Patients with intellectual disabilities (ID) require antipsychotic drugs to treat conduct disorders; however, without adequate monitoring, this could lead to polypharmacy. To avoid this, the guidelines for prescription in ID recommend seeking the minimum effective dose, observing the clinical progress periodically, and prescribing a directed treatment in the case of psychiatric comorbidity.1 Experts especially suggest evaluating the presence of attention deficit hyperactivity disorder (ADHD) because of its prevalence in ID.1,2
Clonidine is an α-2 agonist that is an option for directly treating ADHD.2 It requires initial monitoring and gradual adjustment of the dose due to its effects on the cardiovascular system. In recent years, several studies have reported clinical improvements in resistant psychiatric disorders or conduct disorders when clonidine was added to the treatment.3–6 Furthermore, a few case reports have stated that antipsychotics can be deprescribed after sufficient stabilization of the condition is achieved with clonidine therapy.7,8
It is interesting that there is evidence to describe the efficacy of clonidine in resistant psychiatric disorders, while the improvement in polypharmacy has been reported only anecdotally.4–8 This may be because the current evidence focuses on clinical improvement and not on polypharmacy at follow-up. The aim of this report was to corroborate whether the use of clonidine can reduce the need for antipsychotics in populations with resistant conduct disorders associated with ID and mental illness.
This case series included patients with resistant conduct disorder associated with ID and mental illness in whom clonidine treatment was initiated in 2021 in the inpatient setting at Unidad Hospitalaria Especializada en Discapacidad Intelectual (UHEDI) of the Hospital Sant Joan de Déu Terres de Lleida. This is a long-term center specialized in ID.
At the initiation of the hospitalization, a mental health diagnosis and psychopharmacologic treatment were stated after a detailed clinical evaluation. In those cases in that the aggressiveness persisted despite a proper treatment of the mental disorder were evaluated with the Diagnostic Interview for ADHD in adults with Intellectual Disability (DIVA-5-ID)9 and clonidine were initiated. The defined daily dose (DDD) of antipsychotics was recorded first at the initiation of clonidine and four months after achieving the minimum effective dose of this drug while the patients were still hospitalized. Paired Wilcoxon test was used to determine statistically significant differences in DDD before and after clonidine initiation.
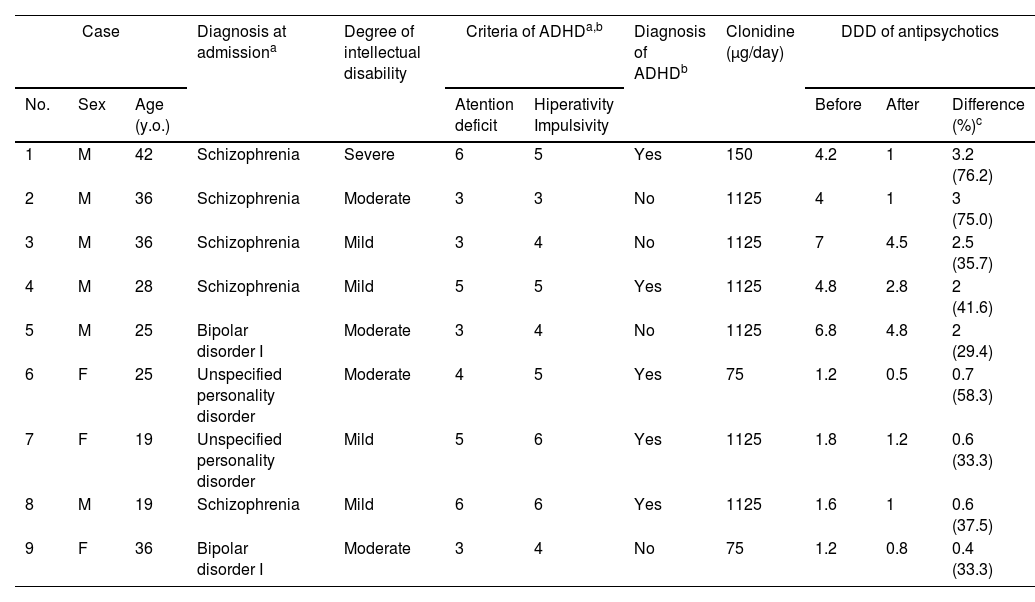
The sample consisted of nine patients (six men and three women), and the variables are summarized in Table 1. After applied the DIVA-5-ID interview the diagnosis of ADHD was reached in five cases. It was found that in all these resistant cases, the conduct was stabilized after the initiation of clonidine. Additionally and more important, a statistically significant difference reduction in the DDD of antipsychotics was observed in all cases at follow-up (p=0.004). This reduction was greater among men and participants with moderate to severe ID.
