Comparison of early period sexual function parameters in patients who had surgical repair and conservative follow-up after penile fracture and the evaluation of surgical intervention time on these parameters were planned in this study.
Materials and methodsTotal of 26 patients who were treated for penile fracture were evaluated. 19 patients had surgical repair and 7 patients had conservative treatment.
Sexual function and erectile dysfunction (ED) degree of the patients before penile fracture and in the 12th week after fracture were evaluated with 5-question International Index of Erectile Function (IIEF-5) questionnaire, Erection Hardness Score (EHS), Sexual Encounter Profile(SEP) 2 and SEP 3. Parameters showing sexual function before and after the fracture were compared.
ResultsIn both groups, a significant change was detected in IIEF-5 score, EHS, SEP-2 and SEP-3 parameters of the patients measured after penile fracture compared to the values before the fracture (all parameters, p<0.05). No difference was detected in the parameters measured before and after the fracture among surgical repair and conservative treatment groups (all parameters p>0.05). Mean time passing until the surgery after fracture was measured as 9.6±6.85h in 19 patients who had surgery.
ConclusionA difference wasn’t detected in sexual parameters in conservative treatment and surgical repair groups in this study. As a significant decrease was observed in sexual function parameters even in conservative treatment cases without sudden detumescence and tunica albuginea rupturing, we think that quick surgical exploration would be useful in cases considered to have penile fracture.
En este estudio se planificó la comparación de los parámetros de función sexual en el período temprano en pacientes sometidos a reparación quirúrgica y seguimiento conservador después de una fractura de pene y la evaluación del tiempo de intervención quirúrgica sobre estos parámetros.
Materiales y métodosSe evaluaron un total de 26 pacientes que fueron tratados por fractura de pene: 19 fueron sometidos a reparación quirúrgica y 7 tuvieron un seguimiento conservador. La función sexual y el grado de disfunción eréctil de los pacientes antes de la fractura de pene y en la semana 12 después de la fractura se evaluaron con el cuestionario International Index of Erectile Function de 5 preguntas (IIEF-5), el Erection Hardness Score (EHS), y el Sexual Encounter Profile (SEP) 2 y SEP 3. Se compararon los parámetros que muestran la función sexual antes y después de la fractura.
ResultadosEn ambos grupos se detectó un cambio significativo en la puntuación IIEF-5 y los parámetros EHS, SEP 2 y SEP 3 de los pacientes medidos después de la fractura de pene en comparación con los valores antes de la fractura (todos los parámetros, p<0,05). No se detectaron diferencias en los parámetros medidos antes y después de la fractura entre los grupos de reparación quirúrgica y tratamiento conservador (todos los parámetros p>0,05). El tiempo medio transcurrido hasta la cirugía después de la fractura se midió como 9,6±6,85h en los 19 pacientes intervenidos.
ConclusiónNo se detectaron diferencias en los parámetros sexuales entre los grupos de observancia conservadora y reparación quirúrgica en este estudio. Como se observó una disminución significativa de los parámetros de función sexual incluso en casos de seguimiento conservador sin detumescencia súbita y desgarro de la túnica albugínea, pensamos que la exploración quirúrgica rápida sería útil en los casos en los que se considere que tienen fractura de pene.
Penile fracture is the rupturing of Buck fascia over corpus cavernosum generally due to a blunt trauma when the penis is erected. The diagnosis is generally clinical. On the other hand, extra examinations such as ultrasonography and magnetic resonance imaging (MRI) can be used for diagnostic validation in suspected cases. Thus a good anamnesis and physical examination in penile fracture patients has the key role in the correct diagnosis and the quick applicability of the treatment.1–3
While conservative treatment was applied in penile fracture treatment before, early surgical treatment is the recommended treatment today as early surgical intervention has lower complication rates. Although different surgical techniques are available, deglovation of penis skin through subcoronal incision and repairment of the torn fascia with absorbable sutures constitute the basis of the surgical treatment.3–5
In previous studies, it was reported that erectile dysfunction (ED) reaching 80% can be seen in patients following conservative treatment. But degradation in sexual functions and ED can be seen in patients despite the surgical repair following penile fracture.5,6
Comparison of early period sexual function parameters in patients who had surgical repair and conservative treatment after penile fracture and the evaluation of surgical intervention time on these parameters were planned in this study.
Material and methodsThe present study protocol was reviewed and approved by the Institutional Review Board of Necmettin Erbakan University Meram Faculty of Medicine (approval No. 20202519). Informed consent was obtained by all subjects when they were enrolled.
