10-year-old female patient who was treated at the orthodontics clinic of the Autonomous University of Guadalajara showed a skeletal class II due to mandibular retrusion and a dental anterior open bite. Diagnosis was established with the aid of complete orthodontic records. The treatment plan consisted in performing rapid maxillary expansion with a Hyrax followed by a 5-month retention period. During this time, 0.022” MBT fixed appliances were placed in the lower arch and afterwards, in the upper arch. Treatment required upper first premolar extractions to reduce the overjet. Treatment objectives were to achieve canine class I, functional molar class II, normal overjet and overbite and to eliminate crowding. It was concluded that even though the results were favorable, a surgical option would have provided a better facial profile, as well as an adequate overjet and overbite.
Paciente femenino de 10 años de edad, tratado en la clínica de ortodoncia de la Universidad Autónoma de Guadalajara. El paciente mostraba una clase II esqueletal debido a una retrusión mandibular y una mordida abierta anterior dental. El diagnóstico fue determinado mediante estudios de gabinete completos. El plan de tratamiento consistió en realizar expansión rápida palatina con Hyrax; seguido de un periodo de cinco meses de retención transversal. Se cementó aparatología fija MBT 0.022” en diferentes tiempos. El tratamiento requirió extracciones de primeros premolares para reducir el overjet. Los objetivos de tratamiento fueron obtener clase I canina, clase II molar funcional, overjet y overbite adecuados y eliminar el apiñamiento. Concluimos que aunque los resultados fueron favorables, la opción quirúrgica hubiera proporcionado un mejor perfil facial, así como un apropiado overjet y overbite.
Proffit defines overbite as the overlap of the incisors in which the incisal edges of the lower teeth are in contact with the incisal and middle thirds of the palatal surface of the upper incisors, slightly below the cingulum. In open bites, vertical overlap does not occur.1 This condition may occur in a single tooth or in a group of teeth.2 Its severity varies from an almost edge to edge relationship up to a severe open bite.3 Open bite incidence varies depending on age and ethnic group being more common in African and Afro-Caribbean populations.4
Although the majority of patients with anterior open bite seek treatment only for aesthetic reasons, several problems may occur such as lack of anterior and canine guidance, difficulty for tearing food, language problems (lisp) and temporomandibular disorders among others.2,4,5
Anterior open bite may be divided into two categories:
- •
Dental open bite: the vertical skeletal pattern does not contribute to the malocclusion and is usually present in the anterior region, from canine to canine; the maxillary incisors are protruded and proclined and commonly results from a habit.
- •
Skeletal open bite: the skeletal pattern does have an influence in the malocclusion and is characterized by an elongation of the lower third of the face, rotation of the mandible in a clockwise direction, a hyperdivergent growth pattern and occlusal contacts only in molars.2,3,6
Development of anterior open bite is the result of the interaction of several factors such as: skeletal disharmonies in which an excessive vertical grow this present, lack of muscular balance, habits such as digital sucking, abnormal function of the tongue, airway obstruction or iatrogenic treatments.3,5–7
The majority of orthodontists are consistent with the fact that anterior open bite is one of the most difficult malocclusions to treat and the one with the largest percentage of relapse even when the patient is treated with orthognathic surgery. Identifying the etiology of the problem provides a greater percentage of success at the end of treatment.2,5,7–11
The literature describes different treatment modalities with the purpose of reducing relapse including miofunctional appliances, fixed appliances, lingual cribs, elastics, wires, molar intrusion, extrusion of the upper anterior teeth, aligners with elastics, orthognathic surgery, extractions, partial glossectomy or orofacial miofunctional therapy.10,11
Mizrahi described four alternatives: miofunctional therapy, orthodontic treatment with fixed or removable appliances, surgical treatment or a combination of the abovementioned.12
For Ngan, by using simple techniques in which the etiologic factors are eliminated the bite is closed through the normal eruptive process.6
Lopez-Gavito reported that more than 35 per cent of anterior open bites treated with conventional appliances relapsed 3mm or more at 10 years post-retention.13
Phelan et al found favorable effects in patients who underwent maxillary expansion and in whom a high-pull chincap was used at the peak of mandibular growth. They also recommended not perform treatment in early stages since it was best to wait until the pubertal stage.4
Pearson reported that the use of a chincap may reduce the mandibular plane angle and that this decrease prevents an increase in facial height and an over-eruption of the posterior teeth but that low reliability rates were presented.14,15
Various researchers conclude that tongue position and activity are the reasons why it is difficult to achieve long-term stability. It has been found that orofacial miofunctional therapy combined with orthodontics significantly reduces the possibility of relapse.5,10
Justus suggests modifying tongue position through the use of spurs due to the fact that patients with open bite most of the time rest the tongue over the incisors. In his research Dr. Justus found that spurs are an excellent choice for both bite closure and stability.5
CASE REPORTDiagnosis and treatment planA female patient of 10 years of age attended the Orthodontics Clinic at the Faculty of Odontology of the Autonomous University of Guadalajara referring as reason for consultation that her teeth were protruded.
