Dentomaxillofacial deformities are conditions that lead to a disharmony between the maxilla and mandible seriously affecting facial appearance and masticatory function. Sometimes the orthodontist requires the collaboration of a maxillofacial surgeon specially. Ever since interventions and osteotomies became more complex an interdisciplinary relationship was established between both specialties. This case report presents a 13-year-old patient with a skeletal class III accompanied by maxillary hypoplasia and mandibular anterior displacement causing an anterior and posterior crossbite. Presurgical orthodontics was performed with 0.022” slot Roth appliances. Once the arches were coordinated, the patient was refered for a surgical assessment. Orthognathic surgery was performed: a LeFort I maxillary advancement with a mandibular ramus segmental surgery was performed to reposition the jaw and treatment was finished with orthodontics to settle the bite. An occlusal adjustment was performed for obtaining the right mandibular movements and appliances were removed having achieved the desired objectives. It is important to make a proper diagnosis to define treatment objectives for each patient in order to improve aesthetics and function.
Las deformidades dentomaxilofaciales son condiciones que propician una desarmonía entre el maxilar y la mandíbula afectando gravemente la apariencia facial y la función masticatoria. En ocasiones requieren la colaboración del ortodoncista con el cirujano maxilofacial, a medida que las intervenciones quirúrgicas y osteotomías del macizo facial fueron más complejas se requirió una fuerte interdisciplina entre ambas especialidades. En este artículo presentamos un caso clínico de una paciente de 13 años de edad con una clase III ósea por hipoplasia maxilar acompañada de desplazamiento anterior mandibular que provoca una mordida cruzada anterior y posterior. Se utilizó ortodoncia pre-quirúrgica Roth Slot 0.022”. Una vez coordinadas las arcadas se remite a valoración quirúrgica. Se realiza la cirugía ortognática (LeFort I maxilar de avance con cirugía segmentaria de las ramas mandibulares para reposición de la mandíbula) y se termina con ortodoncia para asentar la mordida. Se realiza un ajuste oclusal para los movimientos mandibulares adecuados y se retira la aparatología logrando los objetivos planteados. Es importante realizar un adecuado diagnóstico para definir los objetivos de cada paciente para mejorar la estética y la función.
Anomalies in position, size and shape of the facial bones, especially the maxillary bones, usually appear in childhood. These are known as growth disorders and they accentuate in adolescence until the end of the growth period. Although this kind of anomalies have an important genetic base, they tend to be growth problems; in addition there are functional factors such as habits that produce teeth malposition more than skeletal discrepancies.1 Within these anomalies, mandibular prognathism is the most frequent alteration, followed by mandibular retrognathism, maxillary hypoplasia and mandibular laterognathia. All these alterations produce a disharmony in the maxilla and mandible thus causing a distortion in facial aesthetics and masticatory function.2
Class III malocclusions lack anterior guidance and might present contacts during laterality movements, group function or interferences in balance.3 The class III patient has some particular craniofacial peculiarities such as the predominance of an short anterior cranial base or a more vertical mandibular growth pattern than the average. The therapeutic approach is very varied.4 The first thing that must be decided is whether orthopedic treatment will be performed or not. In the event of not being able to do orthopedic treatment, orthognathic surgery or camouflage is usually the path to be taken. In orthopedic-orthodontic and in camouflage treatments, it is usually resorted to auxiliary appliances.5 The main objectives of the orthodontic-surgical treatment are to normalize the facial profile, occlusion and function.
When a patient is selected to receive surgical-orthodontic treatment to correct a facial disharmony, it is convenient to know that the patient must comply with certain rules in order to be treated surgically. These rules are known as the pre-surgical phase and may take up to a year and a half to be achieved:
- a)
Ideal state of oral health.
- b)
No dental retentions.
- c)
Arch coordination.
- d)
Tooth alignment.
- e)
Ideal anterior teeth angulation according to basal bone.
- f)
Curve of Spee as flat as possible.
