Symptomatology of schizophrenia is heterogeneous, there is not any pathognomonic symptom. Moreover, the diagnosis is difficult, since it is based on subjective information, instead of markers. The purpose of this study is to provide a review of the current status of blood-based biomarkers of psychopathological dimensions of schizophrenia. Inflammatory, hormonal or metabolic dysfunctions have been identified in patients with schizophrenia and it has attempted to establish biomarkers responsible for these dysfunctions. The identification of these biomarkers could contribute to the diagnosis and treatment of schizophrenia.
La sintomatología de la esquizofrenia es heterogénea, no existiendo ningún síntoma patognomónico de la misma. Además, su diagnóstico presenta dificultades, ya que se basa en información subjetiva en lugar de en marcadores. El propósito de este estudio es ofrecer una revisión del estado actual de los biomarcadores sanguíneos de las dimensiones psicopatológicas de la esquizofrenia. En pacientes con esquizofrenia se han observado disfunciones inflamatorias, hormonales o metabólicas y se ha intentado establecer los biomarcadores responsables de esas disfunciones. La identificación de estos podría contribuir al diagnóstico y tratamiento de la esquizofrenia.
Schizophrenia is a severe, complex and multifactor mental disorder that is characterised by its broad phenotypic variation, heterogeneous aetiology and fluctuating evolution. It commences in late adolescence or early adulthood and includes symptoms that are positive, negative, affective and cognitive. It affects at least 0.7% of the population.1,2
The symptoms of schizophrenia are heterogeneous, and it has no pathognomic symptom. It is also hard to diagnose, given that this is based on subjective information supplied by the patients themselves, or on the skill of the clinician in drawing inferences, rather than on markers such as laboratory tests or neuroimaging techniques. Due to this, current research centres on seeking markers which would make it possible to evaluate results in a more sensitive and precise way. Biological as well as neurophysiological markers were therefore studied, together with the psychiatric phenotype. Chan et al. reviewed a selection of studies of blood biomarkers in schizophrenia, bipolar disorder and major depression patients, to emphasise the importance of implementing valid biomarkers that not only make diagnosis and effective treatment possible, but which also improve the prognosis for patients.3 The National Institute of Mental Health, in turn, has commenced the Research Domain Criteria Project,4 the aim of which is to increase knowledge about the brain–behaviour relationship and to introduce this information about neural dysfunction in clinical practice, so that more effective treatments can be developed.
This study reviews the current status of blood biomarkers in the psychopathological dimensions of schizophrenia.
The positive dimensionThere are no problems respecting the positive dimension of schizophrenia, as the instruments traditionally used measure it sufficiently well. The 2 most widely used scales in research as well as clinical practice are the Scale for the Assessment of Positive Symptoms5 and the Positive and Negative Syndrome Scale for Schizophrenia (PANSS).6–8
Respecting the biomarkers for the positive dimension, a significant relationship has been detected between triglyceride levels in serum and the positive symptoms evaluated using the positive scale of the PANSS.9 Additionally, a statistically significant inverse relationship has been detected between the plasma glucose levels and the positive symptoms evaluated using the PANSS, showing that an altered glucose metabolism may be associated with the pathogenesis and symptoms of schizophrenia in the early stages of the disease.10 These authors conclude that the factors which best predict glucose levels in schizophrenia patients are insulin resistance, insulin and the positive symptom score in the PANSS.10 Weight gain during antipsychotic treatment, in turn, predicts an improvement in the psychotic syndrome and positive symptoms.11
