia is already available.20,21
Material and methodsStudy design and populationWe used a registry-based cohort study including all children aged 2–18 living in Catalonia for each year between 2009 and 2017. Data was retrieved from (1) the Basic Minimum Set of Data, which registers all diagnoses from the public healthcare facilities in Catalonia, and (2) the Central Registry of Insured Persons, which includes information of all children insured under the Catalan Health Service. The state-funded Spanish National Health System provides access to healthcare services for all children in Spain.22 Because the number of children living in the ‘Vall d’Aran’ healthcare area was too small to ensure anonymization of the data, all data from this healthcare area was excluded (n=1445, 0.11% of the total population of children aged 2–18 in 2017). This study was reviewed and approved by the Clinical Research Ethics Committee of the Parc de Salut Mar.
Definitions of casesData from all children that are diagnosed in public healthcare facilities under the Catalan Health Service is collected in the Basic Minimum Set of Data. This registry includes information on diagnoses from primary care centers, mental health centers, mental health outpatient clinics, and hospital discharges. These centers started registering in different years, for example in 2006 for the hospital discharges and in 1990 for the primary care center cases. The mental health outpatient clinics and the mental health centers started registering in 2008. As we found an artifact of a high number of cases in 2008, the first year that all centers registered in the Basic Minimum Set of Data, we started including cases from 2009 onwards. Clinicians used DSM IV, DSM 5, ICD-9, and ICD-10 criteria to identify mental disorders in children during the time period of our study, but all diagnoses were codified administratively with ICD-9 codes. All children aged 2–18 between 2009 and 2017 that were diagnosed with one of the corresponding ICD-9 codes listed in Table S1 were defined as a mood disorder case, an anxiety disorder case, a conduct disorder case, and/or an eating disorder case. A comorbidity case was defined as a diagnosis of at least two of the disorder groups. Children under the age of 2 were not included, as mental disorders are hardly identified at such a young age, and different classification systems are used.17 In the registry, some cases were duplicated due to registration in different public healthcare centers or by different healthcare professionals. For our study, we selected the first entry in the registry as the first diagnosis of the disorder. For each case, time of diagnosis, sex, age, and healthcare area were collected. Time of diagnosis was defined as the year in which the child was first registered with each specific mental disorder group. Age at diagnosis was collected as a discrete variable, as well as divided into the following categories: 2–6 years, 7–12 years, and 13–18 years. The division into age groups was based on the Spanish school system, as we hypothesized school environment might influence recognition and diagnosis of mental disorders. The 28 healthcare areas (excluding ‘Vall d’Aran’) within the Catalan territory, are determined by socio-economic, demographic, and geographic factors.
Population-based denominatorsTwo population-based denominators were estimated based on data from the Central Registry of Insured Persons: the total population and the total population at risk. The total population was defined as the total number of children aged 18, insured under the Catalan Health Service and living in Catalonia in the year 2017, which was used for the calculation of lifetime prevalence at age 18. The total population at risk, used for the calculation of incidence, was defined as the number of children aged 2–18 that were disorder diagnosis-free for each year between 2009 and 2017 and for each disorder group separately. For both population-based denominators, the population on 1st January of the following year was used. The population-based denominators were stratified by sex, age, and healthcare area using the same categories as those applied for the cases.
