Nowadays, many of the patients who seek orthodontic treatment do so in order to have a re-treatment performed because for several reasons the previous treatment did not meet the patient's expectations or the criteria and goals of contemporary orthodontics. A male patient, 20 years of age, attended the Orthodontics Department of the Faculty of Dentistry at UNAM with fixed appliances placed according to the patient approximately five years ago. Extractions of the teeth #18, 24, 28, 38, 32, 44 had already been performed as well as excessive interproximal recontouring in the tooth #25, moderate upper incisor proclination, bilateral molar class III (left side in cross-bite) left canine class III, right canine class I, teeth #22, 23 and 25 in cross bite; tooth #46 presents a severe mesial inclination; decreased overjet and overbite; gingival recessions in teeth #14, 13, 23, 24, 33, 34 and 43; poorly adjusted restorations in teeth #16, 26, 36, 46; lack of root parallelism; root resorption of tooth #21; irregular alveolar crest in the lower anterior region; fenestrations in the upper anterior segment. It was suggested to the patient an accelerated alternative treatment, which was accepted and performed in 16 months.
En la actualidad muchos de los pacientes que acuden a la consulta de ortodoncia son por un retratamiento, ya que por diversos motivos el tratamiento previo no cumplió con las expectativas del paciente o con los criterios y objetivos de la ortodoncia contemporánea. Se presenta al departamento de Ortodoncia del DEPeI de la Facultad de Odontología de la UNAM un paciente masculino de 20 años con aparatología fija colocada según refiere hace aproximadamente cinco años, con extracciones previamente realizadas de los OD 18, 24, 28, 38, 32 y 44, así como desgaste interproximal excesivo en el OD 25, proinclinación dental moderada superior, clase III molar bilateral (izquierda cruzada), clase III canina izquierda cruzada, clase I canina derecha, OD 22, 23 y 25 en mordida cruzada, el OD 46 presenta una mesioinclinación severa; ausencia de sobremordida horizontal y vertical, recesiones gingivales en los OD 14, 13, 23, 24, 33, 34 y 43, restauraciones mal ajustadas en los OD 16, 26, 36 y 46, ausencia de paralelismo radicular, reabsorción radicular del OD 21, cresta alveolar irregular en la zona anterior inferior, fenestraciones en el sector anterior superior. Se sugiere al paciente una alternativa acelerada de tratamiento, la cual es aceptada y se realiza en 16 meses.