Alterations have also been detected in several inflammatory parameters: the levels of interleukin (IL)-1β seem to increase during acute phases12 and the initial stages of the disease,13 while levels of TGF-β and IL-6 also increase during acute phases.12 Increased positive symptoms (hallucinations and deliria) seem to be associated with interleukin expression in schizophrenia patients;14 thus for example, Dimitrov et al.15 found a positive association between IL-6 levels and the positive symptoms evaluated using the PANSS. Tumour necrosis factor (TNF)-α has also been associated with the severity of the positive dimension,16 as well as the number of hospitalisations and episodes of imbalance that reflect greater severity,17 indicating the possibility that it may be a specific biomarker for this dimension. All of these data show the existence of state-specific markers, i.e., during the first psychotic episodes and acute relapses a series of inflammatory and associated immune processes arise.12,18 Likewise, a positive relationship has been detected between peripheral levels of PCR and the severity of positive symptoms.19
Finally, the endocannabinoid system has been described as an endogenous anti-inflammatory neuroprotector system, and certain markers of this system, such as raised levels of anandamide, have been associated with positive symptoms.20
The negative dimensionThe negative dimension of schizophrenia has traditionally been measured using the Brief Psychiatric Rating Scale,21 the Scale for the Assessment of Negative Symptoms22 and the PANSS.6,22 Additionally, Marder et al. established the negative factor of the PANSS by means of factorial analysis. Nevertheless, the PANSS and even the negative factor obtained by Marder et al.23 have important conceptual and psychometric limitations.24,25
This negative dimension has become of greater interest in recent years due to the diagnostic and therapeutic challenge it involves, together with the great impact of its cognitive symptoms on the functioning of individuals with schizophrenia.24 Negative symptoms show minimum response to antipsychotic medication, and they are therefore an attractive target for the development of new treatments. However, no antipsychotic drug used to date has proven effective in the treatment of the said symptoms.26 Moreover, these symptoms are recognised, evaluated and recorded to a lesser extent than the positive symptoms, in spite of their persistence and impact. This is partially due to the limitations of evaluation tools. However, thanks to the National Institute of Mental Health initiative,27–29 psychometric evaluation is developing swiftly, together with methodological refinement24 thanks to the creation of new scales such as the Clinical Assessment Interview for Negative Symptoms30 and the Brief Negative Symptom Scale.31
Regarding negative dimension biomarkers, post mortem studies of the brain and cerebrospinal fluid of patients with schizophrenia with negative symptoms have found a reduction in dopaminergic, noradrenergic and serotoninergic activity.32 Ventricular widening is associated with the severity of negative symptoms, low monoamine activity and reduced cerebral glucose metabolism activity.32 Additionally, an improvement in glutamatergic transmission has been associated with a reduction in negative symptoms.32 Stradiol, the most powerful female hormone, influences not only primary and secondary sexual characteristics, but also embryonic and foetal growth and the development of brain aminergic networks which are involved in schizophrenia. Stradiol would have neuroprotector properties that may be relevant in the course of schizophrenia, and they could explain the gender differences that exist in terms of progression, negative symptoms and the therapeutic response of patients with schizophrenia.32 According to Kaneda and Ohmori, stradiol concentrations would be a possible biomarker for negative symptoms in men.33 The levels of S100B (a protein produced by the astroglias that regulates the balance between the proliferation and differentiation of neurons and glial cells) in serum have also been mentioned as a possible biomarkers of negative symptoms in schizophrenia.34
