A case report of a 19-year-old female patient who attended the Orthodontics Department, Faculty of Dentistry, National Autonomous University of Mexico without any apparent pathological data is hereby presented. Upon interrogation, the patient referred to have had a previous surgical replacement of the left ear lobe. Physical examination revealed a severe facial asymmetry with mandibular deviation to the left side, straight profile, upper lip retrusion and gibbous nose. Intraorally the patient showed crowding, non-coincident dental midlines, squared arches and class III molar and canine relationship with left crossbite. Radiographically all dental organs were present and mandibular asymmetry could be observed. Cephalometric analysis showed skeletal a class III due to maxillary retrusion, vertical growth pattern, left laterognathia, proclination of upper incisors and upper lip retrusion. Treatment consisted of three phases: 1 presurgical orthodontics with 0.018” slot Alexander appliances and an archwire sequence suitable to the problem that the patient presented. Subsequently, surgical phase 2 was initiated with a sagittal osteotomy for bilateral laterognathia correction. During phase 3, postsurgical orthodontics, the case was detailed, muscular patterns were corrected and the occlusion was settled. Treatment was completed in 36 months. The profile and facial harmony were improved, the positive smile was maintained and the crossbite corrected. Bilateral canine and molar class I was obtained, the dental midlines were centered and arch form was improved as were the overbite and overjet.
El objetivo de este caso clínico es demostrar la corrección de asimetría facial congénita. Se presenta caso clínico de paciente femenino de 19 años de edad que acude al Departamento de Ortodoncia de la Facultad de Odontología de la Universidad Nacional Autónoma de México, sin datos patológicos aparentes, con datos previos quirúrgicos de cirugía protésica de lóbulo auricular izquierdo. A la exploración física se observa asimetría facial marcada con desviación mandibular hacia el lado izquierdo, perfil recto, retroquelia superior y nariz gibosa. Intraoralmente muestra apiñamiento dental, líneas medias dentales no coincidentes, arcadas cuadradas y relación clase III molar y canina bilateral, con mordida cruzada lado izquierdo. Radiográficamente presenta todos los órganos dentarios y asimetría mandibular. El análisis cefalométrico mostró clase III esquelética por retrusión maxilar, patrón de crecimiento vertical; dolicofacial, laterognasia izquierda, proinclinación de incisivos superiores y retroquelia superior. El tratamiento consistió en tres fases: 1. Ortodoncia prequirúrgica llevada a cabo con aparatología Alexander con slot 0.018”, con una secuencia de arcos adecuada al problema que presentaba la paciente, posteriormente iniciando la fase; 2. Quirúrgica, osteotomía sagital bilateral para la corrección de laterognasia, y fase 3. Ortodoncia postquirúrgica, donde se detalló el caso, corrigiendo patrones musculares y de asentamiento oclusal. El tratamiento se terminó a 36 meses, logrando mejorar el perfil y la armonía facial, se conservó la sonrisa positiva, se eliminó la mordida cruzada, obteniendo clase I canina y molar bilateral, se centraron las líneas medias dentales, mejoró la forma de arcadas y sobremordida vertical y horizontal.
Facial asymmetries and dento-skeletal deformities are the result of the complex interaction of many factors that influence development and growth.1 They may be caused by discrepancies in size and position between cranial base and maxilla, between cranial base and mandible or between maxilla and mandible as well as the rest of the craniofacial massif.1
A deformity is the abnormal shape or posture of a body part due to non-disruptive mechanical forces. It appears during late fetal life due to mechanical forces often affecting the muscular-skeletal system. This condition may be isolated affecting only the mandible, extend to multiple craniofacial structures unilaterally or bilaterally or be expressed in the vertical, horizontal or transverse facial plane.2
Treatment for dento-skeletal deformities is performed through orthopaedics, orthodontics, orthognathic surgery or a combination of these. Approximately four per cent of the population has a dentofacial deformity that requires orthodontic- surgical treatment for its correction. The most common indications for surgical treatment are severe skeletal class II and III cases as well as vertical skeletal discrepancies in patients who are no longer in an active growth stage.2 Skeletal class III patients are a large proportion of those who seek orthodontic- surgical treatment. Proffit et al reported that 20% of surgical patients have mandibular excess, 17% have maxillary retrusion and 10% have both. Skeletal class III patients are more likely to seek a clinical evaluation than skeletal class II patients.3 The majority of patients with class III malocclusions present dentoalveolar and skeletal problems and only a minority of cases may be treated with orthodontics only. Nevertheless, patients with severe skeletal class III discrepancies are often treated with orthognathic surgery of the maxilla, mandible or both in combination with orthodontic treatment.2–4
In cases with facial asymmetries it is often intended to correct the transverse problem with orthodontics only, without success and in many of these patients relapse is common.5
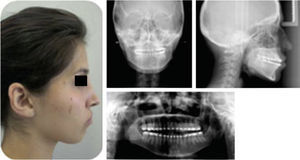
CASE PRESENTATIONA case report of a female patient of 19 years of age is hereby presented. She attended the Orthodontics Clinic at the Division of Postgraduate Studies and Research of the National Autonomous University of Mexico with the following chief concern: «I have a mandibular deviation». She denied having any medical family history of importance and referred a surgical background of a prosthetic surgery in her left ear lobe. She was considered a healthy patient.