Variables recorded in the sample.
| Case | Diagnosis at admissiona | Degree of intellectual disability | Criteria of ADHDa,b | Diagnosis of ADHDb | Clonidine (μg/day) | DDD of antipsychotics | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| No. | Sex | Age (y.o.) | Atention deficit | Hiperativity Impulsivity | Before | After | Difference (%)c | ||||
| 1 | M | 42 | Schizophrenia | Severe | 6 | 5 | Yes | 150 | 4.2 | 1 | 3.2 (76.2) |
| 2 | M | 36 | Schizophrenia | Moderate | 3 | 3 | No | 1125 | 4 | 1 | 3 (75.0) |
| 3 | M | 36 | Schizophrenia | Mild | 3 | 4 | No | 1125 | 7 | 4.5 | 2.5 (35.7) |
| 4 | M | 28 | Schizophrenia | Mild | 5 | 5 | Yes | 1125 | 4.8 | 2.8 | 2 (41.6) |
| 5 | M | 25 | Bipolar disorder I | Moderate | 3 | 4 | No | 1125 | 6.8 | 4.8 | 2 (29.4) |
| 6 | F | 25 | Unspecified personality disorder | Moderate | 4 | 5 | Yes | 75 | 1.2 | 0.5 | 0.7 (58.3) |
| 7 | F | 19 | Unspecified personality disorder | Mild | 5 | 6 | Yes | 1125 | 1.8 | 1.2 | 0.6 (33.3) |
| 8 | M | 19 | Schizophrenia | Mild | 6 | 6 | Yes | 1125 | 1.6 | 1 | 0.6 (37.5) |
| 9 | F | 36 | Bipolar disorder I | Moderate | 3 | 4 | No | 75 | 1.2 | 0.8 | 0.4 (33.3) |
Note: ADHD: attention deficit hyperactivity disorder, M: male, F: female.
In recent years, there has been growing evidence regarding the clinical benefits of adding clonidine to the treatment of resistant psychiatric disorders.4–8 All reports have described a clinical improvement, but only a few have reported a decrease in polypharmacy.7,8 The purpose of this case series was to corroborate the effect of clonidine on the DDD of antipsychotics in the medium term in a population with resistant conduct disorder associated with ID and mental illness.
With respect to the clinical effect, it is interesting that clonidine stabilized complex cases where antipsychotics had failed. On the one hand, it could be related to what previous studies have called an antipsychotic effect of this drug that improves the resistant psychotic symptoms and, consequently, the behavior.4–8,10 On the other hand, it is possible that the stabilization was due to the antiaggressive effect of the clonidine described in ADHD2; it is important to point that in four cases this diagnosis was not reached with DIVA-5-ID. Nevertheless, the difficulty of establish the diagnosis of ADHD in ID have been recognized in clinical practice and literature, therefore it is possible that the results in this report represent cases of ADHD that could not been reached with this tool, if this is true, it would explain the resistance to non-specific treatment with antipsychotics, and the marked response to clonidine. Additionally, it could explain that it was deprescribed more in men and participants with moderate to severe ID, among whom ADHD has a higher incidence and severity, according to previous studies.2
Considering the results of this report, it is rational to consider clonidine as a treatment option in the population with conduct disorders associated with ID and mental illness due to its clinical efficacy and the possibility of offering a reduction in polypharmacy in the medium term, especially when comorbidity with ADHD is suspected. However, it is necessary to consider that the participants in this case series represent a clinical profile of an unusual resistance to treatments and were from a specific inpatient unit. Therefore, the informed results cannot be completely generalized to a larger population.
This case series shows that clonidine could improve the DDD of antipsychotics in a population with conduct disorders associated with ID and mental illness.
FinancingNo specific grants were received from public sector agencies, the private sector or not-for-profit entities for this research.
Conflicts of interestThe authors declare no conflicts of interest.
We thank to our colleagues at Hospital Sant Joan de Déu Terres de Lleida.