A total of 26 patients diagnosed with penile fracture and treated in a university hospital between 2015 and 2020 were evaluated.
Diagnosis was made through anamnesis, physical examination and penile ultrasonography (USG). Penile magnetic resonance imaging (MRI) was performed to confirm diagnosis in patients with high hematoma and thus cannot be completely diagnosed through penile USG and retrograde urethrography was performed to evaluate urethral injury in patients with urethrorrhagia and hematuria.
Age, fracture formation, medical or surgical method applied after fracture and time passing between diagnosis and surgery were recorded for the patients. Sexual function and erectile dysfunction (ED) degree of the patients before penile fracture and in the 12th week after fracture were evaluated by measuring 5-question International Index of Erectile Function (IIEF-5) questionnaire, Erection Hardness Score (EHS), Sexual Encounter Profile (SEP) 2 (Were you able to insert your penis into your partner's vagina?) and SEP 3 (Did your erection last long enough for you to have successful intercourse?) In patients who also have urethral injury, urination condition was evaluated through uroflowmetry and postop International Prostate Symptom Score (IPSS).
Conservative treatment groupIn patients who didn’t have severe pain, extensive hematoma, early detumescence and/or the presence of suspicious linear rupture of the tunica albuginea detected radiologically, conservative treatment was applied through cold application, non-steroid anti-inflammatory drug application and compression with coban bandage.
Surgical repair groupIn patients with early detumescence, extensive hematoma, radiologically detected to have significant rupturing in tunica albuginea, surgical repair was performed. In these patients, urethral catheterization was applied with 16 f foley before the surgery. Penis skin was degloved through subcoronal incision in all patients who were applied surgery. Defect zone was repaired with absorbable 4/0 vicryl sutures to form two layers. Medical dressing was performed by compressing coban bondage after repair. Penis was elevated and fixated so that postop edema would be low. Urethral catheter was removed on postop 1st day in patients without urethral injury and on postop. 10th day in patients with urethral injury.
19 out of 26 patients had surgical repair and 7 had conservative treatment. Patients were separated into two groups as surgical repair group and conservative treatment group. Parameters showing sexual function before and after fracture were compared in the general patient population and among the two groups.