- g)
Heavy archwires four weeks before the surgery.6
Recently, surgical-orthodontic treatment, without presurgical orthodontics or with a short period of this phase known as surgery first or SF by its initials has been suggested.7 The SF concept involves prediction and simulation of dental alignment, incisor decompensation and arch coordination. Based on this information, the decisions on the surgical movement of the maxilla and the mandible can be performed to correct the skeletal discrepancy. SF offers several advantages including improving early the facial profile and symmetry, the establishment of a normal intermaxillary relationship before orthodontic alignment, a shorter total treatment time and a more efficient decompensation.8
Maxillofacial surgeons and orthodontists should discuss with young patients and their parents the importance of patient's motivation during the initial consultation before starting treatment in order to assess the patient's commitment and expectations and satisfying the patient without generating false hopes.9
CASE REPORTA female patient, 13 years of age, is hereby presented. She was diagnosed with maxillary retrusion, mandibular prognathism and brachifacial growth, which had been previously treated with orthopaedic treatment. The patient said that orthopedic therapy was started two years prior to our treatment plan and did not produce favorable results, so it was decided to consider a SF protocol. Fixed appliances were placed to correct the crowding and coordinate the arches in the transverse dimension. A mandibular retroposition and elevation was performed, combined with a LeFort I and height reduction of the maxilla. Subsequently, orthodontic treatment was applied for finishing and detailing. A significant decrease of the hard tissues of the lower third, of the mandibular length and in facial depth was achieved.
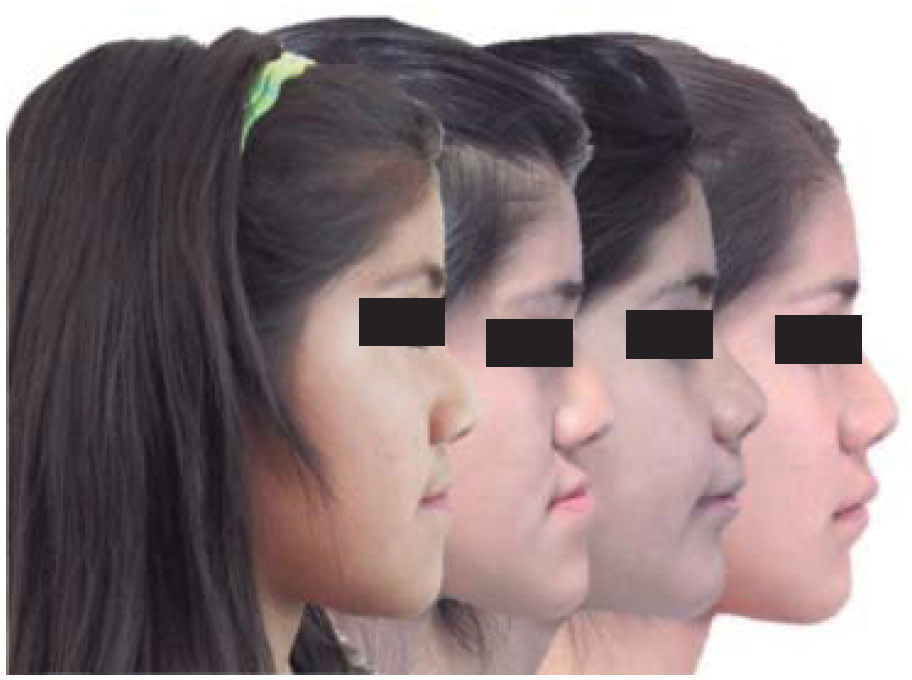
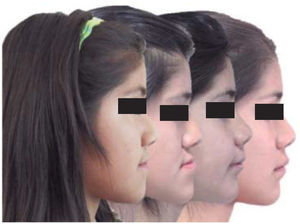
At the initial frontal view, facial symmetry was observed with an increased lower facial third. The cheekbones were slightly marked since the malar bones did not highlight the middle third, a typical feature of class III patients. The smile line was normal. The profile showed a concave shape. The chin was slightly prominent; the nasolabial and mentolabial angle were decreased. The upper lip was slightly retruded (Figure 1).
During the initial interrogation, the patient revealed a shy, withdrawn behavior. The mother commented on having observed depression in her daughter, saying that the patient did not want to go to the school because she was teased at due to her facial appearance.
Upon the intraoral clinical examination the upper arch showed a parabolic shape and slight curve of Spee. The upper basal bone was favorable. The upper first molars were rotated. The mandibular arch had a parabolic shape and a flat curve of Spee. There were mild rotations. The overjet was -11mm.
Occlusal relationships: bilateral molar and premolar class III, with an inverted overjet; overbite was increased by 2mm. Cross bite of the upper incisors and left and right premolars, with cusp to cusp relationship on the left side. The lower dental midline was deviated 2mm to the right. The canine class was not assessable since the deciduous canine (63) was present but with a notable tendency to class III.
