Skeletal class III is the result of mandibular prognathism, growth deficiency of the maxilla or a combination of both. Historically, surgical correction of class III has been achieved only by mandibular setback surgery. With advances in knowledge and techniques, corrective surgery progressed to include bimaxillary and triple surgery (maxilla, mandible and chin). In the last decade, the frequency of jaw surgery decreased less than 10% class III patients, while bimaxillary surgery has come to use in about 40% of the class III patients. Both, bimaxillary surgery and surgery, can improve occlusion, masticatory function and aesthetics, significantly changing the position of the mandible, maxilla and chin. It is intended to explain the development and result in a Class III patient whose treatment was triple orthognathic surgery (anterior segmental, reverse sagittal osteotomy and forward genioplasty).
La clase III esquelética es el resultado del prognatismo mandibular, deficiencia en el crecimiento del maxilar o una combinación de las dos anteriores. Históricamente, la corrección quirúrgica de la clase III se lograba sólo mediante cirugía de retroceso mandibular. Con los avances en los conocimientos y técnicas, la cirugía correctiva progresó para incluir cirugías bimaxilares y triples (maxilar, mandíbula y mentón). En la última década, la cirugía mandibular disminuyó en frecuencia a menos de 10% de los pacientes de clase III, mientras que la cirugía bimaxilar se ha llegado a utilizar en aproximadamente el 40% de los pacientes clase III. Tanto la cirugía bimaxilar como la cirugía triple pueden mejorar la oclusión, la función masticatoria, y la estética cambiando notablemente la posición de la mandíbula, del maxilar y del mentón. Se pretende dar una explicación del desarrollo y resultado obtenido en un paciente clase III cuyo tratamiento fue una cirugía triple ortognática (segmentaria anterior, osteotomía sagital de retroceso y mentoplastia de avance).
Malocclusions with a skeletal problem origin, which require orthodontic treatment or surgical instruments for its correction, occur in approximately 4% of the population. The most common are severe class II, class III, and the vertical skeletal discrepancies in patients without growth. Among the skeletal malformations, class III patients have a high percentage of surgical-orthodontic treatment for their correction.1
Proffit et al reported that 20% of patients had mandibular excess, 17% maxillary deficiencies and 10% of the population had both.
Most people with dento-alveolar class III malocclusions have skeletal problems and the mild cases can often be treated with orthodontics only.2,3 However, patients with skeletal class III malocclusions with significant discrepancies are often treated with mandibular, maxillary or bimaxillary orthognathic surgery in combination with orthodontics.2–4