Statistical analysisStatistical analysis was performed with SPSS, v.23.0 statistical software (SPSS, Inc., Chicago, IL, USA). The categorical variables were described as frequencies and percentages. Continuous variables were presented as mean and standard deviations.
The McNemar and Wilcoxon Signed Rank Tests were used to analyze the relationship between categorical and quantitative variables before and after treatment.
Independent T and Chi-Square (χ2) tests were used to compare the relationship between categorical and quantitative variables penile fracture subgroups. p value below 0.05 was considered statistically significant.
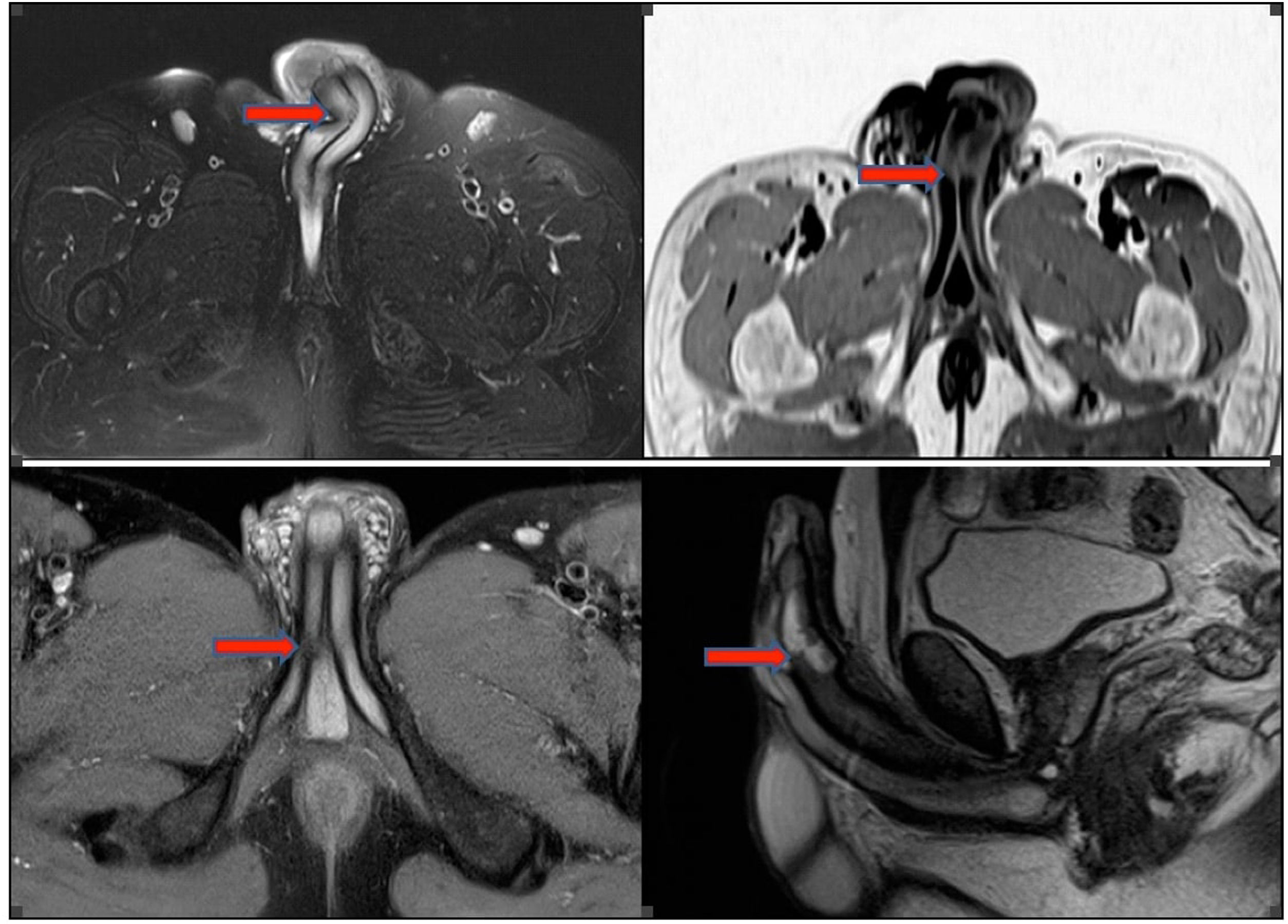
ResultsMean age of the patients was 46±13.2 years. While 17 patients (65.4%) had forced sexual intercourse in the etiology, Taghaandan maneuver (lateral forcing of erected penis by hand) performed to end erection was detected in 6 (23%) patients, rolling in bed was detected in 2 (7.7%) patients and forcing during masturbation was detected in 1 (3.9%) patient. Patients were admitted with ecchymosis, swelling, thudding noise, sudden detumescence and severe pain complaints. Penile MRI was performed in 4 patients (15.3%) in addition for diagnosis (Fig. 1).
Urethral injury was detected in retrograde urethrography performed in two patients due to hematuria and urethrorrhagia. Mean time passing until the surgery after fracture was measured as 9.6±6.85h in 19 patients who had surgery. Mean hospitalization duration of the patients was measured as 3.2±1.36 days (Table 1).
Details of penile fracture patients.
| Age (mean±SD) | 46±13.2 |
| Cause of penile fracture n (%) | |
| Forced sexual intercourse | 17 (65.4%) |
| Taghaandan maneuver | 6 (23%) |
| Rolling in bed | 2 (7.7%) |
| Forcing during masturbation | 1 (3.9%) |
| Clinical admittance way n (%) | |
| Penile ecchymosis | 24 (92.3%) |
| Penile swelling | 22 (84.6%) |
| Thudding noise | 20 (76.9%) |
| Sudden detumescence | 19 (73%) |
| Severe pain | 18 (69.2%) |
| Additional radiological imaging for diagnosis n (%) | |
| MRI | 4 (15.3%) |
| Urethrography | 2 (7.7%) |
| Treatment method n (%) | |
| Surgery | 19 (73%) |
| Conservative | 7 (27%) |
| Time from trauma to surgery (hours) (mean±SD) | 9.6±6.85 |
| Urethral injury n (%) | 2 (7.7%) |
| Mean hospitalization duration (days) (mean±SD) | 3.23±1.36 |
A significant change was detected in IIEF-5 score, EHS, SEP-2 and SEP-3 parameters of the patients measured after penile fracture compared to the values before the fracture (p<0.001, p=0.001, p=0.008, p<0.001, respectively). Change in sexual function parameters were measured as significant in terms of all parameters both in surgical repair group and conservative treatment group.