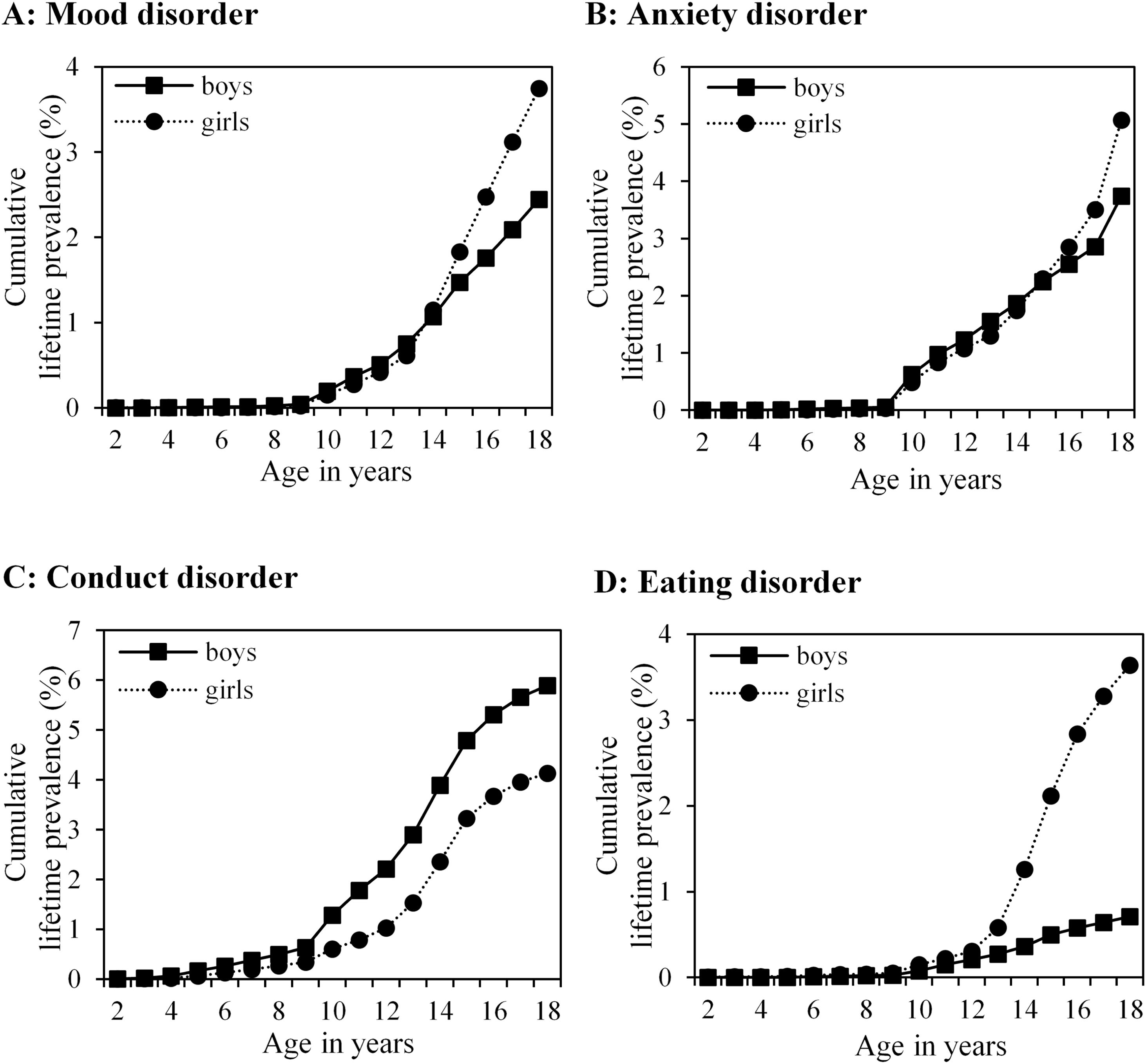
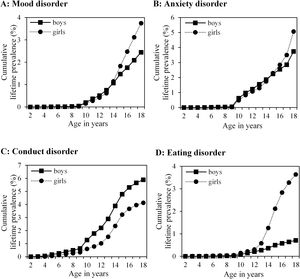
Statistical analysisLifetime prevalence is the proportion of a population that has been diagnosed with a disease at some point in their life up to the time of assessment. Lifetime prevalence of each disorder diagnosis group was calculated overall and stratified by sex. Differences in lifetime prevalence between sex were assessed using univariate logistic regression models, and odds ratios (OR) and confidence intervals (CI) were estimated. Median age of diagnosis of each of the disorder groups was calculated. Cumulative lifetime prevalence of diagnoses between age 2 and age 18 was plotted for children aged 18 in 2017, stratified by sex, using the available data on age at diagnosis for the group of 18-year-olds in 2017. Lifetime prevalence of comorbidity was calculated and stratified by sex and disorder groups.
Annual incidence is the amount of newly identified cases of disease per population at risk in one year. The annual incidence rates were calculated for each of the disorder groups and each of the years between 2009 and 2017 separately. Incidence was stratified by sex and age groups (2–6 years, 7–12 years, and 13–18 years) based on the child's age at time of diagnosis. After visual inspection, we encountered different increasing, decreasing, and stabilizing trends between 2009 and 2017 for each disorder group. We defined these time periods specifically for each disorder group, and we run separate multivariate negative binomial regression models for each of the increasing, decreasing, and stabilizing parts in the temporal trends for each of the disorder groups. All models were adjusted for sex, age groups, and healthcare areas. Models were stratified by sex and age groups when a significant interaction term between sex and year and/or age groups and year was identified.