Few studies have examined the factors that influence the decision between conventional orthodontic treatment and surgical/orthodontic treatment. Kerr et al reported that patients with ANB angles lower than -4° and with inclinations of the mandibular incisors of less than 83° were more likely to have surgical/orthodontic treatment.2 A more recent study concluded that surgical patients could be distinguished from the non-surgical on the basis of the measurement of the values of the Witts appraisal, maxilla/mandible relationship, mandibular length, gonial angle, and the relationship mandibular length and distance sella-nasion.4,5
Treatment of the skeletal class III malocclusions is a significant clinical challenge due to the complex diagnosis and difficult prognosis, especially when the class III is associated with a skeletal or dental asymmetry.6 There are two main treatment options for a class III malocclusion that is diagnosed after growth has been completed: orthodontic treatment with extractions and orthognathic surgery.7 For many patients with a class III malocclusion, surgical treatment is the best alternative.7
Johnston et al, concluded in a study conducted in surgically corrected class III patients that the surgical/ orthodontic treatment is very successful in the overjet correction. Although the anteroposterior skeletal correction (ANB angle) is less successful than the overjet correction, the majority of patients ended up with soft tissues profiles within normal parameters. Bimaxillary surgery was used in 75% of patients who had more severe skeletal and dental discrepancies that the ones treated with mandibular procedures only. However, bimaxillary surgery was 3.4 times more likely to fully correct the ANB angle than mandibular surgery.1
The main objectives of the surgical/orthodontic treatment are to normalize occlusion, function and the facial profile.8–10
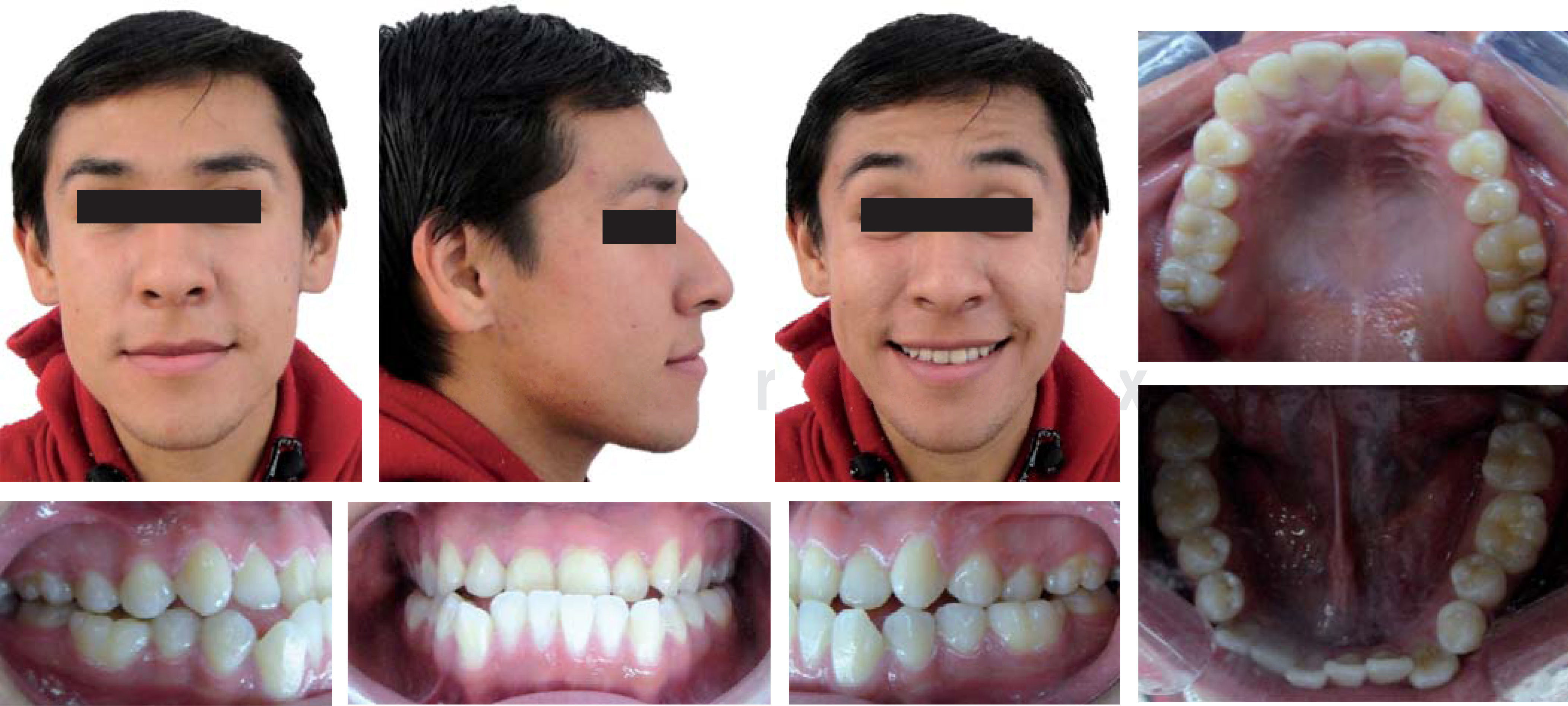
CASE REPORTDiagnosisMale patient, 22 years of age, was referred to the Orthodontics clinic at the Division of Post-Graduate Studies and Research of the National University of Mexico (UNAM) by his Maxillofacial Surgeon because he presented a problem of prognathism. While performing the medical history chart it was found that the patient was apparently healthy. Upon intraoral examination no pathologies or temporomandibular disorders were found. At the photographic analysis it was observed that the patient was dolichofacial, asymmetrical, had the facial middle third depressed at the level of the malar bone, an almost straight profile, and an upper dental midline that coincided with the facial midline. It was also found that the patient had a bilateral molar class III, bilateral canine class III, bilateral anterior and posterior crossbite, deviated upper and lower dental midlines, moderate crowding in the upper and lower anterior segment, negative overjet and asymmetric, squared archforms (Figure 1).