No difference was detected in IIEF-5 score, EHS, SEP-2 and SEP-3 parameters measured before and after the fracture among surgical repair and conservative treatment groups (all parameters p>0.05). Parameters showing erection functions before and after penile fracture are available in Table 2.
Parameters showing erection functions before and after penile fracture.
| Parameters | Total (n=26) | Surgical repair (n=19) | Conservative treatment (n=7) | P before vs after penile fracture | p surgical repair vs conservative treatment |
|---|---|---|---|---|---|
| IIEF-5 score before penile fracture | 22.69±1.56 | 22.78±1.27 | 22.42±2.2 | <0.001c | 0.61* |
| IIEF-5 score after penile fracture | 16.62±6.3 | 16.68±6.6 | 16.43±5.6 | 0.92* | |
| EHS before penile fracture | 3.88±0.32 | 3.95±0.22 | 3.71±0.48 | 0.001c | 0.10* |
| EHS after penile fracture | 2.81±1.09 | 2.84±1.16 | 2.71±0.95 | 0.78* | |
| SEP 2 before penile fracture n (%) | |||||
| Yes | 26 (100%) | 19 (100%) | 7 (100%) | 0.008b | N/A |
| No | 0 | 0 | 0 | ||
| SEP 2 after penile fracture n (%) | |||||
| Yes | 18 (69.2) | 13 (68.4) | 5 (71.4) | 0.88a | |
| No | 8 (30.8) | 6 (31.6) | 2 (28.6) | ||
| SEP-3 before penile fracture n (%) | |||||
| Yes | 24 (92.3) | 1 (5.3) | 1 (14.3) | <0.001b | 0.44a |
| No | 2 (7.7) | 18 (94.7) | 18 (85.7) | ||
| SEP-3 before penile fracture n (%) | |||||
| Yes | 12 (46.2) | 9 (47.4) | 3 (42.9) | 0.83a | |
| No | 14 (53.8) | 10 (52.6) | 4 (57.1) | ||
Abbreviations: IIEF-5: 5-question International Index of Erectile Function questionnaire, EHS: Erection Hardness Score, SEP: Sexual Encounter Profile, N/A: not applicable.
It was detected that 1h delay in surgery time caused a decrease of 0.48 points in IIEF-5 score after fracture and 0.51 points in EHS score after fracture based on the correlation analysis made on surgical repair group and this condition was detected to be statistically significant (p=0.036, p=0.024, respectively). In postop. 12th week controls of two patients who had urethral repair, mean Qmax values were measured as 22.1ml/s and IPSS score was measured as 8. A significant nodule and curvature weren’t detected in postoperative 12th week in the patients.
Finally, the severe ED rate (according to IIEF-5 score) was 31.6% (6/19) in the surgical treatment group and 28.6% (2/7) in the conservative treatment group at 12th week. This difference was not significant and was in line with the SEP-2 results (p=0.88).
DiscussionA typical thudding noise, severe pain and severe detumescence generally follow the trauma during penile fracture.7 Patients are clinically admitted with penile swelling, deformation and ecchymosis in the skin covering the penis. The diagnosis is generally clinical. But USG and MRI are auxiliary imaging techniques to confirm diagnosis. These radiological examinations are used to clarify the diagnosis and determine surgery selection.3,8 Although we based our diagnosis on anamnesis and physical examination findings in our patients, all patients had ultrasonography to detect any presence of tunica albuginea tearing and the defect area. MRI was used in 4 patients (15.3%) who were undiagnosable through USG due to hematoma.
Most common causes of penile fracture were stated as forced sexual intercourse, forced flexion with Taqaandan maneuver, masturbation and rolling in bed respectively. It was most commonly observed in woman on top and doggy style positions. The main factor here is the bending of erected penis during re-penetration after it exits the vagina.9,10 Forced sexual intercourse with 65.4%, forced flexion with 23%, forcing during masturbation in 3.9% and rolling in bed and falling on it in 7.7% were detected in the etiology of our patients and these findings were parallel to literature.