Arachidonic acid, a polyunsaturated omega-6 PUFA fatty acid, and docosahexaenoic acid, a polyunsaturated omega-3 PUFA fatty acid, are inversely correlated with the negative syndrome in schizophrenia patients, and treatment with antipsychotic drugs seems to increase these levels.35 According to Chen et al.36 triglycerides and HDL cholesterol are possibly the 2 main lipid components involved in the development of schizophrenia and the negative syndrome. They found a negative relationship between negative symptoms and triglycerides, and a positive relationship between them and HDL cholesterol36 (Table 1). Another study found that high levels of triglycerides and total cholesterol are associated with a reduction in negative symptoms.37 Additionally, negative symptoms correlate negatively with the BMI.36 Likewise, a higher prevalence of metabolic syndrome was observed in patients with schizophrenia with negative symptoms.38
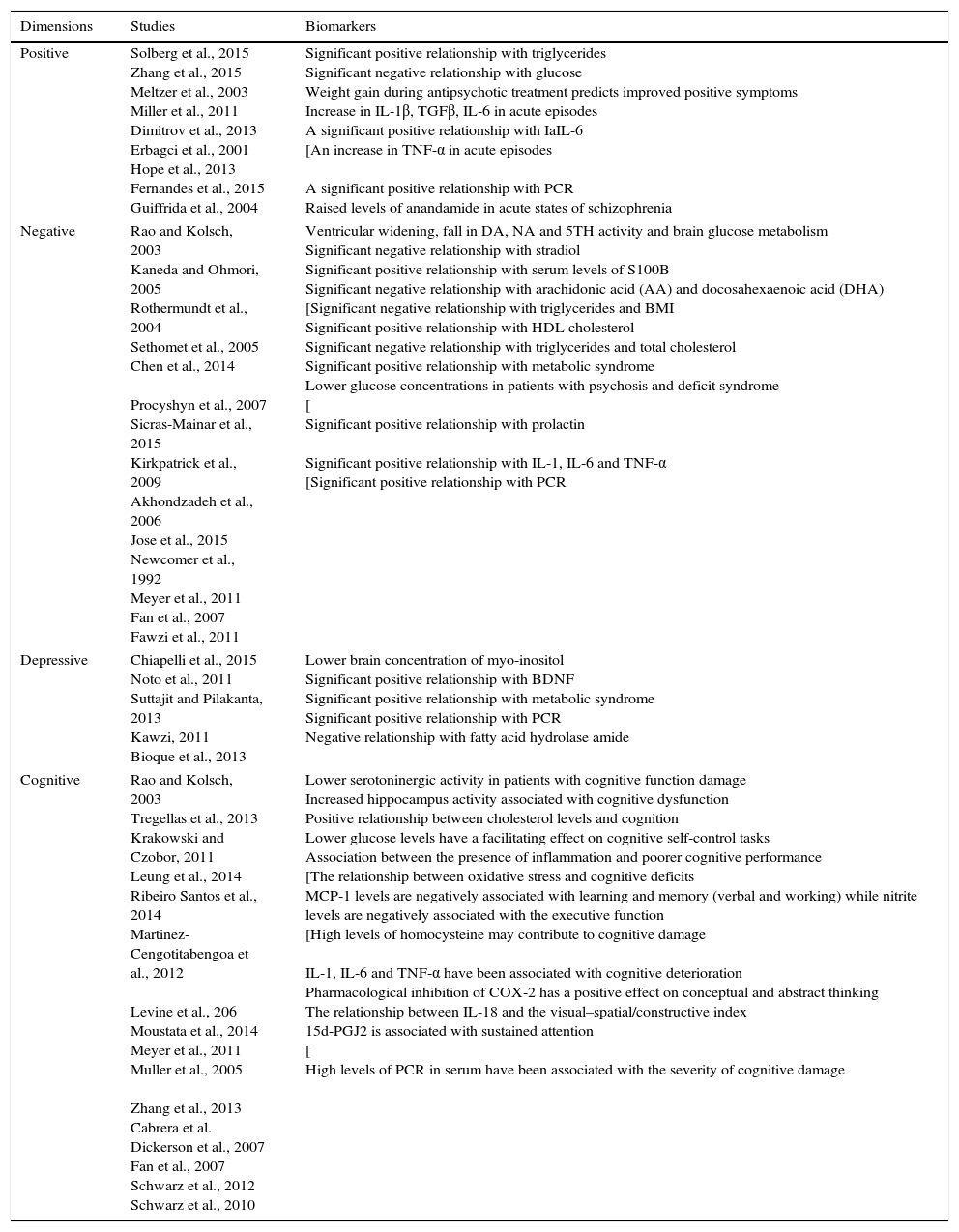
The most significant empirical studies.
| Dimensions | Studies | Biomarkers |
|---|---|---|
| Positive | Solberg et al., 2015 Zhang et al., 2015 Meltzer et al., 2003 Miller et al., 2011 Dimitrov et al., 2013 Erbagci et al., 2001 Hope et al., 2013 Fernandes et al., 2015 Guiffrida et al., 2004 | Significant positive relationship with triglycerides Significant negative relationship with glucose Weight gain during antipsychotic treatment predicts improved positive symptoms Increase in IL-1β, TGFβ, IL-6 in acute episodes A significant positive relationship with IaIL-6 [An increase in TNF-α in acute episodes A significant positive relationship with PCR Raised levels of anandamide in acute states of schizophrenia |
| Negative | Rao and Kolsch, 2003 Kaneda and Ohmori, 2005 Rothermundt et al., 2004 Sethomet et al., 2005 Chen et al., 2014 Procyshyn et al., 2007 Sicras-Mainar et al., 2015 Kirkpatrick et al., 2009 Akhondzadeh et al., 2006 Jose et al., 2015 Newcomer et al., 1992 Meyer et al., 2011 Fan et al., 2007 Fawzi et al., 2011 | Ventricular widening, fall in DA, NA and 5TH activity and brain glucose metabolism Significant negative relationship with stradiol Significant positive relationship with serum levels of S100B Significant negative relationship with arachidonic acid (AA) and docosahexaenoic acid (DHA) [Significant negative relationship with triglycerides and BMI Significant positive relationship with HDL cholesterol Significant negative relationship with triglycerides and total cholesterol Significant positive relationship with metabolic syndrome Lower glucose concentrations in patients with psychosis and deficit syndrome [ Significant positive relationship with prolactin Significant positive relationship with IL-1, IL-6 and TNF-α [Significant positive relationship with PCR |
| Depressive | Chiapelli et al., 2015 Noto et al., 2011 Suttajit and Pilakanta, 2013 Kawzi, 2011 Bioque et al., 2013 | Lower brain concentration of myo-inositol Significant positive relationship with BDNF Significant positive relationship with metabolic syndrome Significant positive relationship with PCR Negative relationship with fatty acid hydrolase amide |
| Cognitive | Rao and Kolsch, 2003 Tregellas et al., 2013 Krakowski and Czobor, 2011 Leung et al., 2014 Ribeiro Santos et al., 2014 Martinez-Cengotitabengoa et al., 2012 Levine et al., 206 Moustata et al., 2014 Meyer et al., 2011 Muller et al., 2005 Zhang et al., 2013 Cabrera et al. Dickerson et al., 2007 Fan et al., 2007 Schwarz et al., 2012 Schwarz et al., 2010 | Lower serotoninergic activity in patients with cognitive function damage Increased hippocampus activity associated with cognitive dysfunction Positive relationship between cholesterol levels and cognition Lower glucose levels have a facilitating effect on cognitive self-control tasks Association between the presence of inflammation and poorer cognitive performance [The relationship between oxidative stress and cognitive deficits MCP-1 levels are negatively associated with learning and memory (verbal and working) while nitrite levels are negatively associated with the executive function [High levels of homocysteine may contribute to cognitive damage IL-1, IL-6 and TNF-α have been associated with cognitive deterioration Pharmacological inhibition of COX-2 has a positive effect on conceptual and abstract thinking The relationship between IL-18 and the visual–spatial/constructive index 15d-PGJ2 is associated with sustained attention [ High levels of PCR in serum have been associated with the severity of cognitive damage |