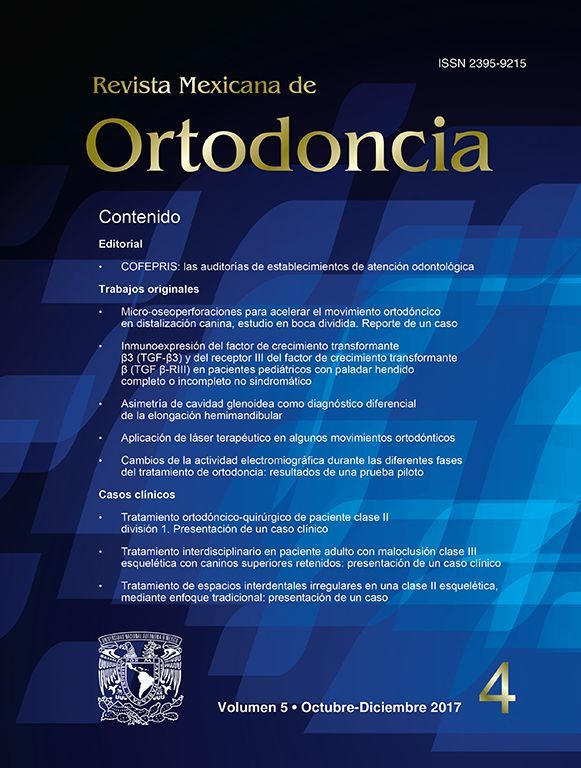
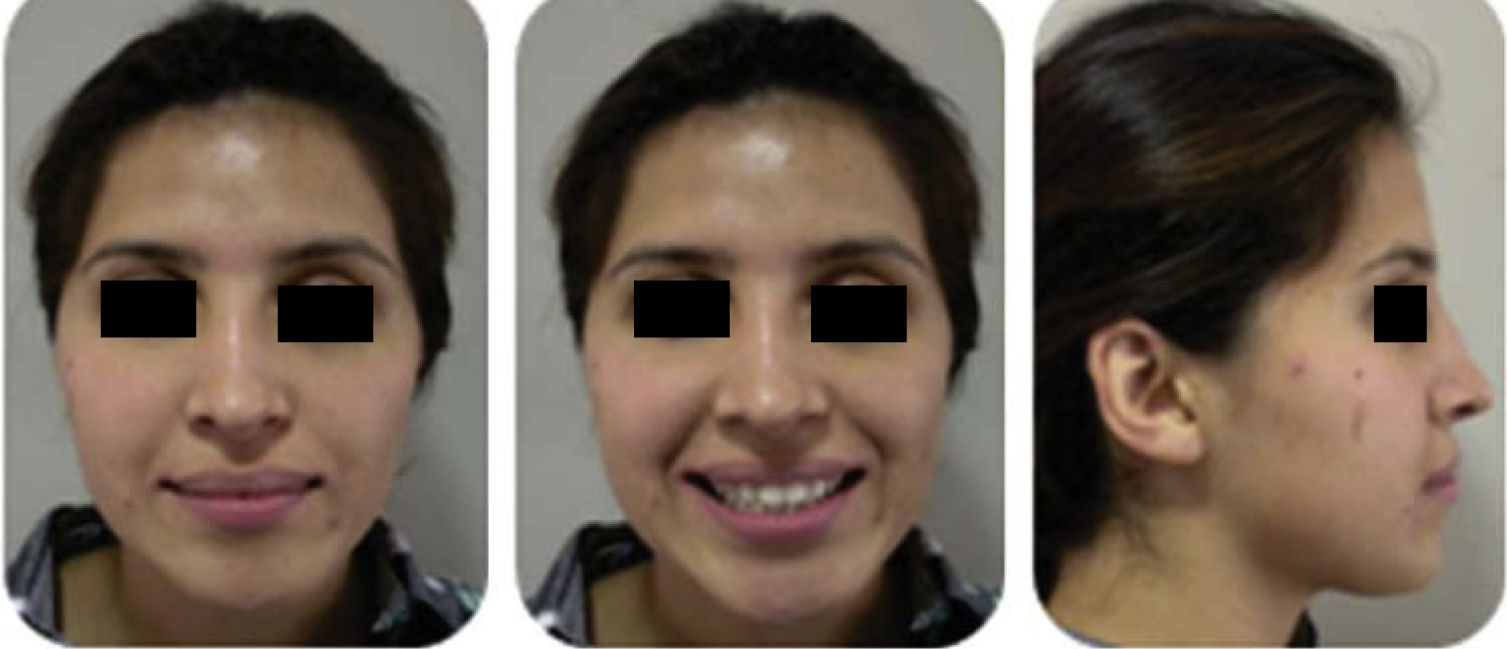
Clinical assessment:Patient with oval face, positive smile; displays 20% of the upper tooth crowns. She had a decreased lower facial third in relation to the middle third, facial asymmetry, deficient anterior projection of the facial middle third, mentalis hypertonicity, thick lips, facial midline did not match the dental and the chin was deviated to the left side.
The patient presented a straight profile, gibbous nose, lower lip protrusion, obtuse (open) nasolabial angle and lip competence (Figure 1).
