Increased mental health problems have been reported in children and adolescents related to the COVID-19 lockdown and its immediate aftermath, especially among adolescent females. However, the longer-term impact of persistent quarantine measures and social restrictions on this population is yet to be further explored.
Materials and methodsWe compared the number of children/adolescents admissions to the psychiatric emergency department (ED) of Hospital Clínic de Barcelona during the COVID-19 lockdown and the following year with the numbers of admissions the year before lockdown, adjusting for variations in the population. We also conducted separate analyses by gender, age group, and diagnostic categories. Finally, we also repeated the analyses considering the cumulated deficit/excess since the start of the lockdown. Statistical significance was estimated using binomial tests with Bonferroni correction.
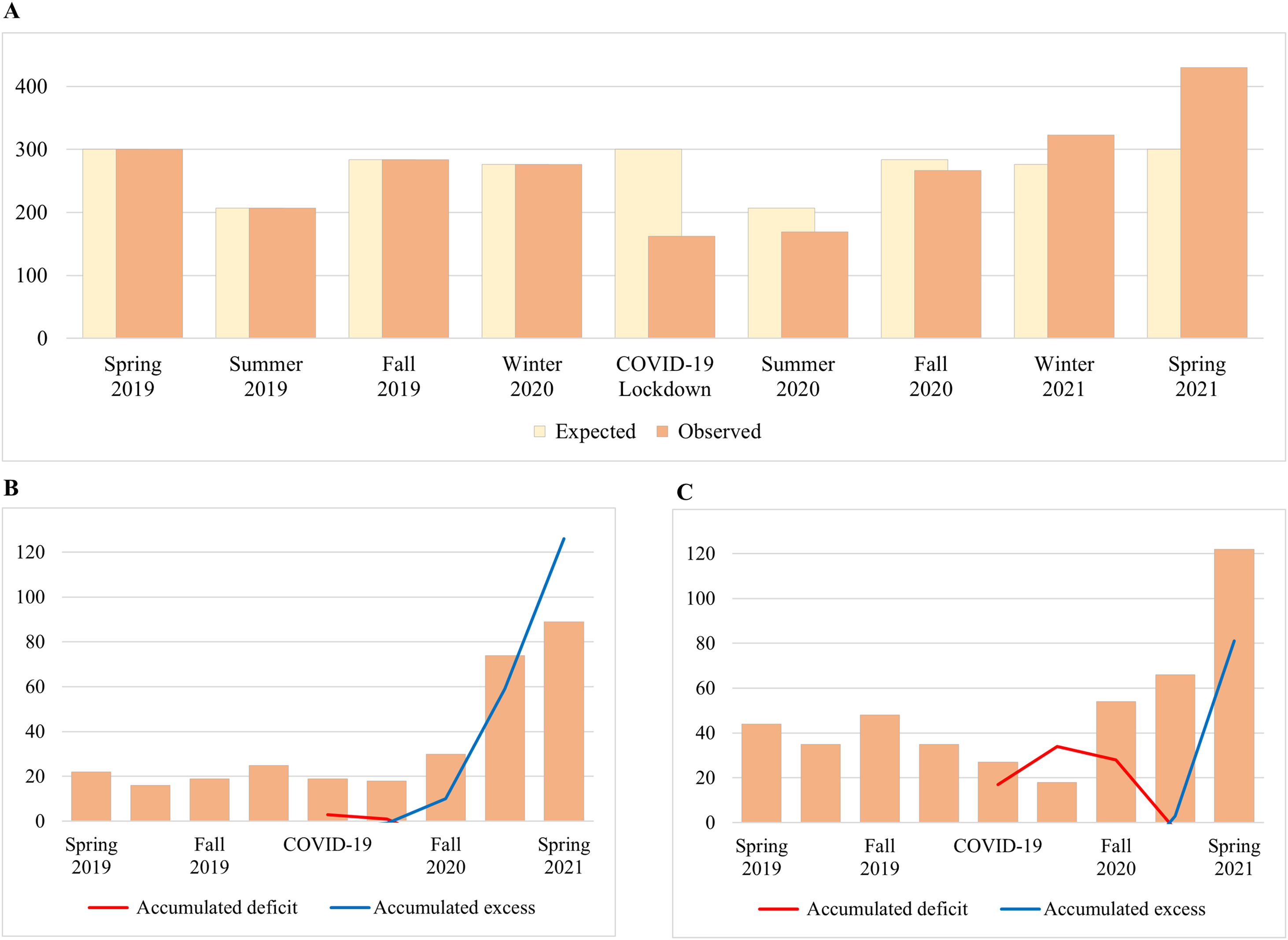
ResultsA total of 2425 admissions were recorded. Globally, admission rates decreased during the lockdown (46%) and progressively increased during the one-year aftermath (43% by spring 2021). This increase was particularly high in adolescent females (85%) while unclear in children and/or males. The main diagnostic categories involved were anxiety, depressive, and eating disorders, as well as self-harm behavior, suicidal ideation, and suicide attempts. The increase in eating disorders, self-harm behavior, and suicide attempts admissions in female adolescents remained statistically significant when considering the cumulated deficit/excess.