Some studies have observed other metabolic anomalies, such as diabetes, in patients with schizophrenia. The increased risk of this seems to be independent of the use of antipsychotic drugs39,40 or poor health habits, and an increased risk is also even observed in the family members of these patients.40 Nevertheless, a recent study found a comparable glucemic state in patients with schizophrenia untreated by antipsychotic drugs and healthy controls, and subsequently antipsychotic drug treatment was associated with a glucose regulation alteration.41 A study that compared 3 groups: patients with non-affective psychosis with deficit syndrome, i.e., with primary negative symptoms and a lack of discomfort or dysphoria; patients with psychosis without this syndrome, both recently diagnosed and therefore untreated by antipsychotic drugs; and control subjects, found significantly higher concentration of glucose in patients with psychosis and without deficit syndrome in comparison with patients with deficit syndrome. The latter in turn had significantly higher levels than the control subjects. Nevertheless, as these authors conclude, the results are not consistent with an interpretation according to which the group with deficit syndrome would have a more severe version of the same dysfunction, i.e., anomalous glucose metabolism. However, they did show that the differences between deficit syndrome and no deficit syndrome go beyond psychopathology.42 On the other hand, it has been suggested that the PPARγ gene is involved in the alteration of glucose levels. Nevertheless, it is not known whether this gene is able to modify the risk of metabolic anomalies or psychosis, or whether it causes metabolic anomalies which lead to psychosis.43
Prolactin levels in patients con schizophrenia have also been associated with increased negative symptoms,44–46 although they have not been associated with positive symptoms or the psychopathology in general.45
Respecting the immuno-inflammatory parameters, IL-1, IL-6 and TNF-α have been linked to negative symptoms.47 Additionally, higher levels of PCR in patients with schizophrenia48,49 have been associated with greater psychopathological severity as shown by the total score in the PANSS,50,51 in the negative scub-scale50,51 and in the general sub-scale.50 Nevertheless, this has not been observed with the positive sub-scale in some studies,50,51 although this is not so in all of them.19
The depressive dimensionRespecting the affective dimension of schizophrenia, depressive symptoms are common and form a central part of the disease.52 They are also associated with a high rate of relapse, suicidal ideas, increased mortality, less social adjustment and a poor quality of life.53–55 The level of depression has been evaluated using specific scales for this population, such as Calgary's Depression Scale,56 as well as general scales used for patients with depressive disorders such as Hamilton's Scale for Depression.57
According to Chiappelli et al.58 although there is no biomarker for depression in schizophrenia they suggest a lower concentration of myo-inositol in the brain as one of the potential neurochemical biomarkers. The neurotrophic factor deriving from the brain has, in turn, been positively associated with the symptoms of depression in schizophrenia.59
Low levels of cholesterol have also been associated with depression and affective disorders, as they may reduce the expression of serotoninergic receptors and cause a reduction in serotoninergic activity.60 Nevertheless, in recent years this relationship has been called into question, given that some authors observed no relationship between cholesterol level and psychiatric disorders.61 The metabolic syndrome has been linked with depression in schizophrenia, more specifically with depressed mood, moderate insomnia and delay or inhibition.62
In connection with the immuno-inflammatory markers, higher levels of PCR have been linked with depression non-psychotic patients63 as well as in patients with schizophrenia.51. Wen et al.64 observed low levels of uric acid, a potential anti-oxidant, in depression but not in other disorders such as schizophrenia; however, no studies centre on evaluating these levels in patients with schizophrenia and predominantly depressive symptoms.