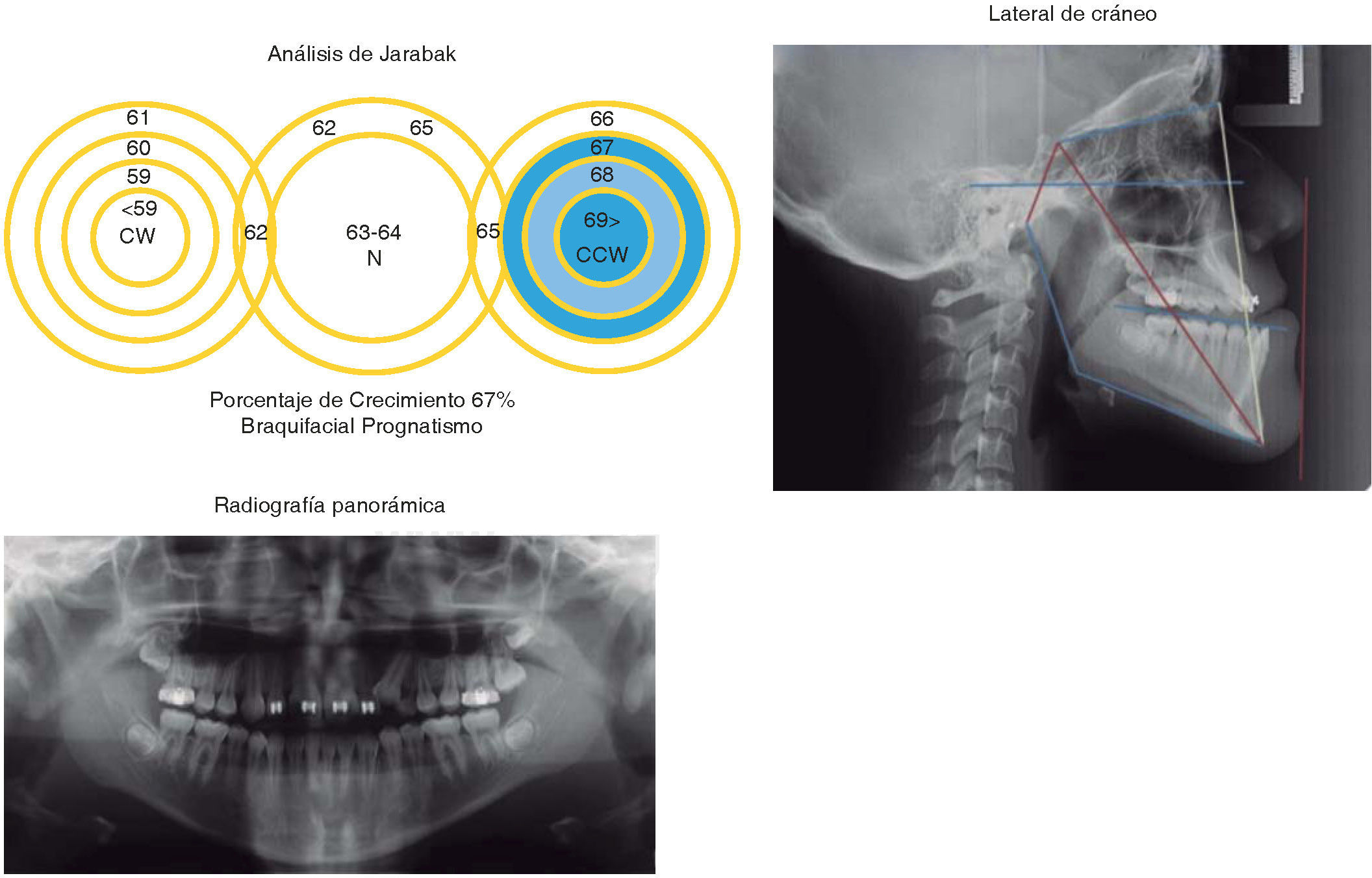
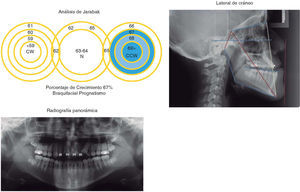
In the orthopantomography presence of 26 permanent teeth was observed; tooth number 63 had not been exfoliated since the canine was supraerupted, the upper and lower third molars as well as the seconds upper molars had not erupted; the condyles were asymmetric as were the maxillary sinuses; the alveolar processes were continuous without observed any intraosseous pathology (Figure 2).