Today many of the patients who undergo orthodontic treatment look for speed and efficiency. One of the main disadvantages of orthodontic treatment is the amount of time it takes to be completed, that remains a cause for which many potential patients do not begin treatment.
Surgically facilitated orthodontics has been used in different ways to accelerate conventional treatment; it is important to define and differentiate a corticotomy from an osteotomy; corticotomy is defined as a surgical procedure in which only cortical bone is cut, drilled or mechanically altered, while an osteotomy is defined as the surgical cut through the cortical and medullar bone. Köle first described osteotomy in 1959 as a way of moving teeth; the procedure involved full buccal, lingual and palatal flaps to expose the alveolar bone followed by interdental and subapical cuts through the full thickness of the alveolus. Köle suggested moving bony blocks (bony block movement) instead of individual teeth so that resorption would not occur and also, retention would be more stable.1
Studies have been conducted with modifications to the technique; Duker used the basic technique of Köle in beagle dogs and in relation to tooth vitality there was no damage, so that their conclusions stated that both the dental pulp as well as the periodontium were not damaged after surgery by the corticotomies. Suya reported the orthodontic treatment assisted by corticotomies of 395 Japanese adults, showing that treatments were completed between 6 and 12 months, in addition to stating that this modality of treatment was less painful, produced less resorption and had less relapse.2,3
A more recent variation was introduced by the Wilcko brothers et al. This includes an innovative strategy by combining selective alveolar corticotomy (SAC), bone graft and orthodontic forces, naming it: Accelerated Osteogenic OrthodonticsTM (AOOTM).4–6
Surgically facilitated orthodontics takes advantage of the phenomenon described in 1983 by Frost. He observed that a surgical wound of the bone leads to an increase in bone turnover and a decrease in bone density in the surgical area and defined it as regional acceleratory phenomenon (RAP). This phenomenon begins within a few days of the initial insult and may take from 6 to 24 months to resolve.7,8
SAC increases the rate of bone metabolism and produces a transient and reversible osteopenia that allows fast tooth movement. As long as dental movement continues, the RAP is prolonged; when it stops, the osteopenia disappears and when the orthodontic tooth movement is completed an environment that promotes alveolar remineralization has been created.7–11
