To compare the sexual functions in women with labia minora hypertrophy and age-matched healthy controls.
Material and method43 patients with labia minora hypertrophy and 30 age-matched healthy controls were enrolled in the present study. The sexual functions of the women were evaluated by using the index of female sexual function (IFSF).
ResultsMean ages of the patients and controls were 30.06±7.11 and 31.34±4.12 (p=0.41), respectively. Mean total IFSF scores of the patients and controls were 24.18±3.24 and 27.53±4.43 (p<0.05), respectively. The subscale scores of IFSF-lubrication, orgasm, satisfaction and pain in the patient group were significantly lower than in the control group (respectively, p<0.001, p<0.05, p<0.001 and p<0.05). There was no statistically significant difference between IFSF-arousal scores of the patient and control groups (p=0.30). The mean IFSF-desire scores of the patient group was higher than the controls (p<0.001). Labia minora hypertrophy was significantly associated with female sexual dysfunction (odds ratio [OR]=14.97, 95% confidence interval [Cl]=[3.66–61.21], p<0.001).
ConclusionThis study suggests that patients with labia minora hypertrophy have poorer lubrication, satisfaction, pain, and orgasm scores on the IFSF scale compared to age-matched healthy controls.
Comparar las funciones sexuales en mujeres con hipertrofia de labios menores y un grupo control.
Material y métodoEn el presente estudio se incluyeron 43 pacientes con hipertrofia de labios menores y 30 controles sanos de la misma edad. Las funciones sexuales de las mujeres fueron evaluadas utilizando el Índice de Función Sexual Femenina (IFSF).
ResultadosLa edad promedio de las pacientes y controles fueron 30,06±7,11 y 31,34±4,12 (p=0,41), respectivamente. La puntuación total media del IFSF de las pacientes y controles fueron 24,18±3,24 y 27,53±4,43 (p<0,05), respectivamente. Las puntuaciones de la subescala de lentificación, orgasmo, satisfacción y dolor en el grupo estudio fueron significativamente menores que en el grupo control (p<0,001, p<0,05, p<0,001 y p<0,05). No hubo diferencias estadísticamente significativas entre las puntuaciones de excitación del IFSF de las pacientes y los grupos control (p=0,30). El promedio de las puntuaciones del deseo del IFSF del grupo de pacientes fue mayor que en el grupo control (p<0,001). La hipertrofia de labios menores se asoció significativamente con disfunción sexual femenina (odds ratio [OR]=14,97; intervalo de confianza [lC] del 95%=[3,66-61,21]; p<0,001).
ConclusiónEste estudio sugiere que las pacientes con hipertrofia de labios menores tienen peor puntuación en cuanto a lubricación, satisfacción, dolor y orgasmo en la escala del IFSF en comparación con el grupo control.
For some adult women, labia minora hypertrophy (LMH) and/or asymmetry can create psychosocial, esthetic, and/or functional concerns.1 LMH is defined as when the labia minora protrude through the labia majora. In addition to being esthetically unpleasant, LMH can interfere with hygiene and be uncomfortable and painful during exercise, sexual intercourse, or when wearing tight clothes.2 Many of the affected women feel embarrassed and thus avoid being seen naked, even by their partner.3 However, there are some women with hypertrophic labia minora who do not seek correction, because they see their morphology as a variation of “normal”. The others seek for intervention because of these esthetic and/or functional problems.4
Female sexual dysfunction (FSD) is defined as any disorder in the process of sexual contact, including six domains of desire, lubrication, arousal, satisfaction, pain, and orgasm. FSD causes distress in women and affects their relationships with partners and their quality of life.5 FSD affects approximately 43% of women.6 Of these women, difficulty with desire is the most common problem, followed by difficulty with arousal, orgasms, and pain.7
This study evaluated sexual function of women with LMH by using the Turkish version of the index of female sexual function (IFSF)8 and compared them with age-matched healthy controls. We hypothesized that LMH is associated with FSD in affected women.
Materials and methodsSubjects and study designA total of 43 women who were diagnosed with LMH who had attended the plastic and reconstructive surgery clinic as outpatients and 30 age-matched healthy women were enrolled in this study. The patients had a genital physical examination performed and were diagnosed with LMH by plastic and reconstructive surgeons. Only patients with grade 3 or 4 LMH were included the study. Labia minora hypertrophy was classified according to Franco9 into grades 1–4 depending on the protrusion of the labia minora through the labia majora as follows: grade 1, <2cm; grade 2, 2–4cm; grade 3, 4–6cm; and grade 4, >6cm. The exclusion criteria for the present study were patients who suffered from one of the following disorders: genitourinary, gynecologic or psychiatric disorders, malignancy, and/or patients with menopause. Controls were chosen among healthy pre-menopausal female staff in our hospital who did not have any major illness, psychiatric, gynecologic or endocrinologic disorder. We did not perform a genital examination in the control group which would potentially discourage their participation in the study. Instead, those enrolled in the control group were asked to disclose any complaints or abnormalities regarding their genital organs. We included only healthy volunteers in the control group.