Data analysis was performed using STATA (version 13.0; Stata Corporation, College Station, Texas, USA) and Open Epi (version 3.01; Dean AG, Sullivan KM, Soe MM).
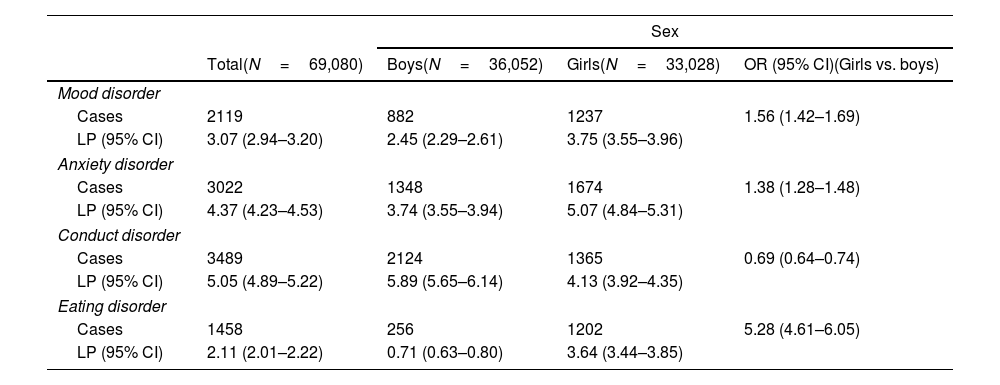
ResultsLifetime prevalence of diagnosesThe highest lifetime prevalence of diagnoses was found for conduct disorders (5.05%), followed by anxiety disorders (4.37%), mood disorders (3.07%), and eating disorders (2.11%) (Table 1). Girls had over 5 times higher odds (OR 5.28 (95% CI 4.61–6.05)) of an eating disorder compared to boys, in addition to having moderately higher odds of a mood disorder (OR 1.56 (95% CI 1.42–1.69)) and an anxiety disorder (OR 1.38 (95% CI 1.28–1.48)), and moderately lower odds of a conduct disorder diagnosis (OR 0.69 (95% CI 0.64–0.74)).
Lifetime prevalence (%) of diagnoses of mood disorder, anxiety disorder, conduct disorder, and eating disorder in children aged 18 in Catalonia in 2017.
| Sex | ||||
|---|---|---|---|---|
| Total(N=69,080) | Boys(N=36,052) | Girls(N=33,028) | OR (95% CI)(Girls vs. boys) | |
| Mood disorder | ||||
| Cases | 2119 | 882 | 1237 | 1.56 (1.42–1.69) |
| LP (95% CI) | 3.07 (2.94–3.20) | 2.45 (2.29–2.61) | 3.75 (3.55–3.96) | |
| Anxiety disorder | ||||
| Cases | 3022 | 1348 | 1674 | 1.38 (1.28–1.48) |
| LP (95% CI) | 4.37 (4.23–4.53) | 3.74 (3.55–3.94) | 5.07 (4.84–5.31) | |
| Conduct disorder | ||||
| Cases | 3489 | 2124 | 1365 | 0.69 (0.64–0.74) |
| LP (95% CI) | 5.05 (4.89–5.22) | 5.89 (5.65–6.14) | 4.13 (3.92–4.35) | |
| Eating disorder | ||||
| Cases | 1458 | 256 | 1202 | 5.28 (4.61–6.05) |
| LP (95% CI) | 2.11 (2.01–2.22) | 0.71 (0.63–0.80) | 3.64 (3.44–3.85) | |
CI: confidence interval; LP: lifetime prevalence; N: number of children; OR: odds ratio.