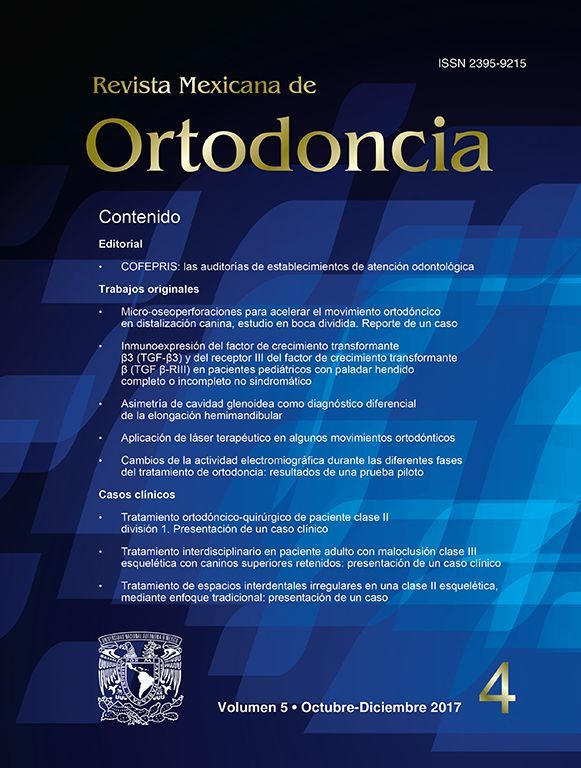
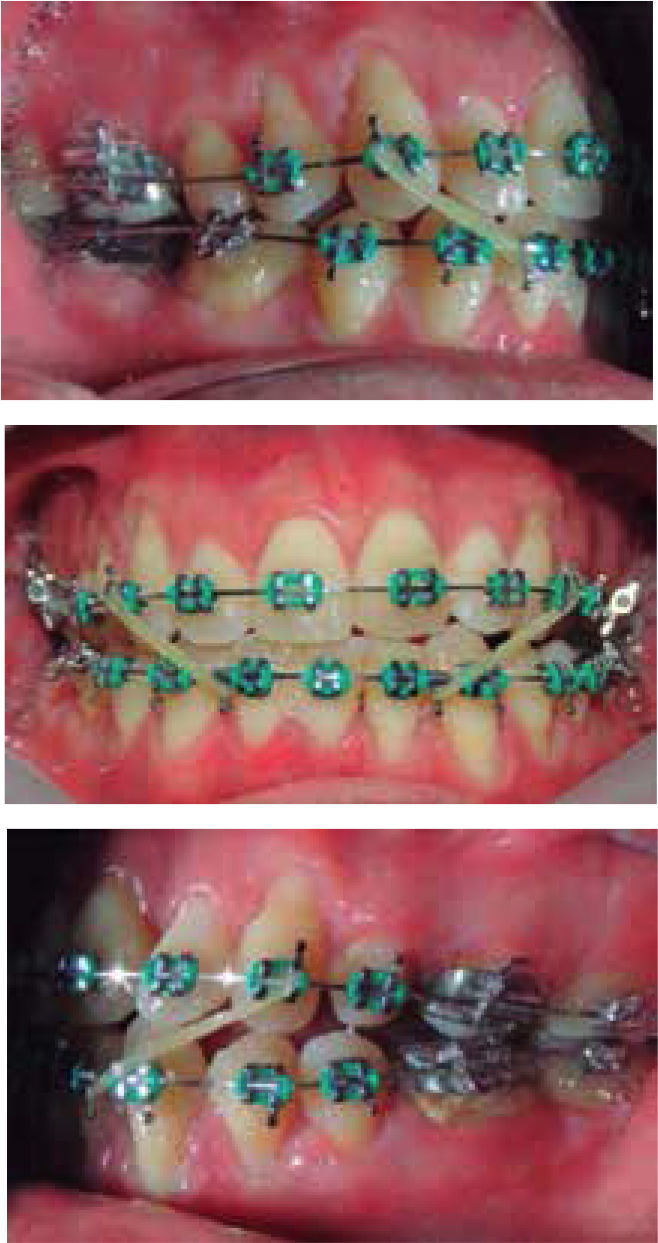
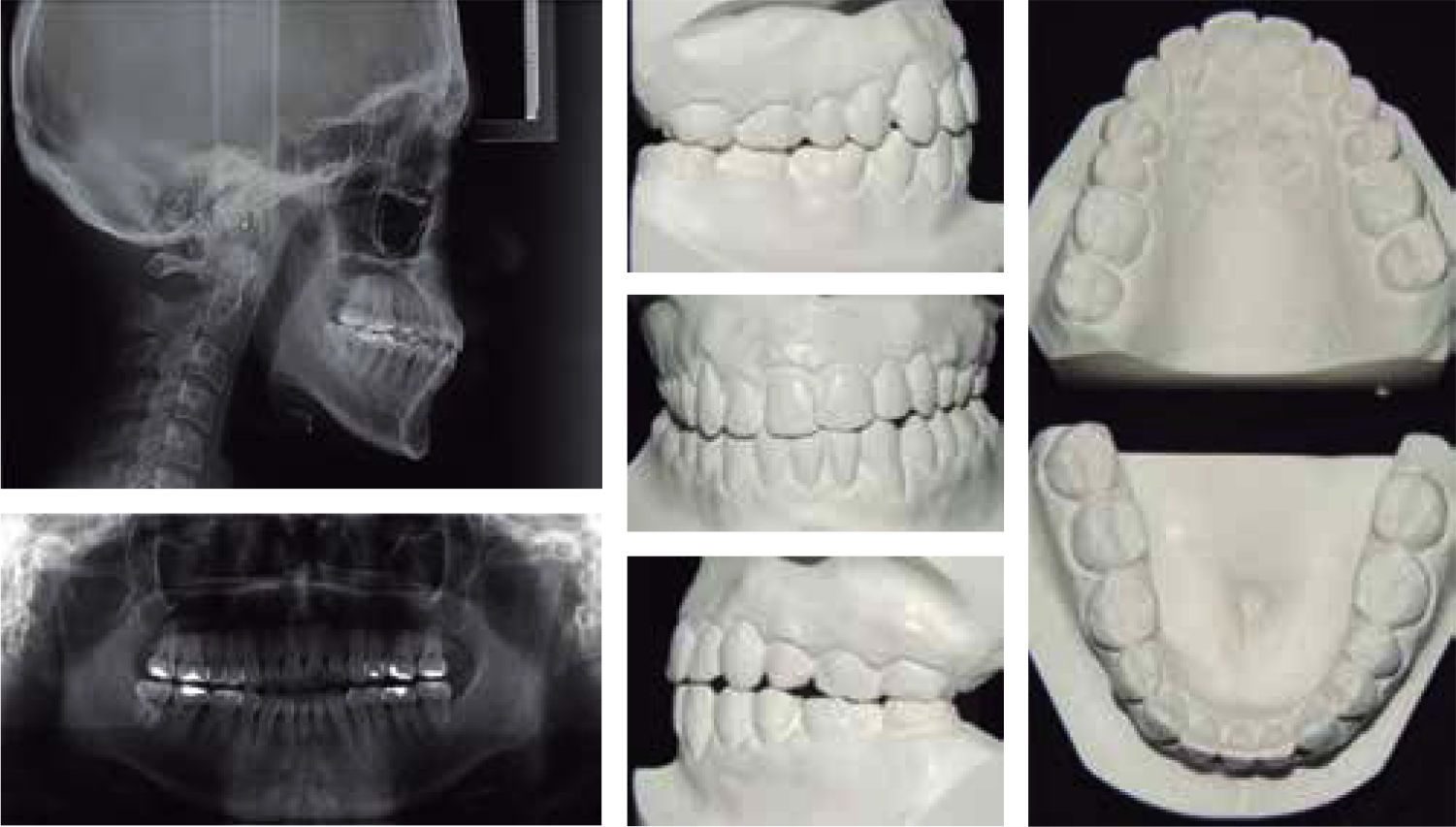
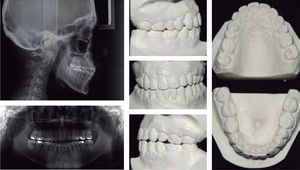
CASE REPORTMale patient 20 years of age with no relevant medical history attended the Orthodontics Clinic of the Faculty of Dentistry of UNAM with fixed appliances and a history of five years of previous orthodontic treatment with extractions. The usual records were prescribed for diagnosis in addition to a cone beam computed tomography (CBCT) (Figures 1 and 2).
DiagnosisSkeletal class I, dolichofacial, straight profile, upper incisor proclination bilateral molar class III (left cross bite), left canine class III, canine class I on the right side, teeth #22, 23 and 25 in cross bite, previously placed fixed appliances and absence of the teeth #18, 24, 28, 38, 32, 44 OD due to the prior orthodontic treatment; excessive interproximal recontouring in tooth #25; tooth 46 with severe mesial inclination; absence of overjet and overbite; gingival recession in teeth #14, 13, 23, 24, 33, 34 and 43; poorly adjusted restorations in teeth 16, 26, 36, 46; lack of root parallelism, root resorption of tooth #21, irregular alveolar ridge in the lower anterior region and fenestrations in the upper anterior segment.
Treatment goals- •
Decrease upper incisor proclination.
- •
Improve the molar and canine relationship.
- •
Improve the relationship of the upper and lower teeth (due to the absences by previous treatment).
- •
Correct crossbite in teeth #22, 23 and 25.
- •
Correct axial inclination of the tooth #46.
- •
Obtain a normal overjet and overbite.
- •
Maintain root length (mainly of tooth #21).
- •
Increase bone volume.
- •
AOOTM was suggested since this option offers a reduction in treatment time, as well as a reduction in the risk of causing root resorption of tooth #21.
- •
Level arches.
- •
Correct rotations.
- •
Class III mechanics.
- •
Coordinate arches.
- •
Root parallelism.
- •
Final detailing.
- •
Retention.
- •
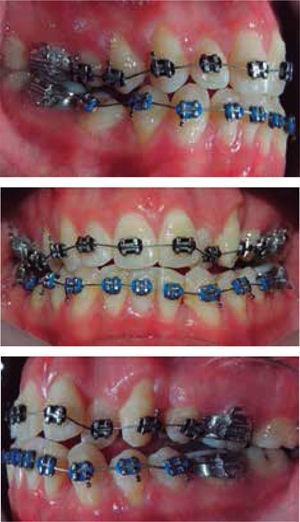
Subsequent to the placement of fixed 0.022” x 0.028” slot MBT appliances (3M Unitek Monrovia, California), upper and lower 0.014” NiTi archwires (Figure 3) were placed to schedule the AOOTM surgery in the following days, however, due to personal issues of the patient, he was operated six months after. During this period, alignment, leveling, and arch form was obtained using the following archwire sequence: 0.014”, 0.016”, 0.016” x 0.022”, and 0.017” x 0.025” NiTi.