Upon facial analysis, the patient showed a normofacial biotype with the facial middle third slightly increased; mouth width coincident with the inter-iris line, nasal width does not match the external edge of the eye, full lips; lip competence achieved through tension of the mentalis muscle, dental midline matches the facial midline and amedium smile. Convex profile, acute nasolabial angle, protrusive upper lip and an open mentolabial angle, as well as a decreased cervico-mental distance (Figure 1).
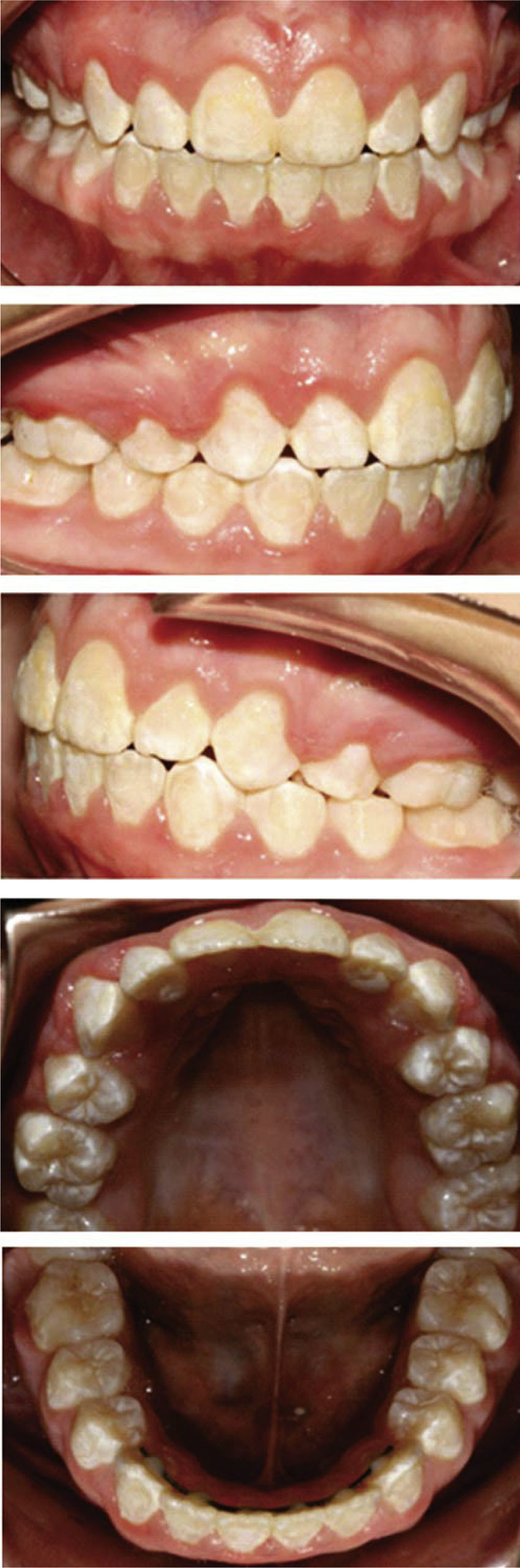
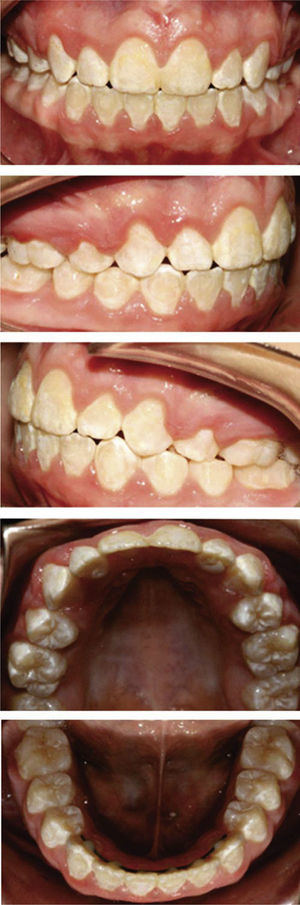
Upon intraoral examination, an anterior open bite from canine to canine was observed as well as the lower dental midline deviated with regard to the upper 3mm to the right, 4mm overjet and -1mm overbite, class II molar relationship and canine class II, a triangular shaped upper arch with moderate crowding and an ovoid lower arch with mild crowding in the anterior region; the upper and lower second molars had not erupted yet and the curve of Spee was 0.5mm (Figure 2).
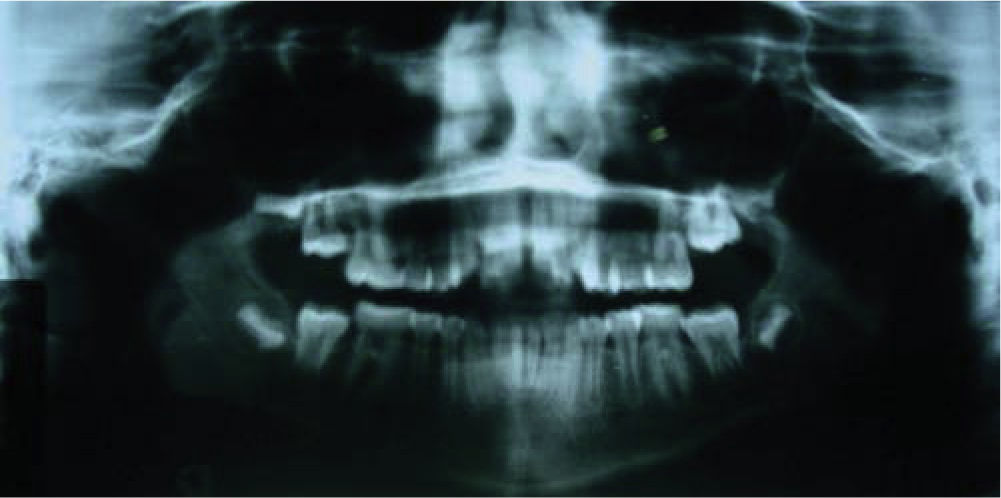
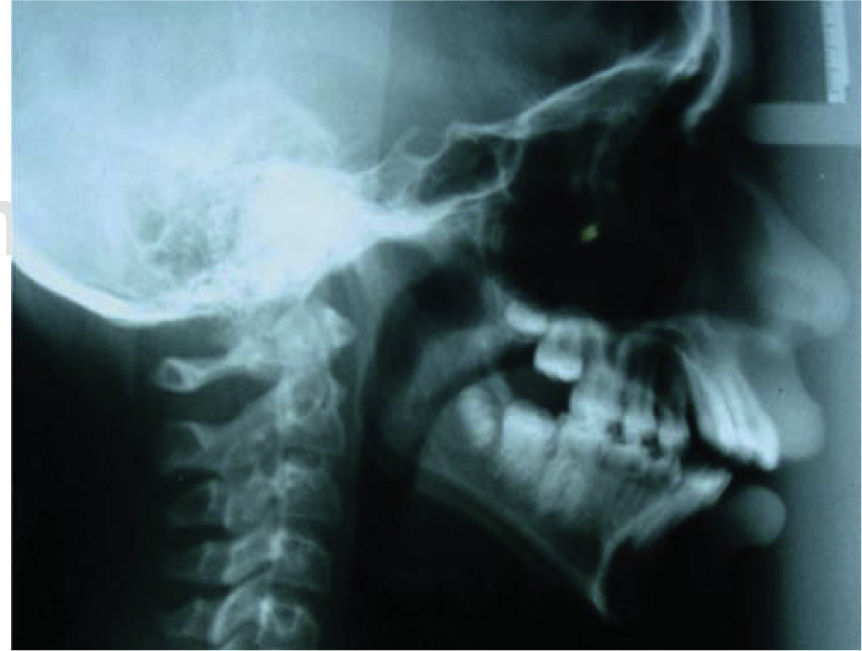
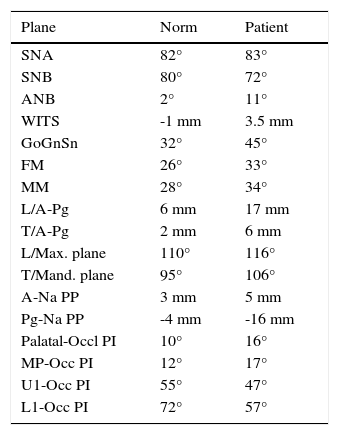