In the panoramic radiograph it was observed that all the teeth were permanent, with absence of the upper and lower left third molars, asymmetric condyles as well as the maxillary sinuses without infectious occupation and continuous alveolar processes without any intraosseous pathology (Figure 2).
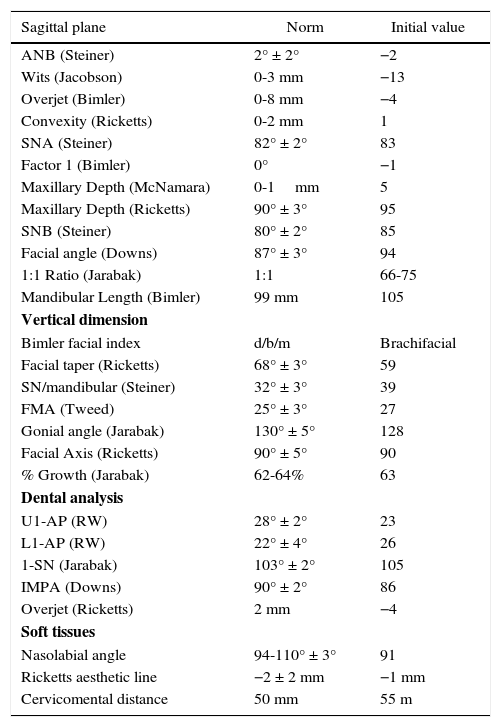
The cephalometric data showed a skeletal class III patient due to prognathism with a brachifacial pattern, a neutral growth tendency and upper and lower incisor proclination (Figure 3yTable I).
UNAM Integrated analysis.
| Sagittal plane | Norm | Initial value |
|---|---|---|
| ANB (Steiner) | 2° ± 2° | −2 |
| Wits (Jacobson) | 0-3 mm | −13 |
| Overjet (Bimler) | 0-8 mm | −4 |
| Convexity (Ricketts) | 0-2 mm | 1 |
| SNA (Steiner) | 82° ± 2° | 83 |
| Factor 1 (Bimler) | 0° | −1 |
| Maxillary Depth (McNamara) | 0-1mm | 5 |
| Maxillary Depth (Ricketts) | 90° ± 3° | 95 |
| SNB (Steiner) | 80° ± 2° | 85 |
| Facial angle (Downs) | 87° ± 3° | 94 |
| 1:1 Ratio (Jarabak) | 1:1 | 66-75 |
| Mandibular Length (Bimler) | 99 mm | 105 |
| Vertical dimension | ||
| Bimler facial index | d/b/m | Brachifacial |
| Facial taper (Ricketts) | 68° ± 3° | 59 |
| SN/mandibular (Steiner) | 32° ± 3° | 39 |
| FMA (Tweed) | 25° ± 3° | 27 |
| Gonial angle (Jarabak) | 130° ± 5° | 128 |
| Facial Axis (Ricketts) | 90° ± 5° | 90 |
| % Growth (Jarabak) | 62-64% | 63 |
| Dental analysis | ||
| U1-AP (RW) | 28° ± 2° | 23 |
| L1-AP (RW) | 22° ± 4° | 26 |
| 1-SN (Jarabak) | 103° ± 2° | 105 |
| IMPA (Downs) | 90° ± 2° | 86 |
| Overjet (Ricketts) | 2 mm | −4 |
| Soft tissues | ||
| Nasolabial angle | 94-110° ± 3° | 91 |
| Ricketts aesthetic line | −2 ± 2 mm | −1 mm |
| Cervicomental distance | 50 mm | 55 m |
Based on the diagnosis the following objectives were determined: to correct the facial biotype, correct the profile created by the skeletal discrepancy and obtain molar and canine class I, eliminate crowding as well as to obtain centered dental midlines, to compensate incisor proclination and correct the skeletal discrepancy by means of orthognathic surgery.
Treatment planIt was suggested to the patient two treatment plans, the first was orthodontic treatment (0.022” Roth prescription with upper and lower bands in first and second molars, archwire sequence in accordance to the technique) with extractions of first premolars and reverse genioplasty. The second treatment option was orthodontic treatment with dental decompensation for a triple orthognathic surgery: segmental surgery with rotation and forward repositioning of the anterior portion of the maxilla with the intention of decreasing the upper incisor proclination, improve the profile and the midfacial depression; sagittal split osteotomy of the mandible to its subsequent retro-positioning and genioplasty. The second treatment plan was the most recommended and therefore, it was accepted.