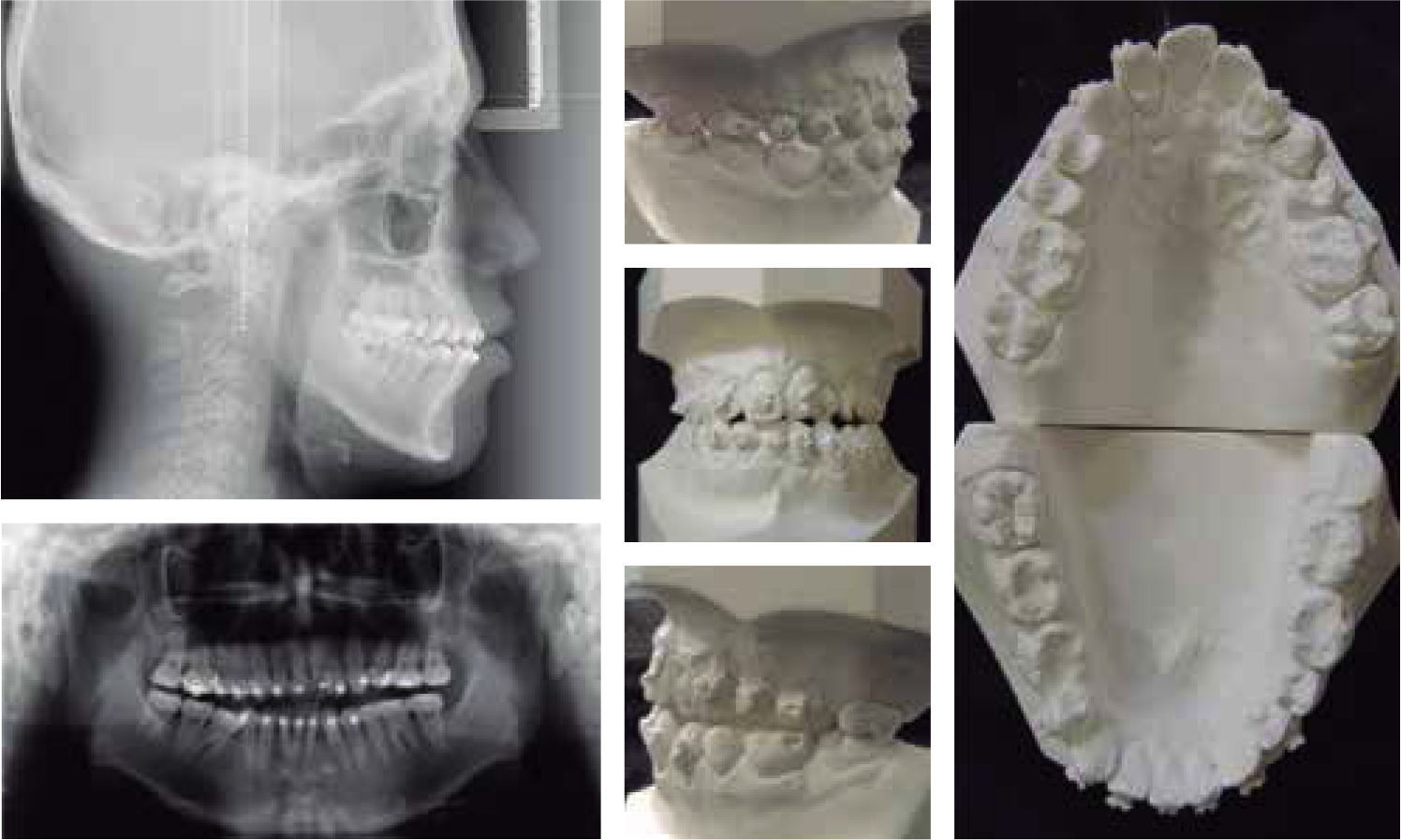
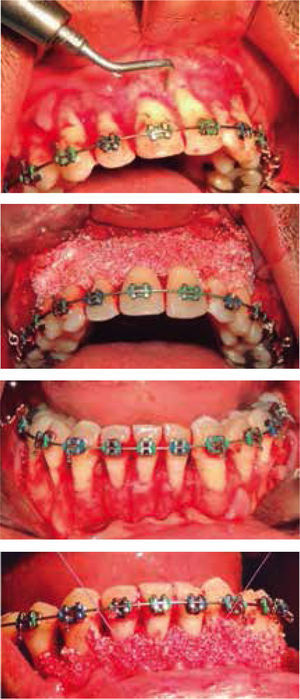
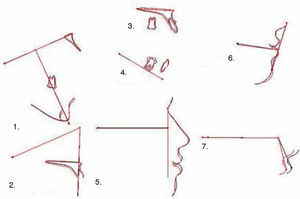
The surgery was scheduled and took place in conjunction with the Department of Implantology of the Faculty of Dentistry of the UNAM (Figure 4). A surgical map was given to the periodontist for the location and realization of the selective alveolar corticotomy (CAS).
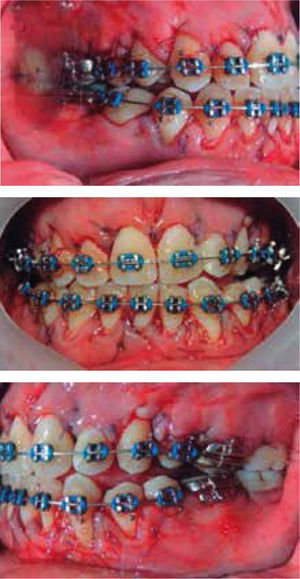
After anesthesia, full-thickness flaps were performed on the buccal area from tooth #16 to 26 bodies and from #36 to 46 (Figure 5). Afterwards, the cuts indicated by the map were done using the surgical piezotome with a BS1 Slim II tip (Acteon Satelec Piezotome®, Barcelona-Spain). Subsequently, the bone graft was placed, the flaps were repositioned and sutured and the first postsurgical activation with arches 0.017” x 0.025” NiTi was performed (Figure 6).