Finally, hydrolase fatty acid expression, an endocannabinoid system marker, has been shown to have a negative relationship with depressive symptoms in FEP.65
The cognitive dimensionFinally, neurocognitive faults have also been widely documented and are considered to be a core characteristic of schizophrenia.66–70 These faults would be relatively independent of psychotic symptoms71,72 and detectable before any sign of the disease.73,74 Moreover, the cognitive deterioration shown by patients during a psychotic episode is similar to that which is observed in the same patients when the symptoms are under control.75 This is why the correlations between the severity of psychotic symptoms and cognitive evaluation measurements are usually zero.76,77 On the other hand, a sub-group of first degree schizophrenia patient family members without psychotic symptoms have displayed a pattern of cognitive alterations similar to those found in patients with schizophrenia.78,79 This shows that certain cognitive alterations may be components of a genetic vulnerability for schizophrenia.
The most common cognitive faults include attention deficit, memory deficit (episodic and working), visual-spatial coordination and executive functions.80–85 The data show a strong connection between these faults and the degree of functioning in patients with schizophrenia.69,86 The presence and severity of cognitive symptoms must therefore be considered an important factor to determine the evolution of the disease,87,88 as they are associated with a more severe course of the disease and frequent use of psychiatric departments.89
Increasing knowledge about neurocognitive faults and their impact on functioning has led to greater interest in possible interventions that could relieve these deficits, as well as in the creation of standardised batteries that would make it possible to measure neurocognition. Due to this the National Institute of Mental Health created the initiative Measurement and Treatment Research to Improve Cognition in Schizophrenia or MATRICS. One of the objectives of this is to create a cognitive battery by consensus that would make it possible to evaluate the said dimension in clinical trials for schizophrenia.90 Other neuropsychological tests are also available for schizophrenia and other psychoses, such as the Brief Assessment of Cognition in Schizophrenia91 or the Screen for Cognitive Impairment in Psychiatry.92
Post-mortem studies of the brand and cerebrospinal fluid in patients with schizophrenia have shown that serotoninergic activity seems to be reduced, not only in those patients with negative symptoms, but also in those with damage to the cognitive function.32 Increased activity of the hippocampus is a characteristic of schizophrenia that has been found to be broadly associated with cognitive dysfunction, so that it has been suggested as a candidate biomarker for therapeutic development.93
Respecting analytical determinations, Krakowski and Czobor94 found a positive relationship between cholesterol levels and cognition in patients with schizophrenia. This associated was especially marked for verbal memory. Additionally, they observed no interaction between medication in the different groups of patients (clozapine, olanzapine or haloperidol) and cholesterol level. I.e., the positive relationship was independent of medication. Some of the explanations which have been offered for these findings include the hypothesis that serum concentrations of cholesterol may influence serotoninergic and cholinergic neurotransmission, or that they correlate with polyunsaturated fatty acids.94,95 Cholesterol may be a marker for polyunsaturated fatty acids, which are involved in the composition of the neuronal membrane and in the synthesis of cholinergic and serotoninergic neurotransmissors. However, in patients with euthymic bipolar disorders those who are obese were found to function less well cognitively than those with bipolar disorder and healthy controls of normal weight.96 These authors suggest that there are several factors which may moderate the association between obesity and cognition in bipolar disorder, such as anthropometric data and lipidometry, as these may mediate the impact of the distribution of body fat in cognition.96
In connection with glucose, reduced levels of the same have been found to have a facilitating effect in patients with schizophrenia during cognitive self-control tasks, but not during physical self-control tasks.97