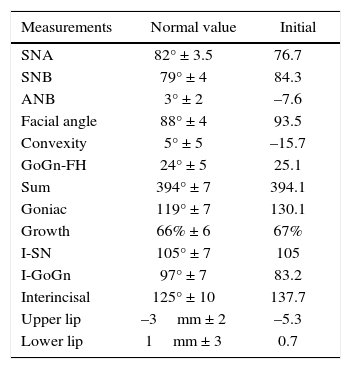
Cephalometric data revealed a skeletal class III patient due to a lack of maxillary growth and prognathism, with a brachifacial pattern in most of the cephalometric analysis, a horizontal growth tendency, upper incisor proclination and lower retroclination (Table I).
UNAM analysis.
| Measurements | Normal value | Initial |
|---|---|---|
| SNA | 82° ± 3.5 | 76.7 |
| SNB | 79° ± 4 | 84.3 |
| ANB | 3° ± 2 | –7.6 |
| Facial angle | 88° ± 4 | 93.5 |
| Convexity | 5° ± 5 | –15.7 |
| GoGn-FH | 24° ± 5 | 25.1 |
| Sum | 394° ± 7 | 394.1 |
| Goniac | 119° ± 7 | 130.1 |
| Growth | 66% ± 6 | 67% |
| I-SN | 105° ± 7 | 105 |
| I-GoGn | 97° ± 7 | 83.2 |
| Interincisal | 125° ± 10 | 137.7 |
| Upper lip | –3mm ± 2 | –5.3 |
| Lower lip | 1mm ± 3 | 0.7 |
In summary, we faced a retrusive maxillary and prognathic mandible class III with horizontal growth.
Treatment goalsThe goals of treatment were: to correct the facial profile, obtain molar and canine class I, eliminate the crowding, match the dental midlines, correct the inclination of the upper incisors and correct the skeletal discrepancy by means of orthognathic surgery.
RESULTSThe complete treatment lasted eleven months.
- •
Presurgical phase
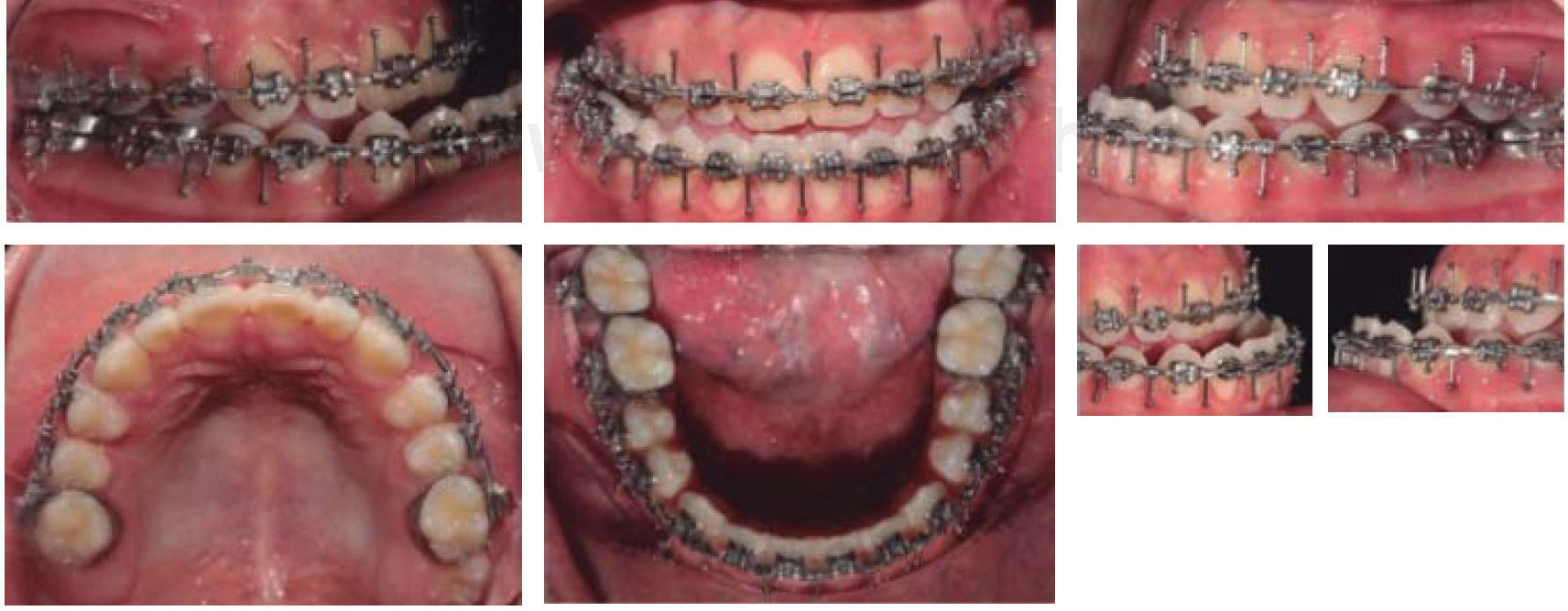
Roth appliances were placed with 0.022” slot (GAC) bands in molars with upper and lower 0.016” x 0.16” NiTi archwires. After two months, bands were placed in second molars with 0.016” x 0.022” NiTi archwires. The upper left cuspid was pulled down with individual ligature and elastic thread until it reached the arch.