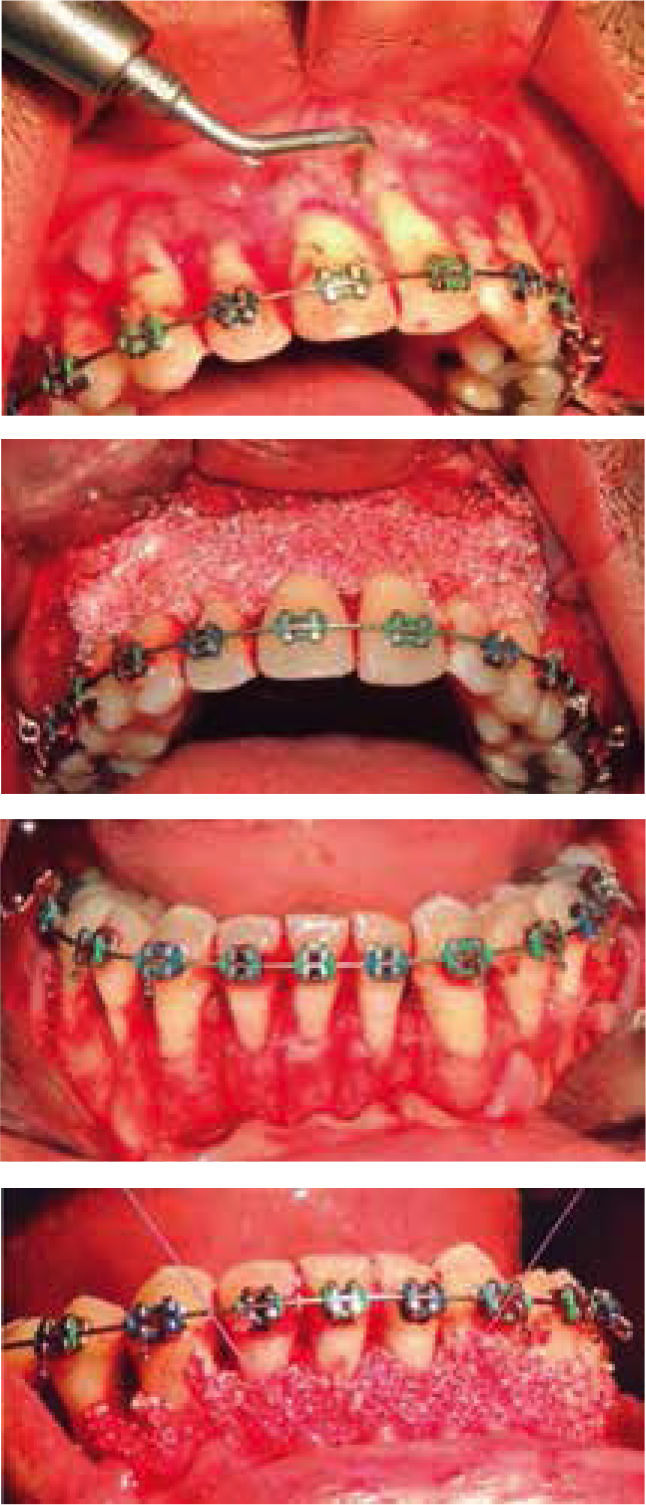
Treatment continued with arch coordination with 0.019” x 0.025” NiTi and 0.019” x 0.025” SS arch wires and the use of class III elastics for two months was prescribed (Figure 7).
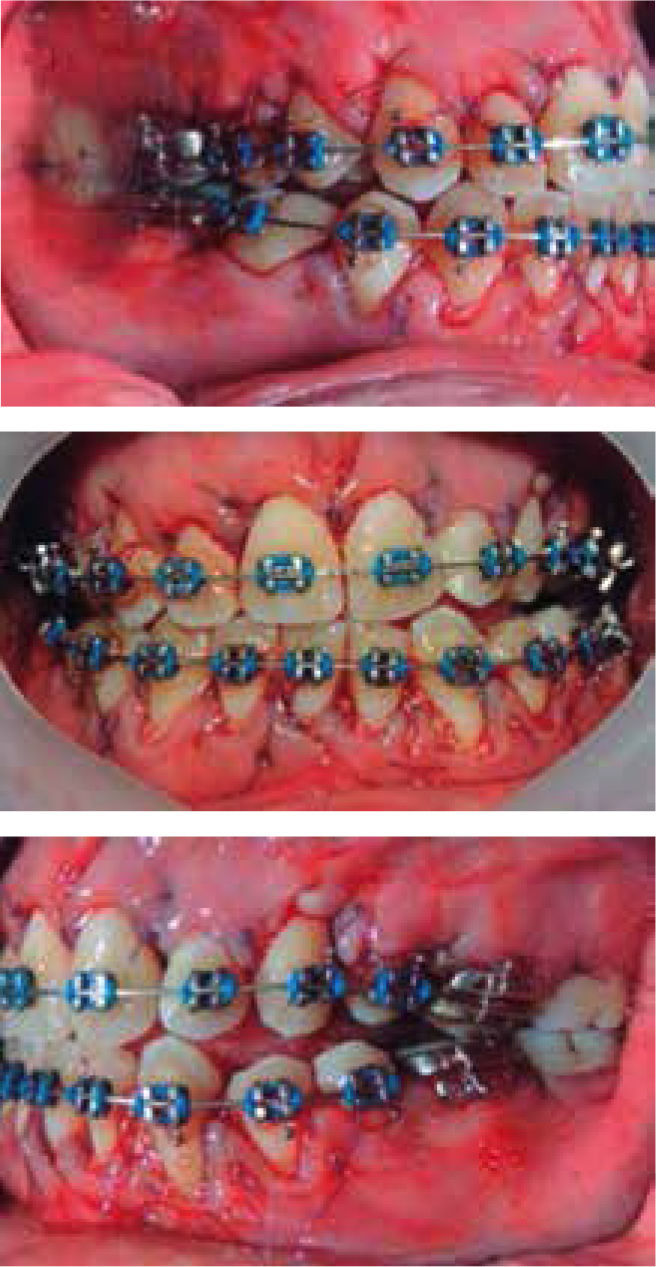
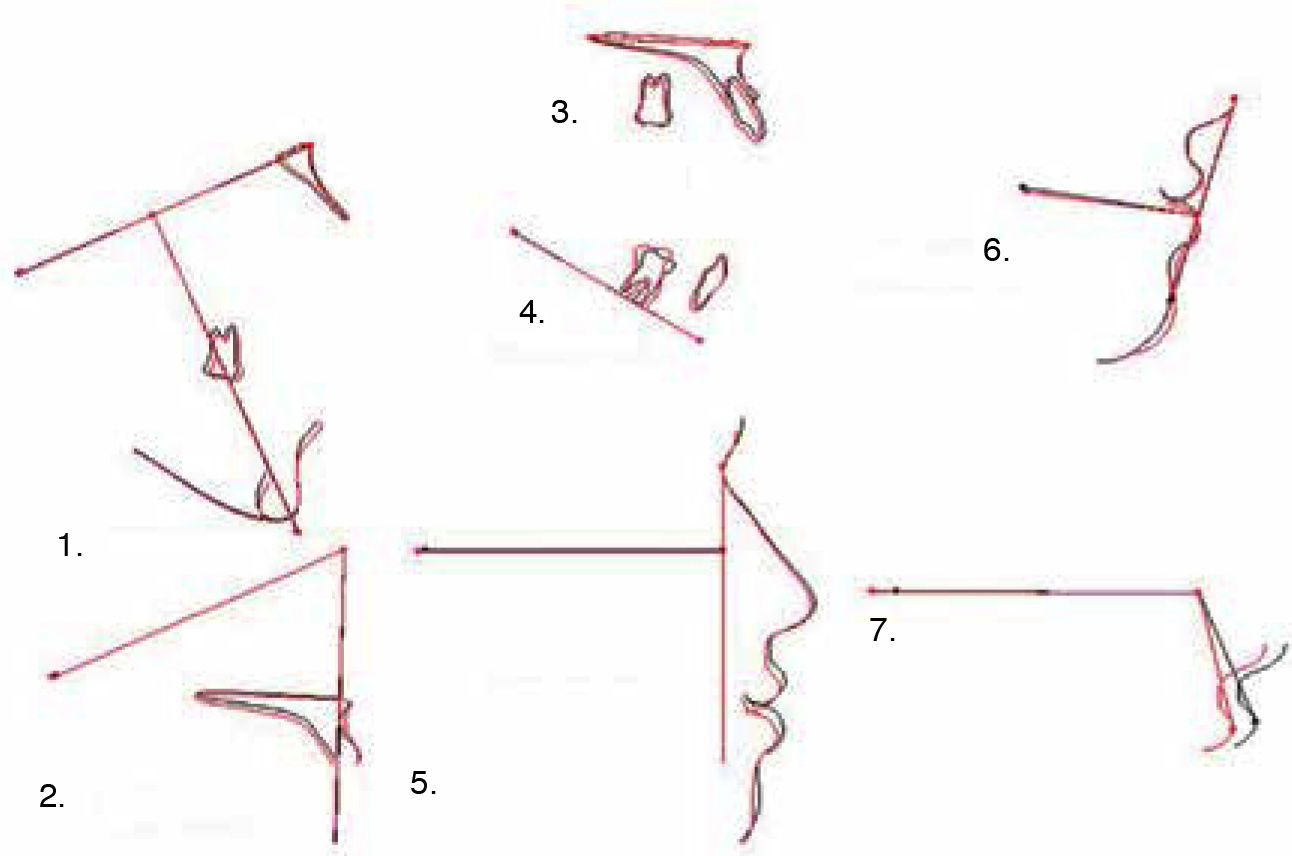
Brackets of teeth #14, 21, 34 and 45 were repositioned, re-leveling was performed using the following archwire sequence: 0.016” x 0.22” NiTi, 0.019” x 0.025” NiTi and 0.019” x 0.025” SS. Afterwards, the settlement phase and final detailing was conducted. Appliances were removed and a removable retention protocol was indicated for 24hours (Figures 8 and 9). Total treatment time was 16 months (six months of conventional orthodontics and AOOTM for 10 months).
Treatment resultsThrough orthodontic therapy the objectives were achieved for the most part, however, final occlusion was not ideal due to the limitations presented by the case initially, the absence of the teeth #24, 44 and 32, in addition to the excessive interproximal wear present on the tooth #25 and the undesirable movements of the previous orthodontic treatment; however the patient was very satisfied with the aesthetics and function.