ConclusionsWe found increased ED admissions during the aftermath of the COVID-19 lockdown among adolescent females. We recommend strengthening the attention to this population to provide adequate specialized care and prevention strategies.
The COVID-19 pandemic has caused enormous disruptions in the lives of children and adolescents. In Spain – one of the European countries more deeply affected by the pandemic – the national lockdown was declared on March 14th, 2020, and lasted until June 21st, 2020. This lockdown significantly changed the daily routines of the youth, including the abrupt closure of schools and subsequent homeschooling, reduced social interactions, or limited access to health services. Some of these restrictions have continued to take place after lifting the lockdown, and have changed accordingly to new waves and variants.
The impact of the COVID-19 pandemic on the mental health of younger individuals has been well reported,1 being childhood and adolescence vulnerable periods for the development of psychiatric disorders.2 Specifically, most phobias, several types of anxiety disorder, autism and attention-deficit/hyperactive disorders had a median age of onset within 14 years old. In addition, another large group of mental disorder including eating disorder and cannabis use disorders, use to emerge during the transitional period across adolescence and young adulthood.2 During COVID-19 lockdown, increases in depressive symptoms and anxiety were found in this population, and particularly among adolescent females.3 Monitoring visits to the psychiatric Emergency Department (ED) may provide useful information on trends in mental health disorders in the context of the COVID-19.4 Evidence suggests increases in the number of suicide-related admissions,5–7 and mental health-related visits for eating disorders, depression, and other conditions, compared to 2019.8–11 However, it is unclear whether this excess is only due to patients who could not access the mental health facilities during the lockdown or indicates genuine upward trends.
In this study, we aim to compare the admissions of children and adolescents to the psychiatric one year before and after the COVID-19 lockdown, and to study the accumulated deficit/excess during and after the lockdown. We hypothesize that the number of admissions will increase after the lockdown in comparison with the previous year, and that sensitivity analyses will show an excess of ED admissions, especially in adolescent females.
Materials and methodsWe undertook a retrospective, observational study, which consisted of a chart review of children and adolescents admitted to the psychiatric ED of Hospital Clínic de Barcelona, from March 14th, 2019 to June 21st, 2021. The study was approved by the local clinical research ethical committee, and was carried out in accordance with the latest version of the Declaration of Helsinki (2013).
Participants and variablesChildren and adolescents up to 17 years old admitted to the psychiatric ED during the observation period were included in the analysis. Individuals had been evaluated and diagnosed by psychiatrists on duty at the time of admission to the ED according to the ICD-10. Socio-demographic and clinical variables were recorded from clinical charts. Records were review by authorized clinicians to check the accuracy of the data and then anonymized for analysis.
Statistical analysisWe used R-version 4.1.2 (R Core Team, 2020) to investigate changes in the number of children and adolescents psychiatric ED admissions during the COVID-19 lockdown and its aftermath. Specifically, we compared the number of admissions during the spring 2020 compared to the spring 2019, and during its aftermath compared to the corresponding seasons in the year before the lockdown. We used two-tailed binomial tests to assess the statistical significance (set at P<.05 after adjusting by Bonferroni correction for multiple comparisons). We also conducted this analysis for specific age/gender groups (defining adolescents as ≥12 years8) and diagnostic labels. To correct for variations in the population, we adjusted the raw numbers of admissions for the total population of children/adolescents in the areas covered by the psychiatric ED. We retrieved the demographic distribution of the pediatric population from the Catalunya statistics institute (https://www.idescat.cat/). We also adjusted the raw numbers of admissions for the number of days of each season (see Table S1).