Treatment progressUpper and lower fixed appliances with Roth prescription, 0.022” slot (GAC®), and bands with the same prescription (Ah Kim Pech®) were placed in the first and second upper and lower molars. Treatment began with an 0.014” niti archwire on the upper and lower arch and Phase I was finished with an upper and lower 0.019” × 0.025” SS archwire (American Orthodontics) (Figure 4).
At this point in treatment, once the malocclusion was decompensate study models were obtained to assess the post-surgery occlusion and considering this, (no adjustments were made since the occlusion was close to ideal) the patient was referred to the Maxillofacial Surgeon for placement of the surgical splints used during surgery. Crimpable Hooks were placed mesial to the right second molars and mesial to the left second molars in both the upper and lower arch. The archwire was cut distal to the right and left canines and then, the triple orthognathic surgery was performed (Figure 5).
The Maxillofacial Surgeon began the surgery performing an osteotomy in the anterior segment (from canine to canine) of the maxilla; it was advanced 4mm and fixed with monocortical titanium screws and two mini plates. Subsequently osteotomies were performed between the mandibular body and ramus (mandibular setback sagittal split osteotomy) with the subsequent 7mm setback. The new mandibular position was fixed with elastomeric chains placed in zigzag from the upper teeth to the lower by means of crimpable hooks. The osteotomies were fixed with monocortical titanium screws. Finally, the 2mm advancement genioplasty was performed by placing a titanium plate fixed with 4 titanium miniscrews.
A week after surgery 3/8”, 6 oz of force class III elastics were placed and three weeks later the segmented surgical archwire was substituted by a 0.017” × 0.025” CuNiti archwire with a distal bendback to bodily intrude the anterior segment without losing much tipping and torque (Figures 6 and 7).
Once the occlusion was leveled, the upper second premolars and lower canine brackets were repositioned along with the lower left central incisor. While assessing the overbite the decision was taken to perform stripping of the lower central and lateral incisors. The spaces were closed with a 0.017” × 0.025” SS lower archwire and a short elastomeric chain (American Orthodontics).
At the finishing stage, a 0.019” × 0.025” SS archwire was placed in the lower arch and in the upper, a braided 0.019” × 0.025” with 3/8”, 3.5 oz settling elastics in zigzag from the upper cuspid to the lower second bicuspid (Figure 8).
The appliances were removed and upper and lower circumferential retainers were placed as retention. A prefinisher was manufactured in the laboratory for post-surgical contention, instructing the patient to wear it at night (Figure 9).
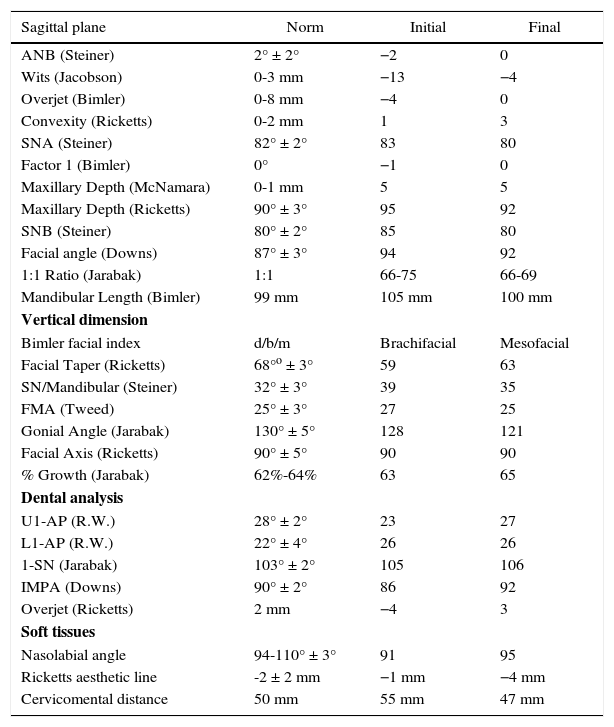
RESULTSThe results were obtained by comparing the initial and final cephalometric values, intraoral and facial photographs and study models.