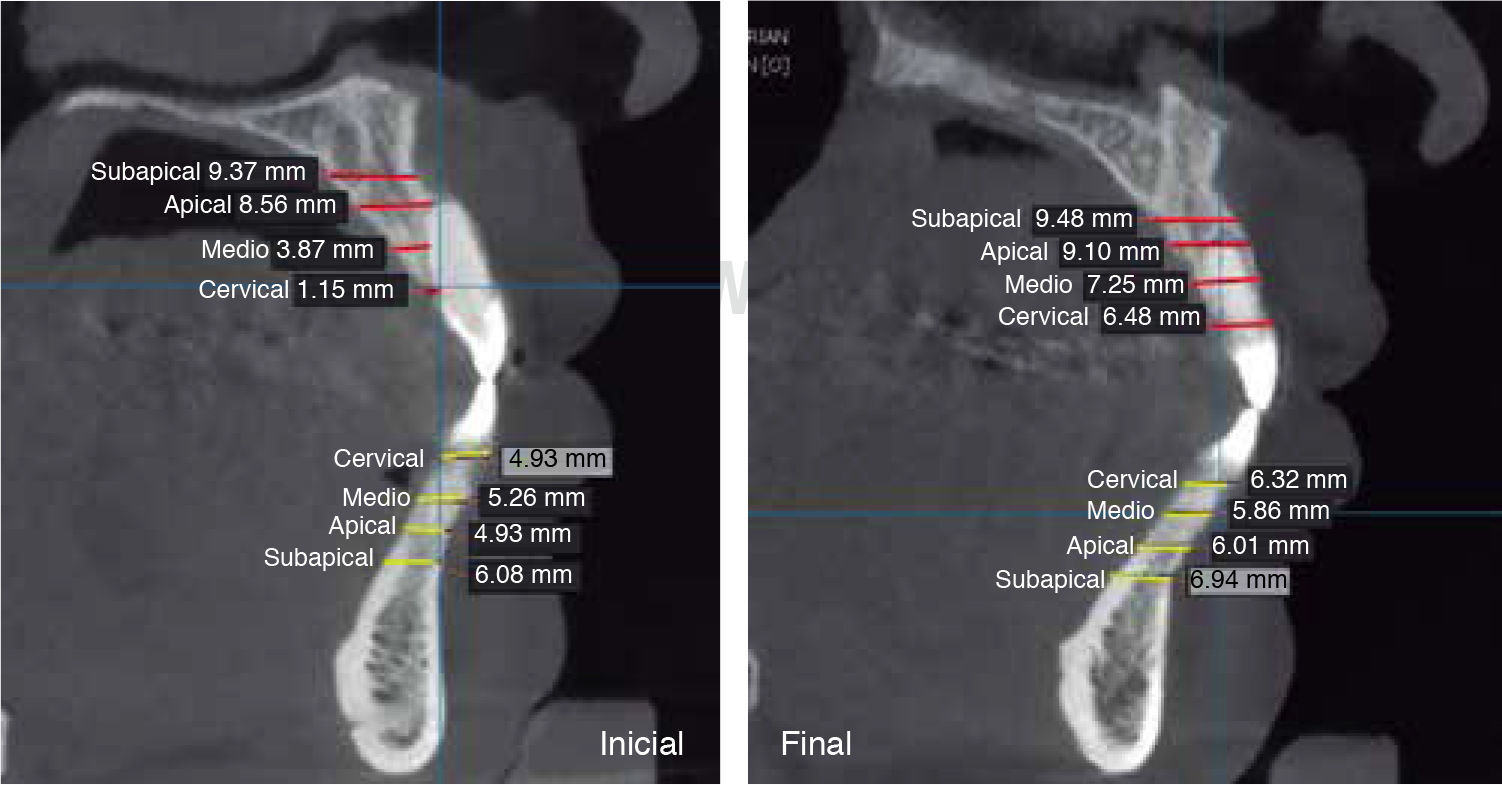
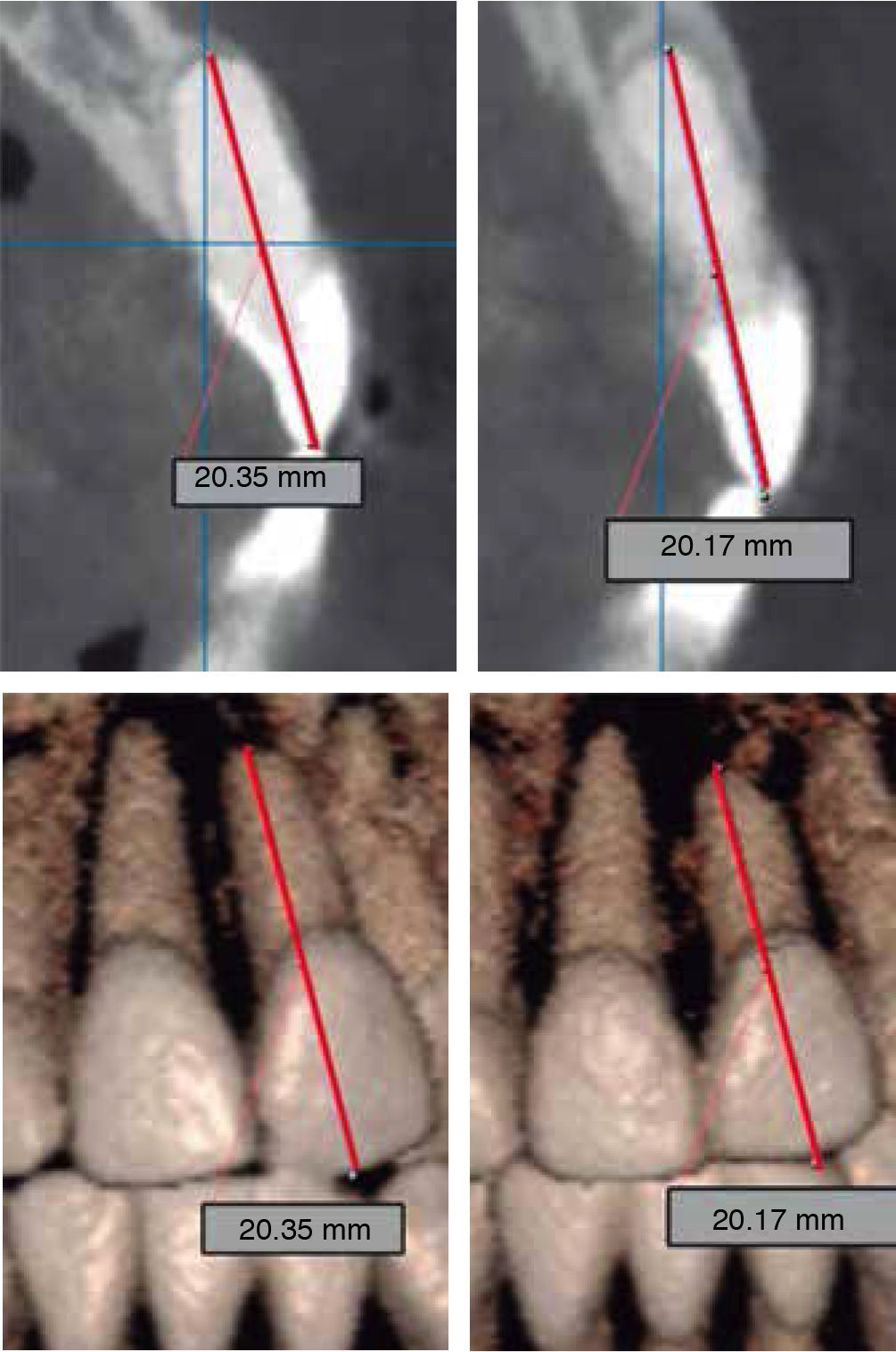
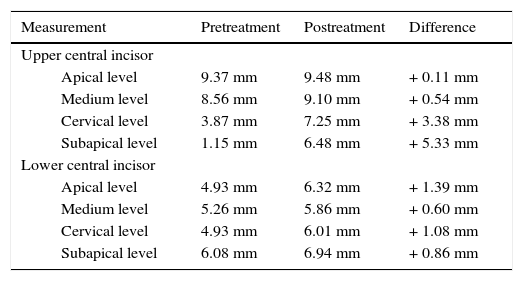
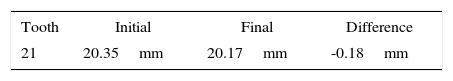
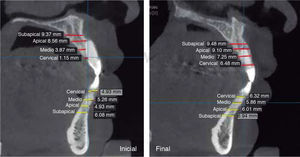
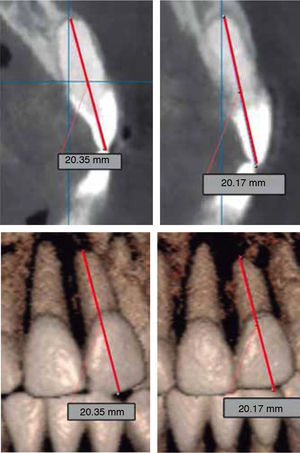
It is important to note the increase in bone volume that was obtained (Table I, Figures 10 and 11), as well as the fact that the root length of tooth #21 was not modified (Table IIandFigure 12).
Comparative measurements of bone volume increase.
| Measurement | Pretreatment | Postreatment | Difference |
|---|---|---|---|
| Upper central incisor | |||
| Apical level | 9.37 mm | 9.48 mm | + 0.11 mm |
| Medium level | 8.56 mm | 9.10 mm | + 0.54 mm |
| Cervical level | 3.87 mm | 7.25 mm | + 3.38 mm |
| Subapical level | 1.15 mm | 6.48 mm | + 5.33 mm |
| Lower central incisor | |||
| Apical level | 4.93 mm | 6.32 mm | + 1.39 mm |
| Medium level | 5.26 mm | 5.86 mm | + 0.60 mm |
| Cervical level | 4.93 mm | 6.01 mm | + 1.08 mm |
| Subapical level | 6.08 mm | 6.94 mm | + 0.86 mm |
Accelerated tooth movement is a theme in constant evolution. It is a therapeutic alternative that applied properly offers great advantages and excellent results.
Retreatment in orthodontics is a reason for consultation, patients may present with different conditions caused by the pretreatment such as: root resorption, dental extractions, interproximal wear, undesirable movements, etc. The patient hereby described presented dental root resorption. One of the advantages of AOOTM was of benefit to the patient since it decreases the risk that the resorption will continue. The reports of Wilcko et al., state that AOOTM causes osteopenia, which allows dental movements on a less dense bone surface, lowering the chance of root resorption (Table IIandFigure 12).5,6,12
The presence of fixed appliances for a long time and a poor dental plaque control causes a bigger chance of caries and periodontal problems. The advantage offered by surgically facilitated orthodontics is that it reduces treatment time and reduces the abovementioned risks. It also motivates the patient to restart an unfinished or poorly performed treatment, as was the case of the patient described in this case report.1–3,5,6,12–18