Sensitivity analysesWe acknowledged the possibility that some patients could not access the ED during the lockdown and thus visited it later, leading to a “compensatory” excess of admissions during the aftermath. To account for this possibility, we also analyzed the cumulative excess/deficit of admissions since the start of the lockdown.
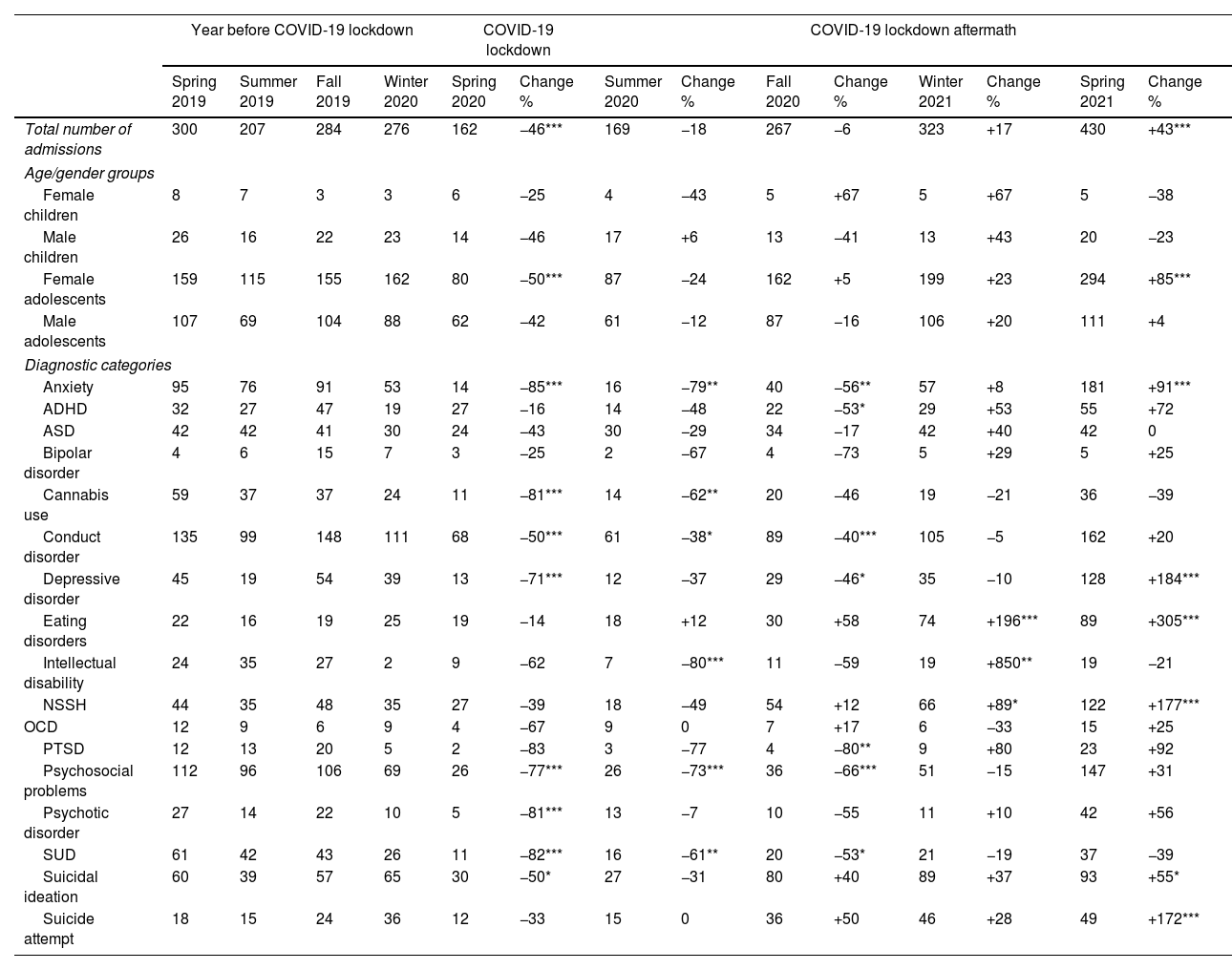
ResultsA total of 2425 admissions to the psychiatric ED were recorded, corresponding to 1419 youth. In addition, 25 admissions were excluded because patients left the ED before being attended. The mean age (SD) of the whole sample was 14.5 (2.2) years old and 60.7% were female participants. Clinical characteristics of the sample across seasons and years can be found in Table 1.