• Extraoral analysis
The frontal photography shows an oval and dolichofacial face; in the lateral photograph a convex profile with a deep mentolabial fold was observed as well as a slight increase in the nasolabial angle. At the smile photograph a high smile with increased teeth display, coincident dental midlines and the total elimination of crowding was observed (Figure 10).
• Intraoral analysis
When comparing the initial and final photographs the alignment and leveling of the upper and lower teeth was evident; a canine Class I and Class I molar, a correct occlusal settlement both in the anterior segment as well as the posterior; a normal overbite and overjet, symmetrical and oval upper and lower arches may be observed (Figure 11).
• Radiographic analysis
Cefalometrically, a significant change in all the sagittal measurements was observed, leaning towards a Class I patient with a decrease in the position of the mandible and the maxilla. In the vertical dimension we can observe a tendency to a mesofacial pattern and a decreased vertical dimension but still within Rickett's normal values (Figure 12andTable II).
Initial and final cephalometric measurements.
| Sagittal plane | Norm | Initial | Final |
|---|---|---|---|
| ANB (Steiner) | 2° ± 2° | −2 | 0 |
| Wits (Jacobson) | 0-3 mm | −13 | −4 |
| Overjet (Bimler) | 0-8 mm | −4 | 0 |
| Convexity (Ricketts) | 0-2 mm | 1 | 3 |
| SNA (Steiner) | 82° ± 2° | 83 | 80 |
| Factor 1 (Bimler) | 0° | −1 | 0 |
| Maxillary Depth (McNamara) | 0-1 mm | 5 | 5 |
| Maxillary Depth (Ricketts) | 90° ± 3° | 95 | 92 |
| SNB (Steiner) | 80° ± 2° | 85 | 80 |
| Facial angle (Downs) | 87° ± 3° | 94 | 92 |
| 1:1 Ratio (Jarabak) | 1:1 | 66-75 | 66-69 |
| Mandibular Length (Bimler) | 99 mm | 105 mm | 100 mm |
| Vertical dimension | |||
| Bimler facial index | d/b/m | Brachifacial | Mesofacial |
| Facial Taper (Ricketts) | 68°o ± 3° | 59 | 63 |
| SN/Mandibular (Steiner) | 32° ± 3° | 39 | 35 |
| FMA (Tweed) | 25° ± 3° | 27 | 25 |
| Gonial Angle (Jarabak) | 130° ± 5° | 128 | 121 |
| Facial Axis (Ricketts) | 90° ± 5° | 90 | 90 |
| % Growth (Jarabak) | 62%-64% | 63 | 65 |
| Dental analysis | |||
| U1-AP (R.W.) | 28° ± 2° | 23 | 27 |
| L1-AP (R.W.) | 22° ± 4° | 26 | 26 |
| 1-SN (Jarabak) | 103° ± 2° | 105 | 106 |
| IMPA (Downs) | 90° ± 2° | 86 | 92 |
| Overjet (Ricketts) | 2 mm | −4 | 3 |
| Soft tissues | |||
| Nasolabial angle | 94-110° ± 3° | 91 | 95 |
| Ricketts aesthetic line | -2 ± 2 mm | −1 mm | −4 mm |
| Cervicomental distance | 50 mm | 55 mm | 47 mm |
Dentally there was an increase in the upper incisor inclination, improving the incisal display and also improving the soft tissues.
In the panoramic radiograph it may be observed that all teeth have an adequate root parallelism, without bone crest loss or pathological processes present, with the screws and surgical titanium plates in place and the performed osteotomies in a osseointegration process (Figure 13).
DISCUSSIONClass III malocclusion has been a topic of interest in many investigations, due to the challenges that its treatment involves. When a class III relationship is diagnosed after the completion of the facial growth, treatment options are more limited. Generally, fixed appliances in conjunction with dental extractions are considered to be the only option for a non-surgical approach.