Once the canine was in position, upper and lower 0.017” x 0.025” NiTi archwires were placed to make movements of tipping and individual torque. Once this stage was concluded, upper and lower 0.017” x 0.25” stainless steel archwires were placed to flatten completely the curve of Spee and improve the inclination of the upper arch.
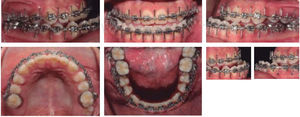
An assessment was made and it was concluded to place crimpable hooks between each bracket (surgical archwires) in order to refer the patient to surgery. This phase lasted only 5 months (Figure 3).
- •
Surgical phase
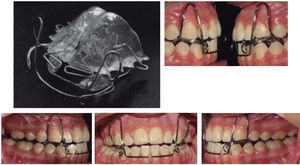
The patient was referred to the Maxillofacial Surgery Department for assessment and treatment. A bimaxillary surgery was performed through sagittal mandibular retroposition and elevation combined with a LeFort I surgery and maxillary impaction. Fixation was achieved only with elastics (Figure 4).
- •
Postsurgical phase
3/16” 3.5 oz. class III and anterior box elastics were placed. Brackets of teeth number 23, 24 and 25 were repositioned to achieve contact points between arches.
Occlusal stops were placed in the molars to correct the cross bite of the upper right molar combined with 3/16” 3.5 oz. crossed elastics and settling elastics with a class III triangular vector on the right side and class II on the left side. Box elastics were continued in the four lateral incisors with 0.016” x 0.022” NiTi archwires for arch settling.
The use of class III elastics was continued and upper and lower 0.019” x 0.025” NiTi archwires were placed.
Microdontia of the upper lateral incisors was noted so an open coil was placed mesial and distal of teeth #12 and 22 to create space for an eventual restoration with resins or veneers.
Finally an occlusal adjustment was conducted and treatment continued with 0.019” x 0.025” stainless steel archwires, upper and lower, for 3 months.
The postsurgical phase lasted 7 months (Figure 5).