Changes in the number of admissions to the Pediatric Psychiatric Emergency Department.
| Year before COVID-19 lockdown | COVID-19 lockdown | COVID-19 lockdown aftermath | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Spring 2019 | Summer 2019 | Fall 2019 | Winter 2020 | Spring 2020 | Change % | Summer 2020 | Change % | Fall 2020 | Change % | Winter 2021 | Change % | Spring 2021 | Change % | |
| Total number of admissions | 300 | 207 | 284 | 276 | 162 | −46*** | 169 | −18 | 267 | −6 | 323 | +17 | 430 | +43*** |
| Age/gender groups | ||||||||||||||
| Female children | 8 | 7 | 3 | 3 | 6 | −25 | 4 | −43 | 5 | +67 | 5 | +67 | 5 | −38 |
| Male children | 26 | 16 | 22 | 23 | 14 | −46 | 17 | +6 | 13 | −41 | 13 | +43 | 20 | −23 |
| Female adolescents | 159 | 115 | 155 | 162 | 80 | −50*** | 87 | −24 | 162 | +5 | 199 | +23 | 294 | +85*** |
| Male adolescents | 107 | 69 | 104 | 88 | 62 | −42 | 61 | −12 | 87 | −16 | 106 | +20 | 111 | +4 |
| Diagnostic categories | ||||||||||||||
| Anxiety | 95 | 76 | 91 | 53 | 14 | −85*** | 16 | −79** | 40 | −56** | 57 | +8 | 181 | +91*** |
| ADHD | 32 | 27 | 47 | 19 | 27 | −16 | 14 | −48 | 22 | −53* | 29 | +53 | 55 | +72 |
| ASD | 42 | 42 | 41 | 30 | 24 | −43 | 30 | −29 | 34 | −17 | 42 | +40 | 42 | 0 |
| Bipolar disorder | 4 | 6 | 15 | 7 | 3 | −25 | 2 | −67 | 4 | −73 | 5 | +29 | 5 | +25 |
| Cannabis use | 59 | 37 | 37 | 24 | 11 | −81*** | 14 | −62** | 20 | −46 | 19 | −21 | 36 | −39 |
| Conduct disorder | 135 | 99 | 148 | 111 | 68 | −50*** | 61 | −38* | 89 | −40*** | 105 | −5 | 162 | +20 |
| Depressive disorder | 45 | 19 | 54 | 39 | 13 | −71*** | 12 | −37 | 29 | −46* | 35 | −10 | 128 | +184*** |
| Eating disorders | 22 | 16 | 19 | 25 | 19 | −14 | 18 | +12 | 30 | +58 | 74 | +196*** | 89 | +305*** |
| Intellectual disability | 24 | 35 | 27 | 2 | 9 | −62 | 7 | −80*** | 11 | −59 | 19 | +850** | 19 | −21 |
| NSSH | 44 | 35 | 48 | 35 | 27 | −39 | 18 | −49 | 54 | +12 | 66 | +89* | 122 | +177*** |
| OCD | 12 | 9 | 6 | 9 | 4 | −67 | 9 | 0 | 7 | +17 | 6 | −33 | 15 | +25 |
| PTSD | 12 | 13 | 20 | 5 | 2 | −83 | 3 | −77 | 4 | −80** | 9 | +80 | 23 | +92 |
| Psychosocial problems | 112 | 96 | 106 | 69 | 26 | −77*** | 26 | −73*** | 36 | −66*** | 51 | −15 | 147 | +31 |
| Psychotic disorder | 27 | 14 | 22 | 10 | 5 | −81*** | 13 | −7 | 10 | −55 | 11 | +10 | 42 | +56 |
| SUD | 61 | 42 | 43 | 26 | 11 | −82*** | 16 | −61** | 20 | −53* | 21 | −19 | 37 | −39 |
| Suicidal ideation | 60 | 39 | 57 | 65 | 30 | −50* | 27 | −31 | 80 | +40 | 89 | +37 | 93 | +55* |
| Suicide attempt | 18 | 15 | 24 | 36 | 12 | −33 | 15 | 0 | 36 | +50 | 46 | +28 | 49 | +172*** |
Changes are relative to the corresponding season in the year before the COVID-19 lockdown. ADHD, attention-deficit/hyperactivity disorder; ASD, autism spectrum disorder; NSSH, non-suicidal self-harm; OCD, obsessive-compulsive disorder; PTSD, post-traumatic stress disorder; SUD, substance use disorder.