Radiographically, the panoramic radiograph evidenced the presence of second molars and germs of the third molars as well as adequate root lengths. On the lateral headfilm the Mcla1ughlin cephalometric analysis was performed (Table I) which allowed to diagnose a skeletal class II due to mandibular retrusion and a vertical growth pattern as well as dental proclination (Figures 3 and 4).
McLaughlin cephalometric tracing's values.
| Plane | Norm | Patient |
|---|---|---|
| SNA | 82° | 83° |
| SNB | 80° | 72° |
| ANB | 2° | 11° |
| WITS | -1 mm | 3.5 mm |
| GoGnSn | 32° | 45° |
| FM | 26° | 33° |
| MM | 28° | 34° |
| L/A-Pg | 6 mm | 17 mm |
| T/A-Pg | 2 mm | 6 mm |
| L/Max. plane | 110° | 116° |
| T/Mand. plane | 95° | 106° |
| A-Na PP | 3 mm | 5 mm |
| Pg-Na PP | -4 mm | -16 mm |
| Palatal-Occl PI | 10° | 16° |
| MP-Occ PI | 12° | 17° |
| U1-Occ PI | 55° | 47° |
| L1-Occ PI | 72° | 57° |
Based on her facial, dental and skeletal characteristics the patient was classified as class II.
Treatment goalsThe goals of treatment were: to eliminate crowding, achieve functional molar class II, canine class I, to correct the anterior open bite as well as the dental midlines and to obtain a normal overbite and overjet.
Treatment planTreatment plan consisted in placing a Hyrax device for a protocol of rapid palatal expansion (1/4 turn every 12hours) followed by a 5-monthperiod of transverse retention using the same Hyrax passively. Placement of 0.022” MBT fixed appliances was planned for the lower arch. After five months of retention upper first premolars extraction was planned as well as placement of upper fixed appliances space closure, occlusion detailing and retention.
Alternative treatment plansThe first alternative treatment due to the patient's facial and skeletal features was a mandibular propeller since in growing patients it helps growth redirection. Its effect over the lower incisors made us discard this option since the patient presented lower incisor proclination, a condition that is exacerbated by mandibular propellers.
Molar distalization was envisaged as an option to correct the molar class, but considering that upper molar distalization produces molar extrusion and increases mandibular hyperdivergency thus producing an open anterior bite, it was preferred not to do so because the patient had a vertical facial tendency.
Surgical-orthodontic treatment was also considered since it would improve the patient's facial overall appearance but the patient's age was not ideal for this option.