Intraorally, there was dental crowding, dental rotations, non-coincident dental midlines, square- shaped arches and a bilateral class III molar and canine relationship with posterior cross bite on the left side.
Model analysis revealed a tooth-bone discrepancy of -10.5mm on the upper arch and in the lower, -5.5mm. Overbite was 3mm and overjet, 2mm (Figure 2).
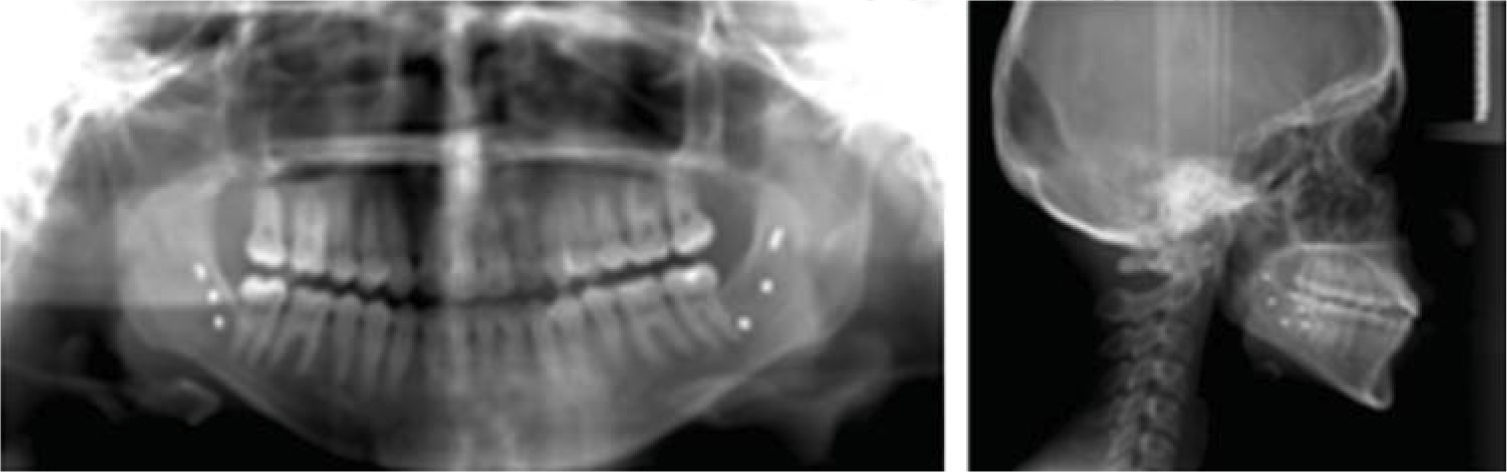
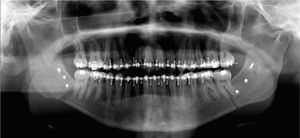
In the panoramic radiograph the presence of 32 teeth was observed, a 1:2 crown-root ratio, good bony ridge level, asymmetry of the mandibular ramus and no sign of temporomandibular joint disease (Figure 3).