Penile fracture patients are clinically admitted with penile swelling, deformation and penile skin ecchymosis and eggplant deformity. Ecchymosis can reach inside scrotum and perineum and even suprapubic and inguinal areas when buck's fascia is disintegrated.11,12
A clinical condition which may imitate penile fracture is penile vascular bleeding. Superficial or deep dorsal penile vein or artery may be traumatized by a penile trauma and may cause bleeding imitating tunica rupture. In such condition, characteristic tearing sound of early detumescence, severe pain and tunica rupture may not be observed in the physical examination and ecchymosis amount is expected to be a little lower than that detected in a real tunica rupture. Kozacıoğlu et al. reported that 3% of the patients they operated due to penile fracture didn’t have tunica rupture and they only had penile vascular injury.13
The most common complaint was penile ecchymosis in the patients we included in the study (92%). Penile swallowing, thudding noise, early detumescence and severe pain were also observed with percentages of 76%, 73% and 69%. 7 patients (26.9%) didn’t have severe pain and early detumescence complaints in our patient group and suspicious linear tunica albuginea rupture was detected radiologically. Although penile vascular injury is primarily considered in these patients in diagnosis, it is not possible to determine the presence of penile fracture without surgical exploration. According to the EAU guideline, patients without significant ruptures in tunica albuginea can be followed up with conservative treatment.14 We applied conservative treatment without surgical treatment in these patients not detected to have significant and wide tunica albuginea rupture due to clinical and radiological findings.
Methods like cold application and NSAI drugs can be applied in conservative treatment.14 We applied conservative treatment through cold application, non-steroid anti-inflammatory drug application and compression with coban bandage in these seven patients.
While conservative treatment was common in penile fracture patients until the beginning of 1980, treatment through early surgical intervention is suggested today as early surgical intervention presented fast recovery, low morbidity, low complication rates and low penile curvature rates in late period.4,15 We tried to apply early surgical treatment in 19 patients in our study. The mean time passing between trauma formation and surgery was 9.6h in these patients. Based on patient anamnesis, this time was detected to be caused by the delays caused in coming to the hospital due to being ashamed and spontaneous recovery hope.
Urethral damage ratio is between 9 and 20% with penile fracture. Presence of tear and urethrorrhagia in bilateral corpus cavernosum is a warning sign for urethral injury. Retrograde urethrography or cystoscopy must be performed in urethral injury suspected conditions.16 Urethral injury was detected in the retrograde urethrography performed due to urethrorrhagia and hematuria in 2 out of 26 patients in our study (8.3%). Two staged repair with 4.0 absorbable suture was applied through the catheter in the surgery. Mean postoperative Qmax of the patients was detected as 22.1ml/s.
Plaque, nodule, curvature formation and erectile dysfunction complications may be observed after penile fracture surgery. Significant nodule or curvature wasn’t detected in our study since the patients were evaluated in postoperative early period (12th week).5,6,9
Erectile dysfunction formation after penile fracture is a quite disturbing complication for the patients. Although sexual functions are quite well after the trauma in isolated penile vascular injuries which may be confused with penile fracture, ED can be observed at high ratios in patients with tunica rupture and are not surgically treated.6 Kakoi et al.17 reported that IIEF-5 scores which were 21 and 17 before penile fracture in two patients over 50 years of age decreased to 8 in two months after the fracture in both patients. But in this series, a recovery was reported since IIEF-5 score was measured as 21 and 12 in the sixth month. In their penile fracture series of 300 patients, El Atat et al.5 reported that only 2 patients (0.6%) had erectile dysfunction.5 Amer et al.9 reported erectile dysfunction with a ratio of 1.9% after the surgery. Barros et al.2 reported ED with a ratio of 14.7% in patients they followed for six months after penile fracture and evaluated their sexual function with IIEF-5 but IIEF-5 values were not given in the study. Patil et al.12 reported ED with a ratio of 44.4% in their series of 18 patients. In the study by Zargoshi6 examining 362 penile fracture patients, it was reported that 10 patients were followed-up without being operated and 352 patients were operated. They stated that ED occurred in 80% (8/10) of non-operated patients. They reported that ED occurred in 8 of the operated patients (2.27%) and IIEF and EHS scores were good apart from these patients. In addition, they reported that10 patients didn’t have a significant rupturing in tunica albuginea during the surgery, but they only had penile venous injury and the erectile functions of these patients were totally normal after the surgery.
In our study, IIEF-5 score measured in the 12th week after penile fracture in the group which had surgery was detected to decrease nearly 6 points compared to the score before the fracture (22.78 vs 16.68). SEP 2: Were you able to insert your penis into your partner's vagina? While none of the patients responded as “No” before fracture in the surgery group, the ratio of patients responding as “No” was measured as 31.6% in the 12th week after fracture. This may be interpreted as the lack of being able to have sexual intercourse in the 12th week in 31.6% of the patients. Interestingly, a decrease was detected in IIEF-5 score, EHS, SEP-2 and SEP-3 parameters in the patients group followed-up with conservative treatments similar to surgical repair group. In addition, the severe ED rate (according to IIEF-5 score) was 31.6% (6/19) in the surgical treatment group and 28.6% (2/7) in the conservative treatment group at 12th week. This rate was similar (p=0.88).