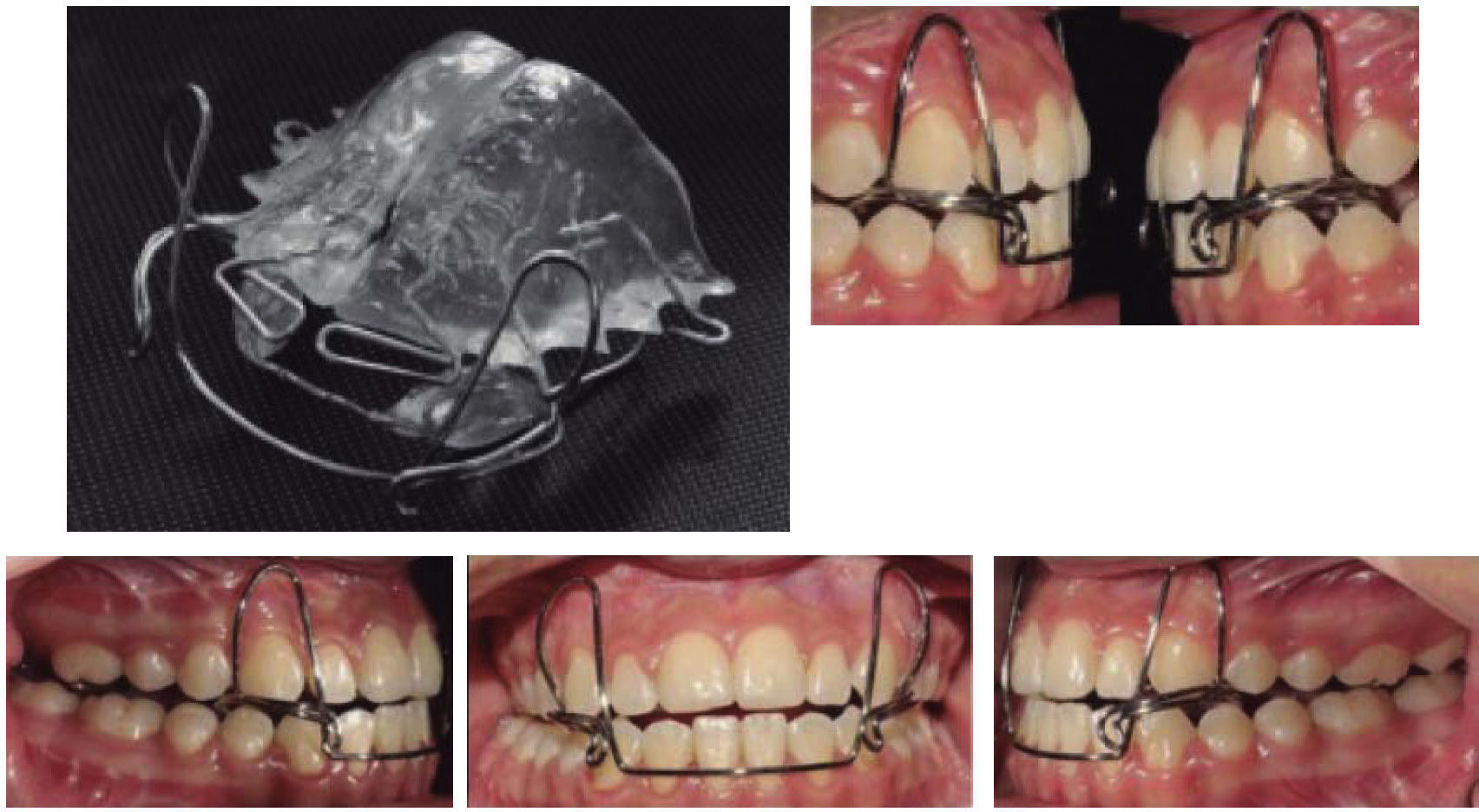
Fixed appliances were removed (Figure 6) and two types of retainers were placed: a circumferential retainer and another one to maintain the inter-arch relationship: an orthopedic appliance (Bimler class III) used by night (Figure 7).
Finally, contact resins were placed in the upper lateral incisors to improve the smile line (Figure 8).