Treatment progressTreatment was initiated with the placement of a Hyrax-type screw to perform rapid palatal expansion. Once the desired expansion was achieved, the screw was closed and left as transverse retention for five months (Figure 5).
Two months after the screw was placed, 0.022” MBT lower fixed appliances were bonded. At the end of the transverse retention period, the patient was sent to the surgery clinic for upper first premolar extractions then upper fixed appliances were placed and the alignment and leveling stage was performed with the archwire sequence prescribed by the technique.
Once the leveling phase was completed, in-mass retraction of the six anterior teeth was begun with 0.019” x 0.025” stainless steel archwires and active tie-backs (Figure 6). During space closure 3.5 Oz 3/16” left class III and right class II intermaxillary elastics were used. Once the spaces were closed apanoramic radiograph was obtained and the brackets of teeth #32 and 42 were repositioned with the aim of obtaining root parallelism. Treatment continued with the settling phase by using a 5/16” 3½ Oz trapezium elastic in the anterior region and 0.019” x 0.025” stainless steel archwires on the upper arch and 0.017” x 0.025” braided on the lower (Figure 7).
Once occlusal settling was achieved, final records were requested and the appliances were removed. A lower fixed retainer from canine to canine was placed as well as an upper circumferential retainer.
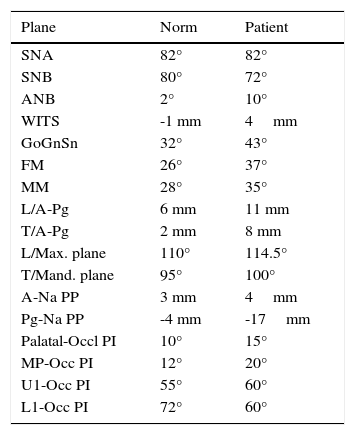
RESULTSLip competence was obtained as well as better upper lip projection, a nice smile, facial harmony. Functional molar class II, canine class I and normal overjet were achieved (Figures 8 and 9). The obtained cephalometric changes were in the dental field through a decrease in protrusion and proclination (Figure 10andTable II).
Final values of the McLaughlin cephalometric analysis.
| Plane | Norm | Patient |
|---|---|---|
| SNA | 82° | 82° |
| SNB | 80° | 72° |
| ANB | 2° | 10° |
| WITS | -1 mm | 4mm |
| GoGnSn | 32° | 43° |
| FM | 26° | 37° |
| MM | 28° | 35° |
| L/A-Pg | 6 mm | 11 mm |
| T/A-Pg | 2 mm | 8 mm |
| L/Max. plane | 110° | 114.5° |
| T/Mand. plane | 95° | 100° |
| A-Na PP | 3 mm | 4mm |
| Pg-Na PP | -4 mm | -17mm |
| Palatal-Occl PI | 10° | 15° |
| MP-Occ PI | 12° | 20° |
| U1-Occ PI | 55° | 60° |
| L1-Occ PI | 72° | 60° |
In this case report the decision to remove only in the upper arch was the best, given the characteristics that the patient presented.
We agree with Proffit in performing first premolar extractions in the upper arch and no extractions on the lower to correct class II cases since during space closure it would be difficult to control anterior retraction.1
The selection of sliding mechanics differs from that used by Denny et al; since they retracted the canine first in order to achieve class I; once this goal was accomplished incisor retraction was performed.15 In the case hereby presented an in-mass retraction from canine to canine was performed.
CONCLUSIONThe goals formulated at the beginning of treatment were met. Harmony between arches was achieved, the anterior open bite was corrected and facial esthetics was improved; but more importantly, the chief complaint of the patient was solved: to correct dental protrusion. In class II cases in whom orthognathic surgery may not be performed yet, camouflage is the best treatment option for restoring function and improving as best as possible facial aesthetics thus increasing self-confidence.
Student of the Orthodontics Specialty. Program
This article can be read in its full version in the following page: http://www.medigraphic.com/ortodoncia