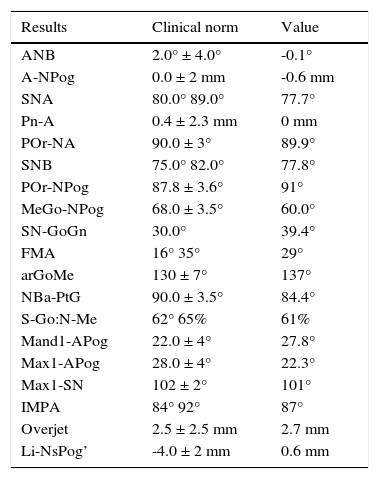
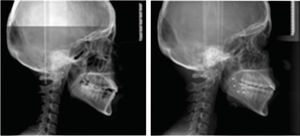
Cephalometric analysis revealed a skeletal class III malocclusion due to maxillary retrusion, a vertical growth pattern, dolichofacial biotype, left laterognathia, upper incisor proclination and upper lip retrusion (Figure 4andTable I).
Initial cephalometric values.
| Results | Clinical norm | Value |
|---|---|---|
| ANB | 2.0° ± 4.0° | -0.1° |
| A-NPog | 0.0 ± 2 mm | -0.6 mm |
| SNA | 80.0° 89.0° | 77.7° |
| Pn-A | 0.4 ± 2.3 mm | 0 mm |
| POr-NA | 90.0 ± 3° | 89.9° |
| SNB | 75.0° 82.0° | 77.8° |
| POr-NPog | 87.8 ± 3.6° | 91° |
| MeGo-NPog | 68.0 ± 3.5° | 60.0° |
| SN-GoGn | 30.0° | 39.4° |
| FMA | 16° 35° | 29° |
| arGoMe | 130 ± 7° | 137° |
| NBa-PtG | 90.0 ± 3.5° | 84.4° |
| S-Go:N-Me | 62° 65% | 61% |
| Mand1-APog | 22.0 ± 4° | 27.8° |
| Max1-APog | 28.0 ± 4° | 22.3° |
| Max1-SN | 102 ± 2° | 101° |
| IMPA | 84° 92° | 87° |
| Overjet | 2.5 ± 2.5 mm | 2.7 mm |
| Li-NsPog’ | -4.0 ± 2 mm | 0.6 mm |
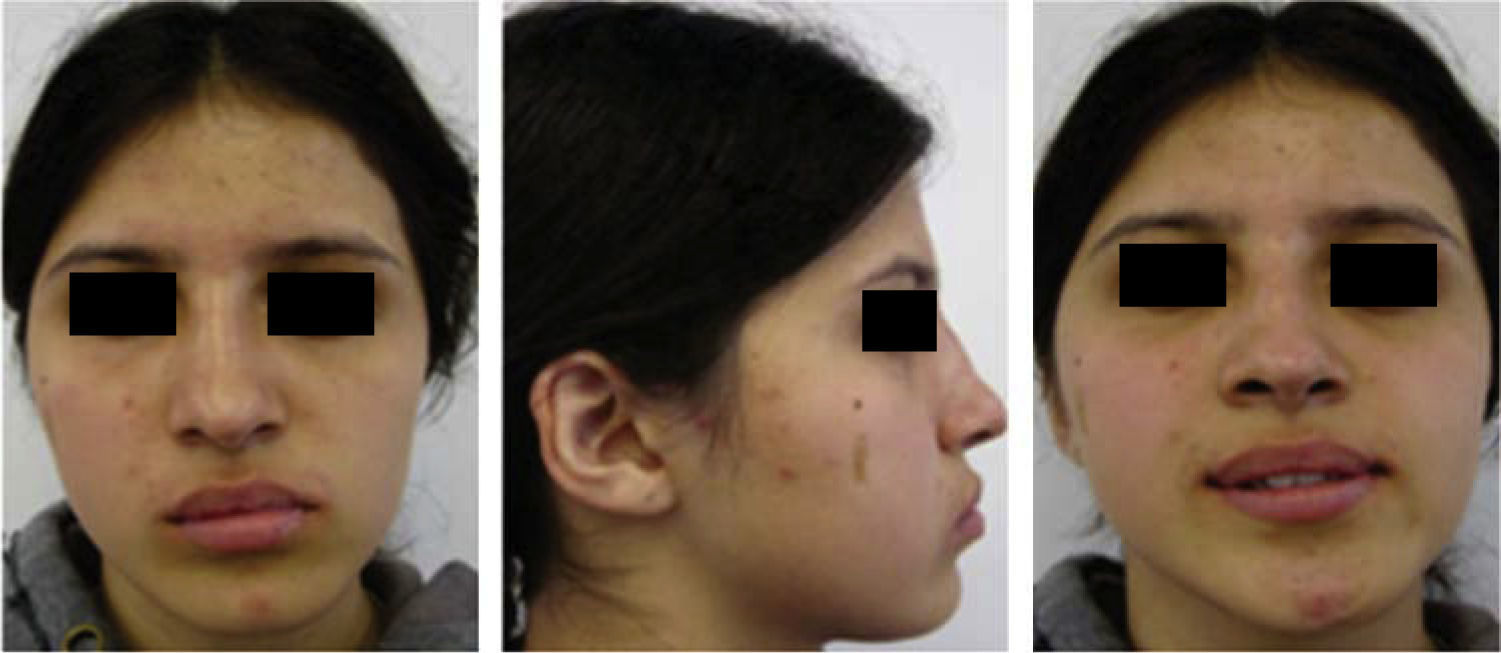
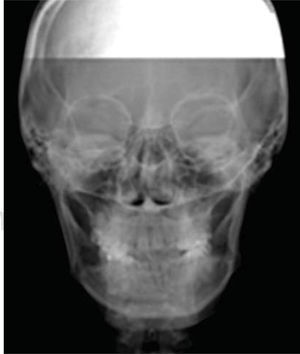
Ricketts posteroanterior cephalometric analysis revealed a mild transverse collapse of the maxilla (Figure 5).
Treatment goals consisted in correcting the facial asymmetry, improving the profile, decreasing the lower facial third, correcting the crossbite, achieve molar and canine class I, improve upper and lower dental inclination and obtain a skeletal class I.
After establishing the diagnosis and goals of treatment, the Department of Orthodontics conducted an interconsultation with the Department of Surgery of the Xoco General Hospital, in order to carry out an interdisciplinary treatment plan.
Therefore, it was suggested to the patient the extraction of the third molars and subsequently an orthodontic-surgical treatment which consisted of three phases: phase 1. Presurgical orthodontics performed with 0.018” slot Alexander appliances and an archwire sequence suited to the problem that was the patient presented. Phase 2. Surgery, a bilateral mandibular sagittal osteotomy for laterognathia correction was conducted, and phase 3. Postsurgical orthodontics, where the case was detailed, correcting muscular patterns and occlusal settlement.
Subsequent to the removal of the third molars 0.018” slot Alexander fixed appliances were placed in order to begin phase I. It was begun with 0.014” NiTi archwires in both arches to for alignment and leveling (Figure 6).
Treatment continued in the first phase, aligning and leveling, using round 0.016” NiTi archwires and afterwards, begin to express torsion movements with 0.016” x 0.022” NiTi, and 0.017” x 0.025” NiTi rectangular archwires. Two months later, the same wire calibers but of different alloy (stainless steel) were used (Figure 7).