All of the participants were married and signed study-specific informed consent forms. The study protocol was approved by the ethics committee of our institution.
InstrumentsThe Turkish version of the index of female sexual function (IFSF) was used to evaluate sexual function in all of the women in the present study. This index has 19 items, and is a self-reported measure of sexual function that was improved for use in epidemiological and clinical studies of female sexual dysfunction. The IFSF is easy to administer and has demonstrated ability to discriminate between normal and diseased populations. This test is reproduced from the version of the International Index of Erectile Function and was developed by Rosen.8 The IFSF was improved for the specific purpose of evaluating six domains of sexual function, including desire, lubrication, arousal, satisfaction, orgasm, and pain over the past month. The measure allows the calculation of specific indices for each dimension, as well as sexual function index, with higher scores showing greater levels of sexual functioning. Also, there is an inverse relationship between the pain score in IFSF and pain severity. The higher pain scores indicate less pain experienced. The Turkish version of the IFSF was developed by Aygin and Aslan.10
Statistical methodsThe data of patients and controls were compared by using the Student's t test. Women with a total IFSF score <26.55 were defined as having FSD10 and odds ratio test was performed according to this cut-off value. SPSS 13.0 (SPSS Inc.) was used for statistical analyses. A p value less than 0.05 was considered significant.
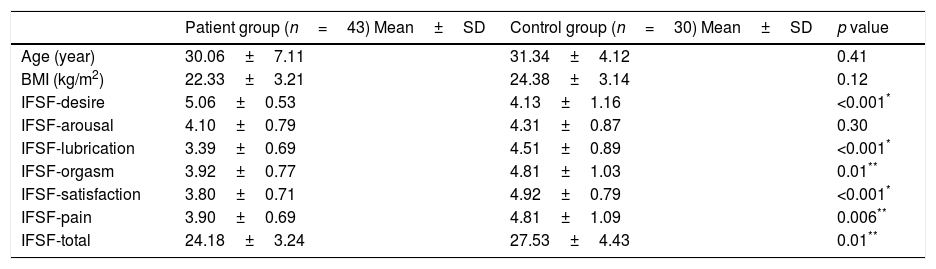
ResultsThe mean ages of the patient and control groups were 30.06±7.11 years and 31.34±4.12 years, respectively, with no difference between the groups (p=0.41). Table 1 shows the mean age, body mass index, and IFSF scores of women in the patient and control groups. In the control group, 4 women were nulliparous (13.33%), and 26 women were primiparous or multiparous (86.66%). In the patient group, 7 women were nulliparous (16.27%), and 36 women were primiparous or multiparous (83.72%). There was no significant difference in parity between the groups (p=0.39).
The mean of the IFSF scores of the women in the study.
| Patient group (n=43) Mean±SD | Control group (n=30) Mean±SD | p value | |
|---|---|---|---|
| Age (year) | 30.06±7.11 | 31.34±4.12 | 0.41 |
| BMI (kg/m2) | 22.33±3.21 | 24.38±3.14 | 0.12 |
| IFSF-desire | 5.06±0.53 | 4.13±1.16 | <0.001* |
| IFSF-arousal | 4.10±0.79 | 4.31±0.87 | 0.30 |
| IFSF-lubrication | 3.39±0.69 | 4.51±0.89 | <0.001* |
| IFSF-orgasm | 3.92±0.77 | 4.81±1.03 | 0.01** |
| IFSF-satisfaction | 3.80±0.71 | 4.92±0.79 | <0.001* |
| IFSF-pain | 3.90±0.69 | 4.81±1.09 | 0.006** |
| IFSF-total | 24.18±3.24 | 27.53±4.43 | 0.01** |
IFSF: index of female sexual function. BMI: BODY mass index.
The mean total IFSF score in the patient group was significantly lower (24.18±3.24) than that in the control group (27.53±4.43, p<0.05). The subscale scores of IFSF lubrication, orgasm, satisfaction, and pain in the patient group were significantly lower (for pain this indicates higher pain scores) than those in the control group (p<0.001, p<0.05, p<0.001 and p<0.05, respectively). There was no significant difference in IFSF arousal scores between the patient and control groups (p=0.30). The mean IFSF desire score in the patient group was significantly higher than that in the control group (p<0.001). Also LMH was significantly associated with FSD (odds ratio [OR]=14.97, 95% confidence interval [Cl]=[3.66–61.21], p<0.001).
DiscussionFemale sexual dysfunction is an important issue for many women because it disturbs their emotional relationship with their partner and also impairs their quality of life.5 The IFSF has been translated into numerous languages and has been widely used to evaluate female sexual function in a variety of nonclinical and clinical settings.11 This study aimed to evaluate the sexual function of women with LMH by using the IFSF. Overall, sexual function values of women in the patient group were significantly lower than those of the control group. This finding may be attributable to their genital pathology (LMH). Based on previous validation studies, a cut-off point for the total IFSF scale score (26.55) was proposed, with lower values indicating FSD.12 In the present study, when we assessed the total IFSF scores of patients with LMH according to this cut-off score, we found that 86% of the patients had sexual dysfunction.