We found a 46% decrease (P<.001) in the number of admissions to the psychiatric ED during the lockdown compared to the 2019 spring (Table 1, Fig. 1). This decrease was observed across all age/gender groups, though it did not reach statistical significance in children. See Table 1 for statistics regarding specific diagnostic labels.
Admissions trends to the children and adolescent Psychiatry Emergency Department. Bar plot showing (a) expected (based on spring 2019 to winter 2020) versus observed global admissions across seasons; and observed admissions and accumulated deficit/excess across seasons due to (b) eating disorders, and (c) non-suicidal self-harm.
Conversely, we found a substantial 43% increase in the number of admissions to the psychiatric ED in the spring 2021 compared to the spring 2019 (P<.001), especially attributable to female adolescents, who showed a significant increase of 85%. We observed that anxiety, depressive disorders, eating disorders, non-suicidal self-harm (NSSH), suicidal ideation and suicide attempts showed a significant increment after lockdown, reaching a 55–305% increase (Table 1). Upward trends in admissions due to eating disorders, NSSH, suicidal ideation and suicide attempts were already observed since fall 2020. Gender differences for each diagnostic category are available in Figs. S1–3.
Sensitivity analysesThe excess of admissions during spring 2021 was similar to the deficit observed during the lockdown for many diagnostic categories (Table S2). However, the excess in eating disorders, NSSH, suicidal ideation and suicidal attempts exceeded the accumulated deficit, with the first two reaching statistical significance (Table S2, Fig. 1, S4). Remarkably, the cumulated excess for eating disorders was of 121% one year after the lockdown, indicating that the excess during the aftermath was not merely a compensation of the deficit during the lockdown.
DiscussionIn our study, we found that admissions of children and adolescents to the psychiatric ED rose by 43% during the spring 2021 compared to the same period in 2019. This was at the expense of female adolescents, who reached an increment of the 85% in 2021, and an accumulated excess of 10% after compensating for the deficit generated during the lockdown. Eating disorders, NSSH and suicide attempts also increased one-year after lockdown, exceeding 42–121% the previous deficit.
After an initial decrease in the number of psychiatric ED visits during lockdown, persistent restrictions, limited social interactions with peers, and difficulties in access to mental health services in the community, together with less fear of the virus, may have yielded the subsequent increase in the number of admissions found in our sample. Increase among girls aged 12–17 years is congruent with previous reports in the literature.8–11 Additionally, the effects of social deprivation and limited interactions with peers derived from COVID-19 lockdown may have been especially negative for the youth, with peer interactions becoming increasingly important, when compared to children or adults.12 Among different diagnoses, admissions due to eating disorders were notably three times higher in the spring 2021 than in the spring before the pandemic. Higher rates of eating disorders have been observed during COVID-19 lockdown, specially of anorexia nervosa, and more complex presentations11,13 who were more likely to require emergency care. Fear of gaining weight and subjective perception of weight gain may have played a role in the development of eating disorders.14 Furthermore, NSSH and suicide attempts increased by 172–176%, in line with previous evidence.5–7,15 Although special attention should have been paid to these conditions, it is really worrisome that many of these problems were anticipated,16 and potential solutions were proposed,17 but rarely applied.
Early onset of mental disorders during these periods can lead to heightened severity and a greater likelihood of more complex disorders later in life. Indeed, mental disorders among young people can lead to morbidity, mortality and dysfunction.18 We provided evidence that COVID-19 pandemic and posterior lockdown may have introduced an additional layer of risk, increasing the incidence of mental health problems among young individuals, thus impeding their transition into functional adulthood.
Among the strengths of our study, we included a substantial sample of youth from different socio-economic backgrounds, and individuals were evaluated by a trained psychiatrist, in contrast to previous studies in which evaluation was carried out mainly by pediatricians.8 Our study also controlled for potential confounders, such as season trends and potential changes in the total population of children and adolescents. We also considered that changes in admissions may have been caused by a compensation of the deficit found during the lockdown, and although it is expected that the deficit accumulated during the lockdown would be immediately compensated after the lifting, this conservative approach further improves the robustness of the results.