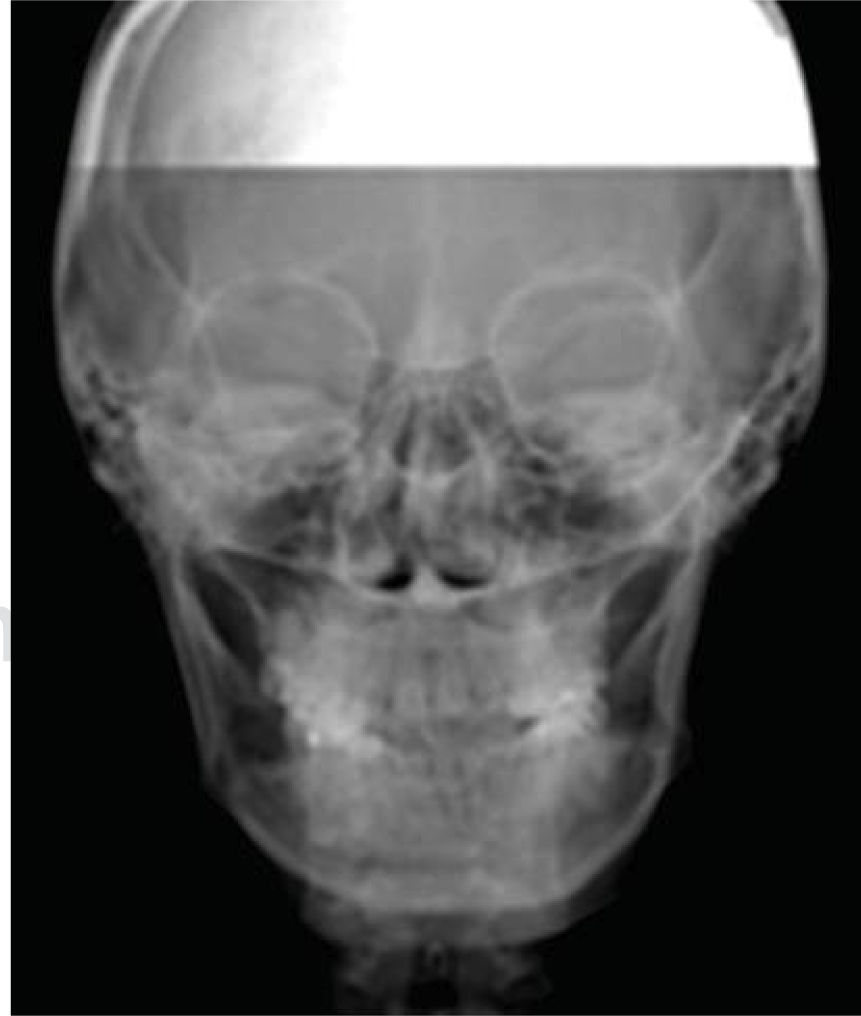
After 18 months the case was re-assessed obtaining study and work models, lateral headfilm, posteroanterior radiograph and an orthopantomography and in conjunction with the Department of Surgery at the Hospital General Xoco the orthognathic surgery was scheduled (Figure 8).
The patient was informed of the surgical risks and complications by means of a valid informed consent.
0.017” x 0.025” stainless steel surgical archwires with crimpable hooks were placed prior to the surgery.
The surgical procedure consisted in bilateral sagittal mandibular osteotomy for laterognathia correction. 8mm fixation screws were used, placing three on each side.
Seven days after surgery intermaxillary elastics were placed in order to correct a midline deviation caused possibly by muscular strength which displaced the segments of the left side. The elastics had a class II vector on the left side and a class III on the right (Figure 9).