Inflammation markers have recently been associated with the cognitive function in schizophrenia, showing an association between the presence of inflammation and worse cognitive performance.98 In FEP a connection has also been found between cognitive deficits and oxidative stress.99 Patients with FEP have lower levels of antioxidants, catalase and peroxidase glutation in comparison with healthy controls. Levels of MCP-1 are negatively associated with learning and memory (verbal and working), while nitrite levels are negatively associated with executive function. Finally, glutation levels are associated positively with the executive function.99 Homocysteine, another oxidative marker that is raised in patients with schizophrenia100,101 seems to play an important role in cognitive processes, as has been found in studies that measure levels of homocysteine in elderly healthy subjects.102,103 Based on these data, it has been suggested that high levels of homocysteine may contribute to the cognitive damage observed in patients with schizophrenia.104,105 Nevertheless, in some studies with FEP no association was found between homocysteine levels and cognition, showing that levels of homocysteine may vary with clinical state, with higher levels in more advanced stages of the disease.106,107
Cytosines may play a central role in complex functions of the CNS such as cognition. Thus IL-1, IL-6 and TNF-α have been linked to cognitive deterioration.47 The pro-inflammatory role of cytosines is mediated by prostaglandins and COX-2. It has been suggested that COX-2 is involved in cognitive function, as in animal models it was found to play an inhibitory role in the strength of synaptic connectivity, which is critical for learning and the consolidation of memory.108 Moreover, Muller et al.109 observed a positive effect on conceptual and abstract thought after pharmacological inhibition of COX-2, showing that COX2 inhibition probably influences different aspects of cognition, more specifically those associated with the prefrontal cortex. Zhang et al.110 found a relationship between the visuospatial/constructional index and IL-18. Animal models show the neuroprotector role of prostaglandins in the CNS.111 A recent study with FEP found a relationship between sustained attention and 15d-PGJ2 after controlling possible confusion factors (age, sex, years of education, BMI, cannabis, tobacco and antipsychotic drug level); better performance in sustained attention tasks was associated with higher levels of anti-inflammatory expression (15d-PGJ2), leading the suggestion of considering this to be a protective factor for cognition.107 Finally, high levels of PCR in serum have been associated with the severity of cognitive damage in patients with schizophrenia50,112–114 and in patients with bipolar disorder.115 Additionally, a recent study found an association between raised levels of PCR and sensory alterations (altered P50 suppression) in patients with schizophrenia.116
To conclude, different elements within the endocannabinoid system have been associated with different cognitive dominions in PEP.117
ConclusionsCurrent research into schizophrenia centres on the search for biomarkers that make it possible to evaluate the disease and make a less subjective diagnosis. Biomarkers have therefore been studied in connection not only with schizophrenia in general, but also with each one of its dimensions.
The positive dimension has been positively associated with triglycerides and negatively associated with glucose and weight gain. Immuno-inflammatory parameters (IL-1β, TGF-β, IL-6, TNF-α and PCR) have also been found to be positively associated with acute phases.
The negative dimension has been positively associated with ventricular widening, levels of S100B in serum, HDL cholesterol, metabolic syndrome, prolactin and immuno-inflammatory parameters (IL-1, IL-6, TNF-α and PCR). It has been associated negatively with dopamine activity, noradrenalin, serotonin, stradiol, arachidonic acid, docosahexaenoic acid, triglycerides, BMI, total cholesterol and glucose.
The depressive dimension has been linked positively to brain derived neurotrophic factor, the metabolic syndrome and PCR, and it has been negatively linked to the concentration in the brain of myo-inositol.
Finally, the cognitive dimension has been positively associated with cholesterol. On the other hand, reduced serotoninergic activity, increased hippocampus activity and immuno-inflammatory parameters (homocysteine, IL-1, IL-6, TNF-α and PCR) have been linked to cognitive deterioration. Some biomarkers have also been associated with specific cognitive tasks.
Nevertheless, in spite of all these studies, to date none of the biomarkers studied has achieved levels of precision that would allow it to be used in the diagnosis and treatment of individuals with schizophrenia.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Garcia-Alvarez L, Garcia-Portilla MP, Gonzalez-Blanco L, Saiz Martinez PA, de la Fuente-Tomas L, Menendez-Miranda I, et al. Biomarcadores sanguíneos diferenciales de las dimensiones psicopatológicas de la esquizofrenia. Rev Psiquiatr Salud Ment (Barc.). 2016;9:219–227.