Median age of diagnosis was 16 years for mood, anxiety, and eating disorders, and 15 years for conduct disorders. This was similar for both sexes. A comparable pattern in cumulative lifetime prevalence per age was seen for mood and anxiety disorders (Fig. 1). Both had low cumulative lifetime prevalence until the age of 9, followed by an increase of diagnoses for both boys and girls. After the age of 14 and 15, girls were diagnosed more frequently with mood and anxiety disorders, respectively. In conduct disorders, new diagnoses were generally given from an earlier age (i.e. 5 years old), but the amount of new diagnoses did increase after the age of 9. In all ages, boys had a higher lifetime prevalence compared to girls. Similar to mood and anxiety disorders, new diagnoses of eating disorders were typically given after the age of 9. In addition, for girls there was a larger increase in new diagnoses from the age of 12 onwards, while the amount of new diagnoses in boys increased only slightly.
Lifetime prevalence of comorbidity was present in 20.74% (17.43% in boys and 23.81% in girls) of the 18-year-old population of children with at least one mental disorder diagnosis in 2017. Mood and anxiety disorders were the most frequent comorbid disorder diagnoses (43.14% of all comorbidities), followed by anxiety and conduct disorders (16.80%) and mood and conduct disorders (16.21%).
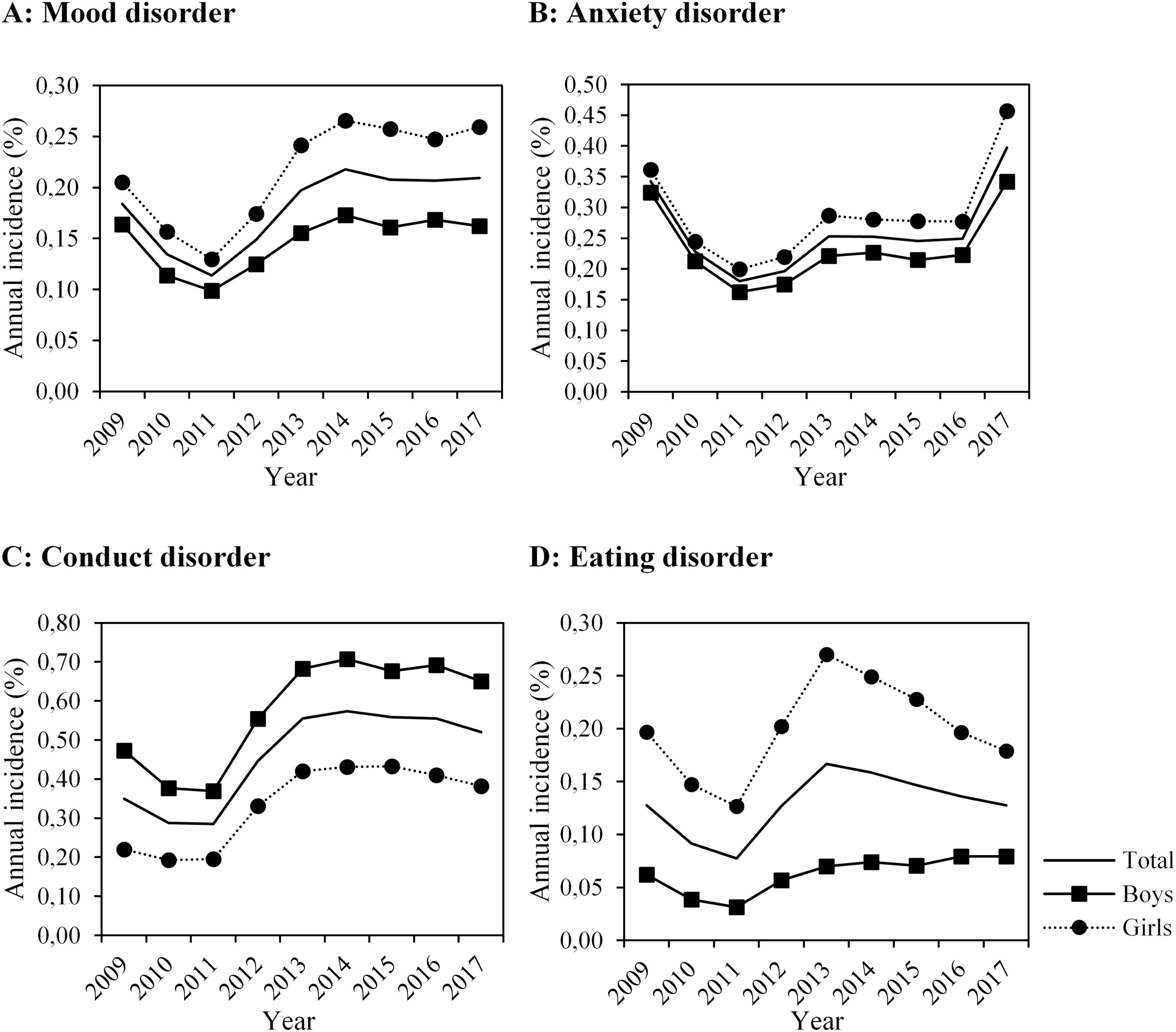
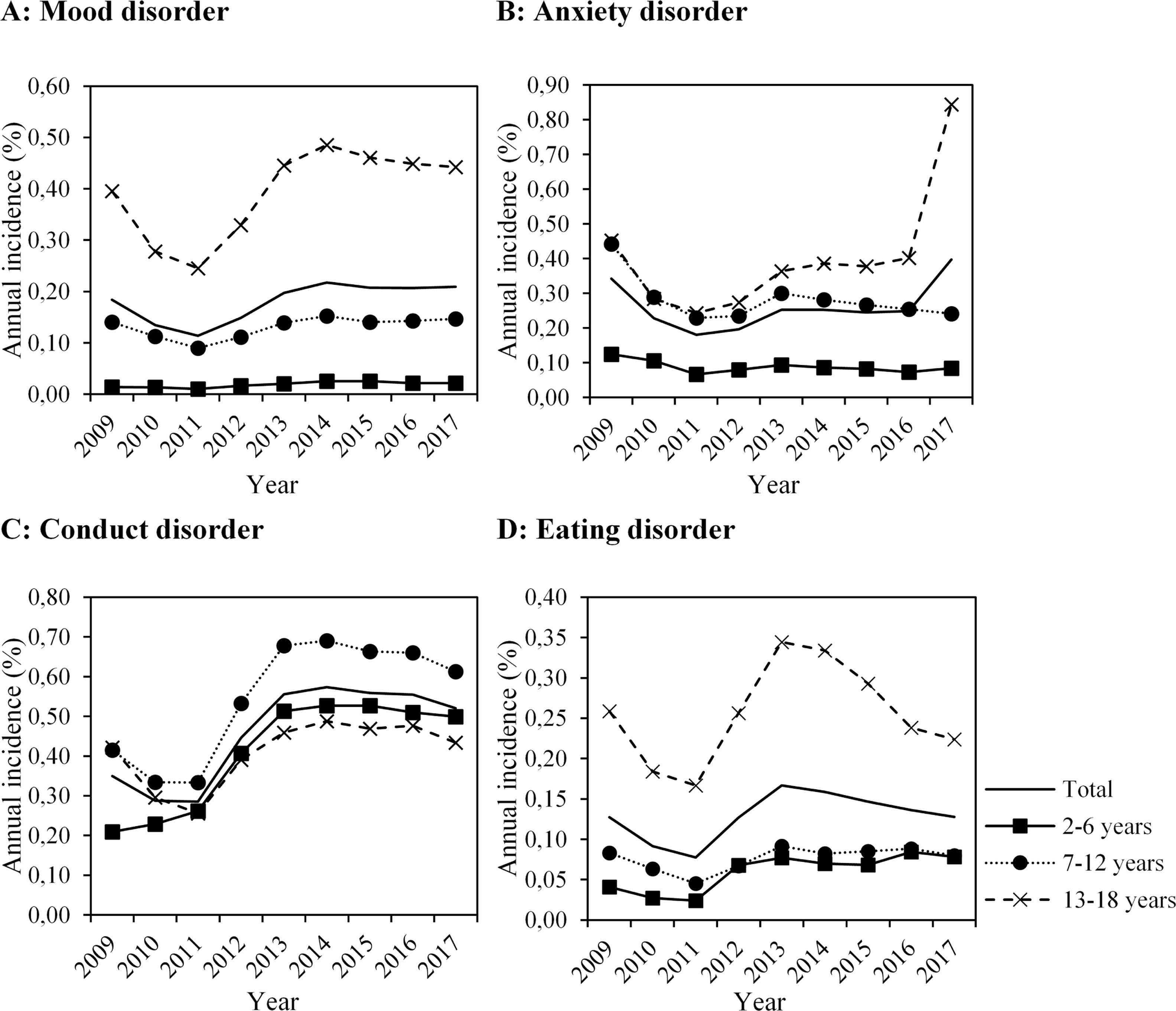
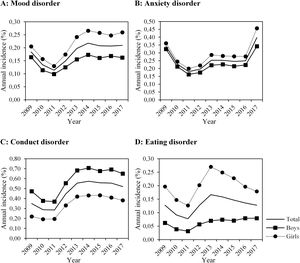
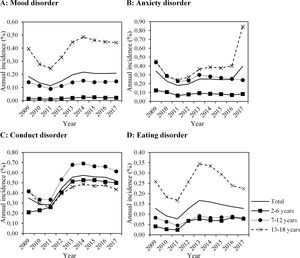