This study has also limitations. The retrospective chart review accounts for the limited quality of data concerning diagnosis categories, since they may depend on the evaluator. Nonetheless, clinical records were manually inspected by authorized clinicians to minimize this concern. Additionally, since our findings are from a single center, they may not be generalizable to other regions in Spain and/or worldwide, especially those with different COVID-19-related restrictions or outbreaks.
In conclusion, this study strongly suggests an upward trend of psychiatric ED admissions among adolescent girls, mainly related to eating disorders, NSSH, and suicide attempts, during the aftermath of COVID-19 lockdown. Adaptation of current children and adolescent mental health services may be required. However, further research is needed to evaluate future trends and to establish whether these changes continue or if they tend to stabilize/return to pre-pandemic levels.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interestsAF has received travel and educational support from Lundbeck, unrelated to the present work. MGR has received funding unrelated to the present work for research projects and/or honoraria as a consultant or speaker from the following entities: Angelini, Janssen, Lundbeck, Otsuka, Sanofi-Aventis and Spanish Ministry of Science and Innovation-Instituto de Salud Carlos III. GF has received CME-related honoraria, or consulting fees from Angelini, Janssen-Cilag and Lundbeck. AGP has received CME-related honoraria, or consulting fees from Angelini, Janssen-Cilag, Casen Recordati, and Lundbeck. MSV has received financial support for CME activities and travel funds from Janssen-Cilag, Lundbeck, Rovi, and Casen Recordati. MTP has received support from Lundbeck. MV has received honoraria from Otsuka. NB has received support from Janssen-Cilag, Otsuka-Lundbeck, Angelini Pharma, and Casen Recordati, and declares no support related to the subject of this article. FGA has received CME-related honoraria, or consulting fees from Otsuka-Lundbeck and Viatris, and reports no financial or other relationship relevant to the subject of this article. EP has received support from Janssen-Cilag and Otsuka-Lundbeck, Angelini Pharma, and Casen Recordati, and declares no support related to the subject of this article. EV has received grants and served as consultant, advisor, or CME speaker unrelated to the present work for the following entities: AB-Biotics, Abbott, Abbvie, Adamed, Angelini, Biogen, Dainippon Sumitomo Pharma, Ferrer, Gedeon Richter, Janssen, Lundbeck, Otsuka, Rovi, Sage, Sanofi-Aventis, Sunovion, Takeda, and Viatris. IB has received support to attend conferences or honoraria from Angelini, Janssen and Otsuka-Lundbeck. LF, LC, TMF, ML, LL and JR have no competing interests to declare that are relevant to the content of this article.
This research was supported by CIBER – Consorcio Centro de Investigación Biomédica en Red – (CB07/09/0004), Instituto de Salud Carlos III, Spanish Ministry of Science and Innovation. LF thanks the support from an educational grant from the Insituto de Salud Carlos III (FI20/00047). GF's work is supported by a fellowship from “La Caixa” Foundation (ID 100010434 – LCF/BQ/DR21/11880019). AGP receives support from an educational grant from Spanish Ministry of Health, Instituto de Salud Carlos III (CM21/00094) and by the European Social Fund Plus (FSE+). EV thanks the support of the Spanish Ministry of Science and Innovation (PI18/00805, PI21/00787) integrated into the Plan Nacional de I+D+I and co-financed by the ISCIII-Subdirección General de Evaluación and the Fondo Europeo de Desarrollo Regional (FEDER); the Instituto de Salud Carlos III; the Secretaria d’Universitats i Recerca del Departament d’Economia i Coneixement (2017 SGR 1365), the CERCA Programme, and the Departament de Salut de la Generalitat de Catalunya for the PERIS grant SLT006/17/00357. Thanks to the support of the European Union Horizon 2020 research and innovation program (EU.3.1.1. Understanding health, wellbeing and disease: Grant No. 754907 and EU.3.1.3. Treating and managing disease: Grant No. 945151). JR receives support from Instituto de Salud Carlos III and the European Regional Development Fund (FEDER) (CPII19/00009) and the Secretaria d’Universitats i Recerca del Departament d’Economia i Coneixement (2021 SGR 1128), and IB thanks the Instituto de Salud Carlos III and the Pons Bartran legacy (FCRB-IPB2-2023) for their support.