Traditionally, the removal of four bicuspids would be the first choice and sometimes also the extraction of first molars. First molar extractions may be chosen instead of premolar extractions when the first molars have extensive caries, hypoplasic lesions, apical pathologies or large restorations. Other situations in which the first molars could be removed are a significant crowding in the distal portion of the mandibular arch, a high mandibular plane angle and an anterior open bite. A disadvantage of first molar extractions is the difficulty in space closure due to the fact that the lower second molars tend to incline mesially and lingually, leaving interproximal spaces and fostering a periodontal condition.1
Surgical-orthodontic treatment in class III patients comprehends a pre-surgical orthodontic treatment to decompensate the malocclusion, followed by surgery and subsequently the detailed and finishing of the occlusion. Decompensation aims to retrocline the proclined upper incisors and procline the retroinclined lower incisors to a more normal axial inclination. This procedure increases the severity of the Class III dental malocclusion and often results in a gradually less pleasant facial profile. The preoperative dental decompensation dictates the magnitude and type of surgical change and is an important factor for treatment success. The lack of optimal dental decompensation compromises the quality and quantity of the correction.3
The intraoral vertical osteotomy of the mandibular ramus is a simple technique with some advantages, including a shorter surgical time, less risk of damage to the inferior alveolar nerve and a more favorable effect over the temporomandibular joint. Orthognathic surgery with vertical osteotomy produces changes in the bony and soft tissues of the maxillofacial region, including the tongue and hyoid bone positions.9
Chris Johnston et al in a study performed in class III patients measured lateral headfilms before and after orthognathic surgery and concluded that orthodontic and surgical treatment were extremely successful in the correction of the overjet to an ideal range. Although the AP skeletal correction (ANB) was less successful than the correction of overjet, the majority of the patients ended up with their soft tissue profiles within normal values. Bimaxillary surgery was performed in 75% of the patients. However, bimaxillary surgery was 3.4 times more likely to fully correct the ANB angulation than just performing mandibular surgery.1
Stability has been a very important factor in orthodontic treatments and even more in surgical -orthodontic treatments. Since the factor that caused the malocclusion was a skeletal one, there may be some relapse due to residual growth. In the case hereby presented, retention was bimaxillary to reduce the risk of relapse.
Gundega Jakobsone et al. in a three-year follow-up study in class III patients who were treated with bimaxillary surgery concluded that there was good occlusal stability in all patients. Skeletal stability varied depending on the direction and amount of surgical movements. Relapse occurred in the first six months after the surgery but in spite of it, a dentoalveolar compensation took place thanks to a good occlusal stability.4
Nobuo Takeshita et al. as a result of a complete assessment before, during and after a surgical-orthodontic treatment in a class III patient with asymmetry and mandibular condylar displacement, concluded that Orthodontics with orthognathic surgery might improve the functions of the stomatognathic system, including masticatory muscles activity, condylar movement, and occlusal force. In addition, with coronal and sagittal magnetic resonance imaging they were able to assess the 3-dimensional position of the TMJ disk and it was demonstrated that although the disk displacement was not corrected, there was no worsening of these displacement after surgery.11,12
The self-esteem factor was one of the most important of treatment, since it was a skeletal problem that was facially reflected in the patient, it was a major reason for consultation. Thus it was considered a factor for performing orthognathic surgery to correct and improve the patient¿s facial appearance.
Elizabeth Meade et al. studied 318 patients who underwent orthognathic surgeries. The patients and their parents were asked to fill a questionnaire asking how they felt before (during pre-surgical orthodontic treatment) and after the surgery, and came to the conclusion that the patients who were more excited before surgery and who remembered how they looked before surgery were the most satisfied with the treatment results. The authors also found that parents who perceived their children more excited and who focused more on the possible identities that they might acquire at the end of the pre-surgical treatment were the most satisfied.13
CONCLUSIONSSkeletal class III malocclusion may be corrected in several ways, but in the end the treatment plan must be focused on the problems faced by the patient and from that starting point, set the ideal treatment plan and then, the alternative treatment.
Triple orthognathic surgery combined with orthodontic treatment is an excellent option for the correction of skeletal class III malocclusions since it corrects the skeletal and dental problems of the patient without the need for compensatory orthodontic treatments that could lead to the loss of some dental organ or to the instability of the treatment outcome.
At the end of the day, a straightforward correction of the problem will allow an improvement both in the soft tissues and in the occlusal and dental position of the patient, all of them important objectives in our treatments.
This article can be read in its full version in the following page: http://www.medigraphic.com/ortodoncia