Temporal trends in incidence of diagnosesFor mood disorder diagnoses, in 2009–2011 the incidence rate annually decreased on average 28% (IRR 0.78 (95% CI 0.74–0.82)), in 2011–2014 it annually increased 24% (IRR 1.24 (95% CI 1.20–1.28)), and after 2014 it stabilized (IRR 0.98 (95% CI 0.95–1.00)) (Fig. 2, Tables S2–S4). In 2009–2012 the incidence rate of anxiety disorder diagnoses annually decreased on average 43% (IRR 0.70 (95% CI 0.67–0.73)), in 2011–2013 it annually increased 20% (IRR 1.20 (95% CI 1.15–1.25)), and in 2013–2016 it stabilized (IRR 0.99 (95% CI 0.97–1.02). In the period between 2016 and 2017 there was a second increase of diagnoses of anxiety disorder of 36% (IRR 1.36 (95% CI 1.23–1.51)). In 2009–2011 the incidence of conduct disorder diagnoses annually decreased 9% (IRR 0.92 (95% CI 0.89–0.96)), in 2011–2014 it annually increased 26% (IRR 1.26 (95% CI 1.23–1.28)), and after 2014 it stabilized (IRR 0.98 (95% CI 0.96–1.00). In 2009–2011 the incidence of eating disorder diagnoses annually decreased on average 30% (IRR 0.77 (95% CI 0.71–0.83)), in 2011–2013 it annually increased 51% (IRR 1.51 (95% CI 1.40–1.63)), and after 2014 it stabilized (IRR 0.98 (95% CI 0.95–1.01)).
Temporal trends were largely comparable for both sexes and age groups in all disorder groups, with the exception of anxiety disorders (Figs. 2-3, Table S3). Incidence of anxiety disorder diagnoses in 2016–2017 doubled (IRR 2.04 (95% CI 1.86–2.25)) in the age group 13–18 years for both sexes.
DiscussionThis study provides new insights into the lifetime prevalence of the diagnosis of common mental disorders in a large registry-based cohort of Southern-European children. Of all 18-year-old children, 3.1% had ever been diagnosed with a mood disorder, 4.4% with an anxiety disorder, 5.1% with a conduct disorder, and 2.1% with an eating disorder. Girls had higher odds of a mood disorder, anxiety disorder, and eating disorder, but lower odds of a conduct disorder diagnosis. Median