Figure 10 shows the presence of fenestrations in the upper anterior segment. The tissue's response to the AOOTM at the end of treatment was a large increase in bone volume. The increase in bone volume was real not by produced by a change of the root position or teeth inclination (Table I, Figures 10 and 11).5,6
AOOTM can be considered as very invasive due to the elevation of flaps of total thickness on the labial and lingual surfaces; however, this allows a better view of the surgical field, the direction of the roots and the area to fit the bone graft.5,6
There are a variety of techniques and modifications to perform the surgical procedure in surgically facilitated orthodontics. One of them is the one the proposed by Serge Dibart en where corticotomies are performed in a direct way through the periodontium, making this the least invasive procedure, however, it may be unsafe in some cases.16–18
Every surgically facilitated orthodontic treatment protocol has as a disadvantage the risks and limitations that all types of surgery offer (infection, inflammation, bleeding, postoperative discomfort, etc.), as well as an increase in the cost of treatment specially if a bone graft is placed.5,6,12–18 However, the advantages and benefits of this treatment modality justify its application provided that the patient is given all the relevant information in detail.
CONCLUSIONSAccelerated Osteogenic OrthodonticsTM, is a great therapeutic tool for the treatment of conventional, as well as complex cases, as was the case of a poorly performed previous orthodontic treatment. There is a need for further scientific evidence to affirm many concepts of this modality of treatment.
Student of the Orthodontics Specialty.
This article can be read in its full version in the following page: http://www.medigraphic.com/ortodoncia