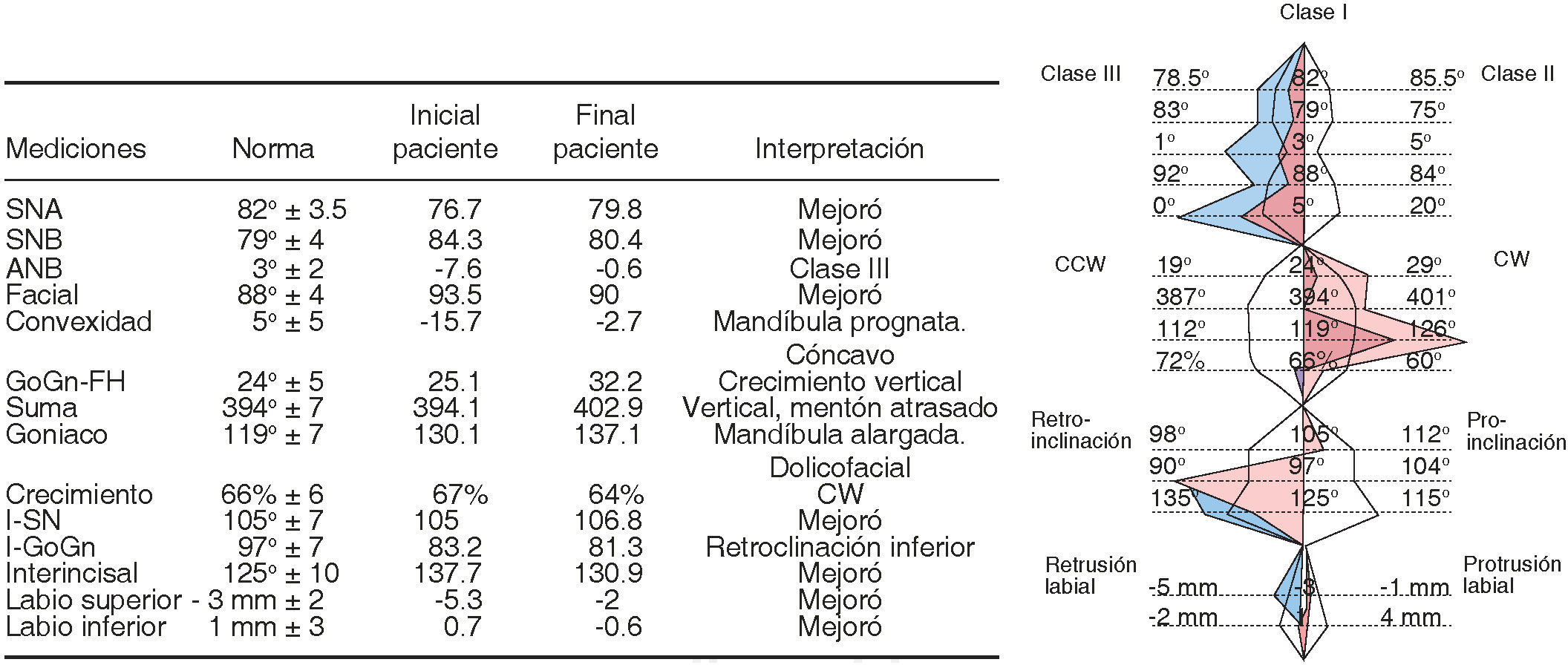
The patient finished her treatment as a mesofacial skeletal class I, although some cephalometric values such as the GoniacAngle remained vertical. The upper and lower incisor inclinations were corrected. The profile was greatly improved and both the lips and the interincisal angle achieved a good relationship. This may be due to the distal relocation of the mandible thus obtaining maximum intercuspation (molar and canine class I, matching dental midlines) and the protrusion of the lower incisors. The patient was satisfied with the results (Figure 9andTable II).
DISCUSSIONIn order to obtain successful results when treating these patients, it is essential the integration of several disciplines from the initial assessment until the conclusion of the set goals. It is necessary the integrated effort of surgeons, orthodontists, prosthetic dentists and other specialists that the case may require.10 It is imperative to have a close collaboration between all of them for orthognathic surgery to produce satisfactory facial results for each specialty and for the patient while correcting the malocclusion.11
Regarding the surgery's stability, Wen-Ching12 in 2013 came to the conclusion that chronological age does not influence long-term stability in class III patients. In patients who underwent surgery first the most important factors of instability include: the amount of overbite, a deep curve of Spee, an increased negative overjet and if there was an significant amount of mandibular setback during surgery. Furthermore, they concluded that the initial occlusion may be a very important indicator to predict relapse in the orthodontic-surgical treatment.
Composite resins are an excellent option to restore anterior teeth due to their aesthetic and mechanical properties. In addition these materials are a conservative, fast and optimal cost - benefit alternative. In addition the evolution of adhesive systems and its adhesion (mainly to enamel) makes these restorations long lasting and predictable.13
CONCLUSIONSThe maxillofacial surgeon should understand the treatment plan from the orthodontics point of view and the orthodontist should be able to identify the objectives of the pre-surgical orthodontic treatment and know the limitations of orthognathic surgery. Satisfactory results depend on a good diagnosis and treatment plan of the dentofacial deformity as well as a good integration of knowledge between the involved professionals, otherwise errors in the planning of the case may interfere with the expected success and lead to frustration, both of the patient and the staff in charge.9 It is important to follow a logical sequence, determined by each analysis carried out in all the stages of a long road that finally leads to achieving functional, aesthetic and psychological rehabilitation for these patients.
This article can be read in its full version in the following page: http://www.medigraphic.com/ortodoncia