age-of-diagnosis was 16 years for mood, anxiety and eating disorders, and 15 years for conduct disorders. Comorbidity was present in 20.74% of the cases. The most prevalent comorbidity was mood disorder with anxiety disorder. For all diagnosis groups we observed a decrease of the incidence rates in 2009–2011, an increase in 2011–2013/2014, and then a stabilization. However, incidence of anxiety disorder diagnoses in older children doubled between 2016 and 2017.
Steinhausen and Jakobsen (2019) reported cumulative incidences in a Danish-registry based cohort of 18-year-olds of 1.84% for mood disorders, 0.84% for anxiety disorders, 1.32% for conduct disorders and 0.85% for eating disorders.23 These estimates are consistently lower than our findings. Gyllenberg et al. (2014) reported a lifetime prevalence of specialized service use in 14-year-old Finish children of 1.4% for mood disorders, 2.2% for anxiety disorders, 1.7% for conduct disorders, and 0.4% for eating disorders.19 Compared to the cumulative lifetime prevalence of our study population at age 14 (data not shown), our estimates are slightly lower for mood and anxiety disorders (1.11% and 1.81%, respectively), and higher for conduct and eating disorders (3.16% and 0.79%, respectively). However, this study only included diagnoses in specialized mental health services, while our study also included primary healthcare services which report information of children diagnosed outside the public mental healthcare facilities under the Catalan Health Service. Furthermore, variation in how and by whom cases were registered might underlie the differences found in our study compared to previous studies, as is also suggested by geographical variability in lifetime prevalence in our study (supplementary Fig. 1).