A previous study investigated psychosexual function of patients who had a previous operation for LMH.13 In this study, the authors used the Pelvic Organ Prolapse Urinary Incontinence Sexual Function Questionnaire (PISQ) to evaluate sexual function of the patients. They did not find any difference in sexual function of patients who had a labioplasty performed and those who did not. However, this previous study had two major limitations. The first limitation is that there was no control group including age-matched healthy women. The other limitation is that the study did not assess details of the phases of sexual function. The PISQ is a status-specific sexual function questionnaire for evaluating female urinary incontinence and/or pelvic organ prolapse.14 The IFSF has been used more often than the PISQ to assess sexual function of women in clinical studies and epidemiological trails.
To the best of our knowledge, our study is the first to evaluate sexual function of women with LMH who did not undergo labiaplasty. In our study, sexual function of patients with LMH were compared with those of age-matched healthy women. The six phases of sexual function were investigated separately by using the IFSF. We found that the mean IFSF lubrication, orgasm, satisfaction, and pain scores in patients were lower than those in controls. However, the mean score of IFSF desire in patients was higher than that in controls. There was no significant difference in the IFSF arousal score between patients and controls (Table 1). Sexual function in women begins with desire, continues with arousal and lubrication, and finishes with an orgasm. Our findings indicated that sexual desire of patients with LMH was higher than that of controls. The arousal phases of patients with LMH and controls were similar. Therefore we believe that there are no problems at the beginning of sexual activity in women with LMH. However, the next phases, including lubrication and orgasm of patients, were significantly worse than those in controls. Although patients with LMH may suffer from excessive mucus production in daily life, in our study lower scores were declared about lubrication. This may be related about after taking off clothes, they faced with their genital pathology, and this psychological effect disturbed lubrication. Furthermore, obstruction of the entry of the vagina, might have diminished the lubrication.
Additionally, the IFSF satisfaction and pain scores in patients were lower than those in controls (for pain this indicates higher pain values).
Overall, our findings suggest that patients with LMH have worse sexual function compared to a control group. A total of 37 of 43 patients with LMH in the present study had FSD by using the IFSF. Although these patients had increased sexual desire, the total sexual function was worse than healthy controls. We speculate that patients with LMH have normal sexual desire and arousal initially, but this does not translate to adequate sexual satisfaction and orgasm during intercourse. The resultant unfulfilled sensuality would lead to build up of sexual desire over time.
There are some limitations to the present study. First, we did not have sex hormone profiles of the participants. Sex hormone values may affect female sexual function. The other limitation is the absence of IFSF data after surgical correction of LMH. Improvement of scores after treatment would definitely provide stronger evidence to prove the negative impact of this genital pathology on female sexual function. Future studies that include a longitudinal assessment of IFSF scores pre- and post-treatment in a larger group of patients over a longer period of time would more accurately clarify the relationship between LMH and FSD. Furthermore, the design of the control group in this study was subject to significant limitations. The selection of its members from female co-workers at our hospital runs the risk of incomplete or inaccurate disclosure of sexual function given the sensitivity of the topic. To mitigate this risk we ensured the anonymity of responses. Nevertheless, we cannot entirely exclude the effect of this limitation on our results. The fact that 86% of our patients reported sexual dysfunction however still lends strength to our conclusions.
Ideally, members of the control group should have been subjected to a comparable genital assessment to rule out LMH and measure its degree if present. This would have provided greater confidence in the study findings. Instead we queried those enrolled for any genital abnormalities. They were informed about LMH and its grades. As the control group was chosen from medical staff, they could easily understand LMH, and examined themselves to exclude any genital anomalies in the control group. Although we admit that this is a sub-optimal solution to exclude LMH, a genital examination would have deterred many from volunteering to this study and was therefore impractical given the intimacy of the organs involved. Thus, despite the difficulties imposed by the sensitivity of genital and sexual disclosure in a conservative society, we recruited the most practically feasible control group to compare sexual function with those who present with LMH.
Finally, human sexuality is a complex topic that is governed by a myriad of variables. The presence and nature of the partner, social and cultural values, religious beliefs, economic, familial, and genetic factors, in addition to education are all influential. Although, the ideal study would account for all these different elements, this is not always feasible nor practical. The findings of this study therefore should be interpreted in the context of the above disclosed limitations.
ConclusionOur study indicates that most women with LMH have sexual dysfunction. We speculate this to be attributable to their genital pathology (LMH), but further studies showing improvement in IFSF scores after surgical correction may furnish stronger evidence to confirm this relationship.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestThe authors declare that they have no conflicts of interest to disclose.