The patient continued wearing elastics for muscular pattern correction and for occlusal settling (Figure 10).
An ortopantomography was obtained for verifying root parallelism (Figure 11).
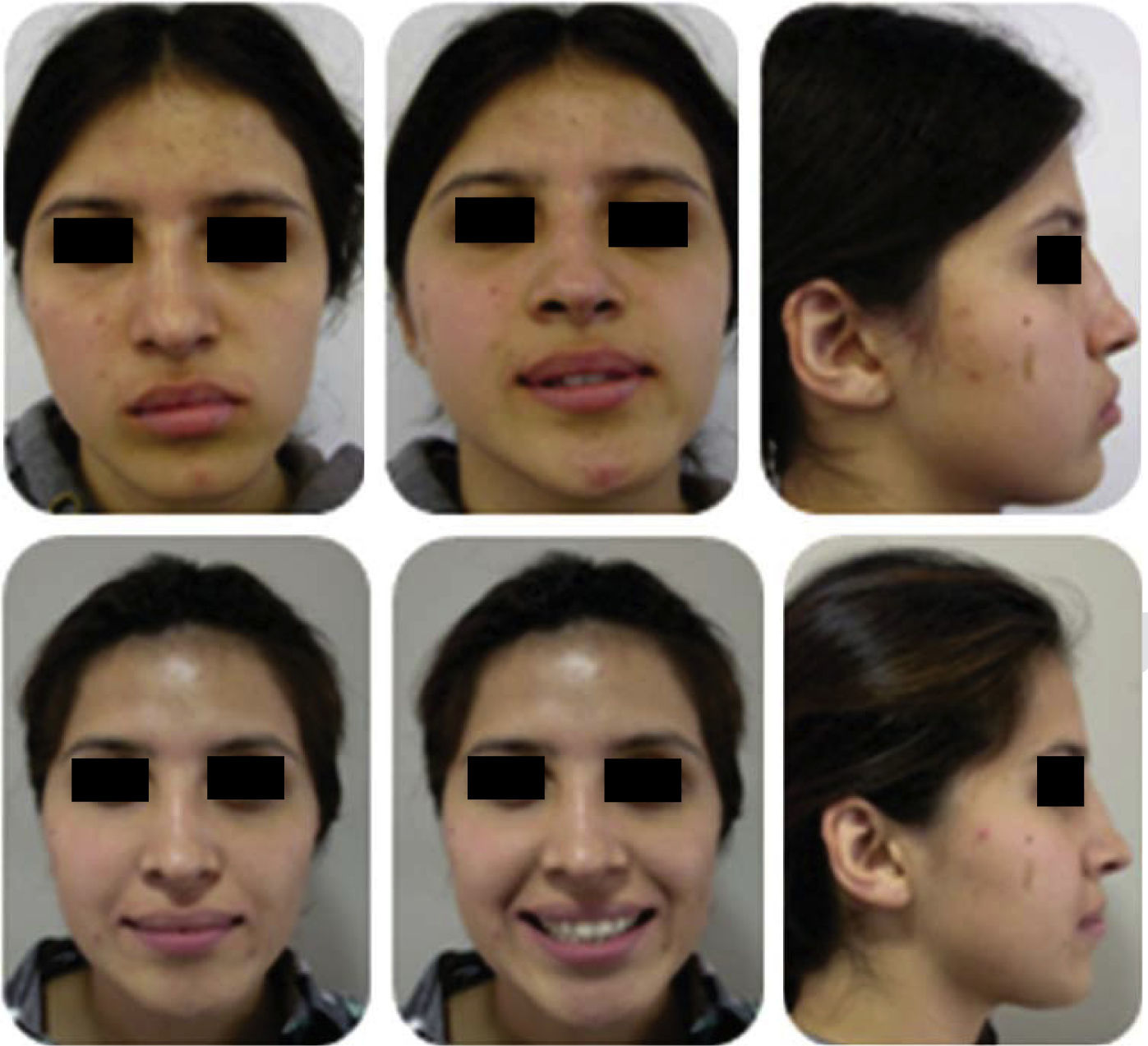
RESULTSTreatment was completed in 36 months. Facial asymmetry was achieved, the profile was improved, and a decrease in the middle third was obtained thus providing an overall improvement in facial harmony.
The smile was maintained positive (Figure 12).
The crossbite was corrected thus leaving a stable occlusion. Bilateral canine and molar class I was obtained. The dental midlines were corrected and there arch form was improved as well as the overbite and overjet (Figure 13).
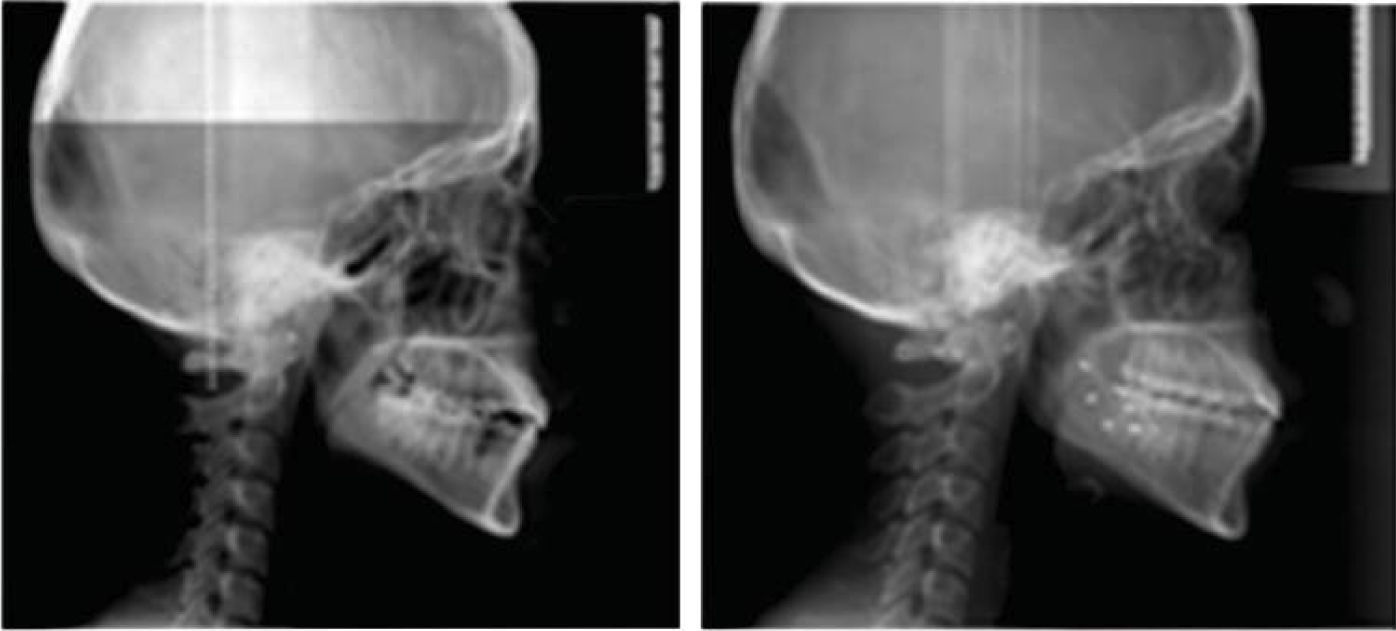
Dental inclinations were improved and root parallelism was achieved, as also the skeletal class I (Figure 14).