Lifetime prevalence of diagnoses found in our study was consistently lower than lifetime prevalence of case-level disorders reported in survey- and interview-based studies.8–15 This difference might be explained by (1) an overestimation of case-level mental disorders in survey/interview-based studies, mainly of cases with low impairment, (2) missed cases in our study due to treatment in specialized private centers, and (3) low help-seeking behavior in children with mental disorders by themselves or their primary caretakers.4,5,11,24,25 Emerging evidence suggests that a variety of factors underlie an underutilization of services, including little parental knowledge about the availability and accessibility of services, poor recognition of child's mental disorders within their community, and the stigmatization of mental health problems.26 Furthermore, service utilization may depend on the type of disorder, the degree of family-related stress, and socioeconomic determinants.27
These findings highlight the need for the improvement of both detection of mental disorders and access to mental health services for children. Our findings on differences between boys and girls in lifetime prevalence are consistent with both registry-based studies and studies on lifetime prevalence of case-level disorders.8,10,11,16,28 Contrary to our findings, a large cohort-study in the United States reported lower median age of onsets for case-level mood disorders (13 years), anxiety disorders (6 years), and conduct disorders (11 years).11 The percentage of comorbidity cases found in our study could not be directly compared to previous studies, as none of these studies included the exact same disorder groups in their analysis. However, our data does support the high comorbidity between mood and anxiety disorders, and to a lesser extent between conduct disorders and mood and anxiety disorders found in previous clinical and community studies, including in the context of Catalonia.16,17,29–31 In our study, the lifetime prevalence of conduct disorders was relatively high compared to the other disorders. Also, comorbidity with conduct disorders was frequent. This might suggest that the diagnosis of conduct disorder ‘masks’ the diagnosis of another mental disorder, e.g. a child with a depressive disorder might present first with behavioral problems which leads to a diagnosis of conduct disorder instead of a depressive disorder. Osa et al., for example found that subclinical Oppositional Defiant Disorder was highly comorbid with other disorders such as anxiety disorders in a community sample of preschool children in Catalonia.32 Moreover, it might be interesting to further research commonly shared symptoms among children with comorbid disorders, as Ezpeleta et al. indicated that irritability was often a shared symptom in children with both internalizing and externalizing problems in a community sample in Catalonia.33
The results of our study add new knowledge to recent trends of mental disorder diagnoses in children. Previous studies suggest that the incidence of mental disorders in children had been increasing until the beginning of the 21st century, and is now moving toward a plateau phase globally.34,35 One explanatory factor for the trends found in our study, might be the financial crisis in Spain which lasted from 2008 to 2014. Yet, previous studies that have researched the effect of the financial crisis in Spain only found a significant worsening in mental health among children at risk of eviction, but not among children in the general population.36,37 However, we cannot directly compare these studies with our results, as in our study we analyzed the yearly temporal progression of mental disorder diagnoses, opposed to performing a pre/post-financial crisis study. Interestingly, previous studies conducted on the temporal trends of the incidence of Autism Spectrum Disorder and Attention Deficit Hyperactivity Disorder in Catalonia using the same registry, did not show comparable patterns in time.20,21 This might suggest that incidence of the diagnosis of the four disorder groups we have researched respond differently to social changes compared to Autism Spectrum Disorder and Attention Deficit Hyperactivity Disorder. The twofold increase between 2016 and 2017 in anxiety disorder diagnoses in older children alone could not sufficiently be explained by existing literature. In the absence of major social events during this period that might cause such a rise in actual anxiety disorder cases, this increase might be partly caused by changes in registration or randomness in the data that we were not aware of. More research is thus needed to see whether this trend remains consistent in the following years, and what its underlying causes might be, before conclusions might be drawn.