As a result, no difference was detected in sexual function parameters among surgical repair group and conservative treatment groups. Although the patients in this group are mostly defined as penile vascular injury in literature, this decrease in sexual function scores makes us consider the suspicious tunica albuginea trauma on radiological imaging. Thus, we don’t recommend conservative treatment in patients considered to have penile fracture diagnosis clinically. We think that making a surgical exploration and repairing even a small tunica rupture would be advantageous in these patients. Since the sexual function parameters were checked in an early period like 12 weeks in our study, we hope that these scores with improve in both groups in line with literature in the long term.
Katı et al.15 reported that the IIEF-5 scores decreased to 20 from 22 in the sixth month in patients who were applied surgery in a mean duration of 250min (hospital arrival time: 132min, time passing until the intervention: 118min) after fracture formation. They reported that the good results were related to early surgical intervention. Kozacıoğlu et al.13 separated penile fracture patients into three groups based on intervention time as 0–6h, 6–12h and 12–24h. Mean intervention time of the patients was measured as 8.9h. In postoperative 1st year, no difference was detected in IIEF-15-ED scores among the groups. It was stated that erectile function score decreased to 26.5 from 26.9 in the general patient group. In addition, another study reported that surgical intervention delay longer than 24h increased erectile dysfunction and lengthened hospitalization duration. In line with literature, mean surgical intervention time after penile fracture was measured as 9.6h in our study. But based on the correlation analysis, a significant decrease was detected in IIEF-5 and EHS scores for every 1h delay in surgical intervention. Thus we think that early referral, quick diagnosis and urgent surgical intervention are quite important especially to protect erectile functions in penile fracture patients.
Since penile fracture is not a very common condition, there are limited patient series in the literature. Panella et al.18 performed surgical treatment to patients with high suspicion for penile fracture in their study including 20 patients, while conservative treatment was applied to patients with tunica albuginea rupture smaller than 5mm. Conservative patient selection is not clear according to the guidelines, as there are not enough studies on this subject. A fracture-like clinic can occur due to injury of penile vessels and/or tunical contusion and thinning, and thus clinical and radiological false positives can be seen in the diagnosis of penile fracture. Therefore, a conservative follow-up option can be considered in suspected fracture patients without severe pain, extensive hematoma, and early detumescence. In this study, conservative treatment was applied to patients with mild clinical situation, no early detumescence and no extensive hematoma.
This may be considered as an important limitation for the study, as patient selection is made according to subjective criteria. Despite this limitation, no significant difference was found between the post-treatment parameters and ED rates between the surgical repair group and conservative treatment groups. This indicates that although the clinical picture of the patient is mild, the post-traumatic erectile function can be significantly affected. Therefore, we think that surgical exploration may be a more appropriate option in patients with a diagnosis of penile fracture. Low number of patients, lack of late-term sexual function parameters, questioning pre-fracture sexual parameters after the fracture were the other limitations of this study.
In conclusion, although it is a rare urological emergency, penile fracture has an important effect on general health and sexual functions. Thus early referral, quick diagnosis and urgent surgical intervention may contribute the penile fracture patients to lead a normal life.
A difference wasn’t detected in sexual parameters in conservative treatment and surgical repair groups in this study. Additionally, since a significant degradation was detected in sexual function parameters even in conservative treatment cases without sudden detumescence and with suspicious linear tunica albuginea rupturing, we think that quick surgical exploration would be useful in cases considered to have penile fracture. We also think that an awareness should be formed on penile fractures in primary health care institutions and society due to the importance of early treatment.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Authors’ contributionsConceptualization: HHT, MGS and GE. Funding acquisition: HHT. Methodology: HT, MGS, GE and HU Supervision: HT, MGS Writing-original draft: HHT, MGS, AA, MB. Writing-review & editing: all authors.
Ethics statementAll procedures performed in this study involving human participants were conducted in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Consent according to the Helsinski declaration was taken from Necmettin Erbakan University Meram Faculty of Medicine ethics committee before the study (No: 20202519).
FundingThis research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interestsThe authors declare that there is no conflict of interest.