A bimaxillary retainer was placed with the aim of improving occlusal settlement and control muscle strength. After three months a final occlusal adjustment was performed (Figure 15).
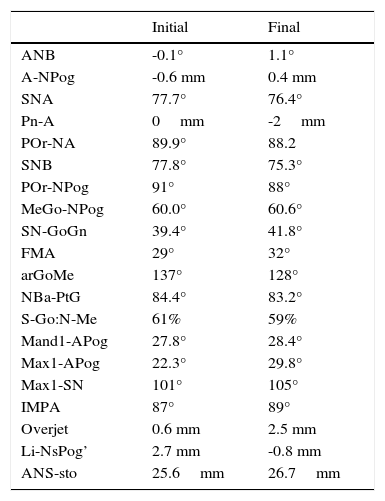
The obtained facial changes may be observed in figure 16. The occlusal changes are illustrated in Figure 17 and the radiographic ones in figure 18. Table II shows the cephalometric changes.
Initial and final cephalometric values.
| Initial | Final | |
|---|---|---|
| ANB | -0.1° | 1.1° |
| A-NPog | -0.6 mm | 0.4 mm |
| SNA | 77.7° | 76.4° |
| Pn-A | 0mm | -2mm |
| POr-NA | 89.9° | 88.2 |
| SNB | 77.8° | 75.3° |
| POr-NPog | 91° | 88° |
| MeGo-NPog | 60.0° | 60.6° |
| SN-GoGn | 39.4° | 41.8° |
| FMA | 29° | 32° |
| arGoMe | 137° | 128° |
| NBa-PtG | 84.4° | 83.2° |
| S-Go:N-Me | 61% | 59% |
| Mand1-APog | 27.8° | 28.4° |
| Max1-APog | 22.3° | 29.8° |
| Max1-SN | 101° | 105° |
| IMPA | 87° | 89° |
| Overjet | 0.6 mm | 2.5 mm |
| Li-NsPog’ | 2.7 mm | -0.8 mm |
| ANS-sto | 25.6mm | 26.7mm |
All faces have slight asymmetries which must be considered in all three dimensions of space. In this case, the asymmetry included the mandible with a severe inclination of the occlusal plane.6,7
When preparing of these cases, it must be take into consideration both the anterior and the posterior inclination of the plane, along with that of the mandibular ridge.8
The mandible on the left side by rotating in a posterior direction, required a significant amount of advance to achieve its centering and extremely rigid fixation was used.
A good bony support was achieved thus producing a better appearance of the soft tissues and a symmetrical face. Facial assessment and the knowledge of the impacts that surgical changes may produce in the mandible when moving it horizontally are the key to improving facial balance and harmony.
CONCLUSIONFacial and dental asymmetries are a difficult problem to treat which makes a comprehensive diagnosis based on precise and detailed information necessary. The facial asymmetries are diagnosed with more easily if we continue appropriate evaluation protocols craniofacial and dental, and whether it makes use correct of the different aids available diagnostic.
The facial asymmetries play an important role in the orthodontic treatments, before starting you must have a precise diagnosis helping all the tools that we have at the moment. Planning in the orthodontic-surgical treatments must be carried out in an interdisciplinary way from diagnosis. The cooperation of the patient is essential. Whatever the dentofacial deformity, there should be a protocol of individualized attention, by listing in order of importance the needs of patients in order to resolve them in a timely manner in the required order.
This article can be read in its full version in the following page: http://www.medigraphic.com/ortodoncia.
Graduated from the Orthodontics Department at the Division of Postgraduate Studies and Research of the Faculty of Dentistry, UNAM.