One of the main strengths of our study is the design. We used a registry-based cohort that included all children aged 2–18 within the region of Catalonia and contained information from four different public health centers, over a long time period. Furthermore, a uniform reporting system was used in Catalonia in all years between 2009 and 2017, which increased the accuracy of comparison over time. The findings of our study should be interpreted in the context of several limitations. First, due to the organizational nature of the Basic Minimum Set of Data, no data was available on private healthcare facilities and the Child Development and Early Care Centers. The findings of this study thus focus on how many cases of mental disorders are detected by the Spanish public health care system. Although Spain has a national health insurance scheme in which all children are included, and we expect the majority of children with a mental disorder to have attended one of the included public healthcare facilities at least once before they reached the age of 18, it is likely that we missed some cases, especially in regions with a higher socioeconomic status where use of private healthcare is more frequent.38,39 Furthermore, age of diagnosis might not have been accurately registered for all cases, especially those in preschool children. Second, study design masked variation in diagnostic practices. Although all cases were administrated with ICD-9 codes, diagnostic practices might have differed between different facilities or even between healthcare professionals. Unfortunately we were not able to report on diagnostic practices used to report mental disorders in this study. Third, we only included first time episodes of each mental disorder, because we could not differentiate between a duplicate (i.e. the same mental disorder episode diagnosed by two different professionals) and a relapse episode. This potentially caused an underestimation of the incidence of diagnoses, especially in older ages. Fourth, the large variation in incidence over time might be related to underlying factors that were beyond the scope of our study, but we cannot exclude that this might also be due to a low coverage and quality of the Basic Minimum Set of Data as a measurement of mental disorder cases in Catalonia. Fifth, undocumented migrants are only covered by national health insurance if they fulfill strict requirements (e.g. a minimum of three-months residence to access public healthcare), and might experience additional barriers for accessing mental health services, related to fear of prosecution and cultural background.40 Although it is difficult to estimate the number of undocumented migrant children in Catalonia during the period of our study, this potentially led to an underestimation of cases in our results. Sixth, although we had information available on the geographical variability of mental disorder diagnoses (supplementary Fig. 1), we were not able to look at potential other factors that might explain variability, such as socioeconomic status. This might be interesting to research in further studies. Last, a small proportion of our 18-year-old study population might not have continuously lived in Catalonia since they were 2 years old, but this information was not available. Children would have been registered with either a local pediatrician (up to 14 years) or a general practitioner (above 14 years) as soon as they had moved to Catalonia, during which their previous medical history would have been documented.
ConclusionAccording to the registers of the Catalan Health Service, diagnoses of conduct disorders were the most prevalent in 18-year-olds in Catalonia, followed by anxiety, mood, and eating disorders. Our study showed both decreasing and increasing temporal trends in the incidence rates in the last 10 years, which were similar for all disorder groups. However, incidence rates of anxiety disorder diagnoses in older children doubled between 2016 and 2017. The results from our study can inform and guide the development of health policies, including the direction of resources toward both adequate diagnosis and prevention measures of mental health disorders in children. More research is needed into the factors underlying (1) the possible underdiagnosis of mental disorders in children and (2) the recent increasing trends of anxiety disorder diagnoses in older children.
Ethical standardsThis study was reviewed and approved by the Clinical Research Ethics Committee of the Parc de Salut Mar, which waived the need to obtain informed consent, because authors only had access to anonymized data through registries. No contact with study subjects was involved in this study. Adequate measures to ensure personal data protection and confidentiality were taken according to the Regulation (EU) 2016/679 on the protection of natural persons with regard to the processing of personal data and on the free movement of such data, and the Spanish Law of Personal Data Protection and Digital Rights Guarantee (3/2018, of 5th December). National regulations on personal data protection were implemented to guarantee the highest standards in personal data management.
Conflict of interestNone.
We would like to express our gratitude toward Joan Albert d’Escofet from the Agency for Health Quality and Assessment of the Catalan Health Department, for providing us with the data needed for this study. Mònica Guxens is funded by a Miguel Servet fellowship (CPII18/00018) from the Spanish Institute of Health Carlos III and Laura Pérez-Crespo by the Health Effects Institute (Assistance Award No. R-82811201). We also acknowledge support from the Spanish Ministry of Science and Innovation and the State Research Agency through the “Centro de Excelencia Severo Ochoa 2019–2023” Program (CEX2018-000806-S), and support from the Generalitat de Catalunya through the CERCA Program.