Aspergillus flavus and Aspergillus fumigatus are commonly involved in fungal endophthalmitis. However, other less pathogenic species of the genus are also causal agents of opportunistic infections. Aspergillus hiratsukae, a species within Aspergillus section Fumigati, is an uncommon fungus responsible for a few infectious cases worldwide.
Case reportWe present a case of post-surgical endophthalmitis in a man caused by A. hiratsukae after phacoemulsification surgery and intraocular lens implantation. The patient underwent an urgent vitrectomy in which infectious foci were observed. Due to adverse clinical evolution, evisceration was performed five days after admission. In the study of the intraoperative samples fungal growth was observed. Microscopic analysis showed conidial heads resembling Aspergillus species. The final identification of A. hiratsukae was achieved by amplifying and sequencing the ITS1-5.8S-ITS2 spacer region. Antifungal susceptibility testing was performed using the method described by EUCAST. The isolate exhibited sensitivity to azoles and polyenes.
ConclusionsDue to the morphological similarity of the Aspergillus species, molecular techniques are essential for discriminating among them, as there are different antifungal susceptibility profiles within the same complex. Further studies to improve clinical surveillance, make an early diagnosis and start a targeted therapy are necessary.
Aspergillus flavus y Aspergillus fumigatus son patógenos habitualmente implicados en la endoftalmitis fúngica. Sin embargo, otras especies menos patógenas del género también son capaces de producir infecciones oportunistas. Aspergillus hiratsukae, especie perteneciente a la sección Fumigati de Aspergillus, es un hongo infrecuente del cual se han informado unos pocos casos de infección en todo el mundo.
Caso clínicoPresentamos un caso de endoftalmitis postquirúrgica causada por A. hiratsukae en un hombre tras cirugía de facoemulsificación e implante de lente intraocular. Al paciente se le realizó una vitrectomía urgente, pero la mala evolución derivó en la evisceración a los cinco días del ingreso. En las muestras intraoperatorias se observaron cabezas conidiales compatibles con Aspergillus. La identificación final de la especie A. hiratsukae se realizó mediante amplificación y secuenciación de la región espaciadora ITS1-5.8S-ITS2. La sensibilidad del aislamiento a los antifúngicos se valoró mediante el método descrito por EUCAST. La cepa mostró sensibilidad a los azoles y a los polienos.
ConclusionesDebido a la similitud morfológica de las diferentes especies del género Aspergillus la discriminación molecular es fundamental, ya que la sensibilidad a los diferentes antifúngicos puede variar entre especies. Avanzar en el estudio de estos patógenos es necesario para mejorar la vigilancia clínica, el diagnóstico temprano y la instauración de una terapia dirigida.
Fungal endophthalmitis, a serious ocular infection, is one of the leading causes of visual loss worldwide.5 Postoperative or traumatic injuries and immunosuppressed status are the main risk factors associated with these infections.8 It is well known that Aspergillus species are closely related to fungal endophthalmitis, mainly associated with exogenous processes.9 Although Aspergillus flavus and Aspergillus fumigatus are responsible for most cases, opportunistic infections caused by other species of the genus have been described.15 Historically, teleomorph members of the genus have been considered microorganisms with lower pathogenic capacity due to lower production of asexual spores than their anamorphic relatives.13 The uncommon fungus Aspergillus hiratsukae, a species belonging to Aspergillus section Fumigati, is the cause of a few infectious cases in humans worldwide.13,10,17
In this report, we present a case of post-surgical endophthalmitis caused by A. hiratsukae in a 75-year-old male with an intraocular lens implant. The patient was referred to our center with the suspicion of left eye (LI) endophthalmitis after undergoing epiretinal membrane removal with phacoemulsification surgery, intraocular lens (IOL) implantation and vitrectomy at a private institution 3 weeks before. A week after surgery, the patient reported pain and reduced visual acuity, so an urgent vitrectomy was done and intravitreal injections of unspecified antibiotics were given. Due to the unfavorable evolution, the patient was referred to our hospital. On arrival, visual acuity in the LI was 0.01. Examination revealed an edematous cornea accompanied by abundant anterior chamber cellularity (cell 4+) and hypopyon 1mm. Posterior iridian synechiae and a retrolental inflammatory membrane were also observed.
The intraocular pressure of the LI was 11mm Hg and the surgical incisions were watertight. Due to an intense vitritis, the condition of the posterior pole could not be checked by funduscopic examination. An ultrasonography confirmed the presence of a dense and poorly mobile hyperechogenic material filling the vitreous. Given the high suspicion of post-surgical endophthalmitis, an urgent vitrectomy was scheduled. A very dense vitritis was observed, as well as infectious foci at the base of the vitreous with hemorrhages in the posterior pole and evidence of retinal ischemia. Abundant cotton-wool spots adjacent to and inside the IOL-sac complex were observed and explanted. An iridian plastron was also visible under the main incision of the phacoemulsification surgery. The treatment consisted of intravitreal injections of ceftazidime, vancomycin and voriconazole every 48h. Given the fulminant evolution and the severity of the clinical manifestations, evisceration of the LI five days after admission was performed.
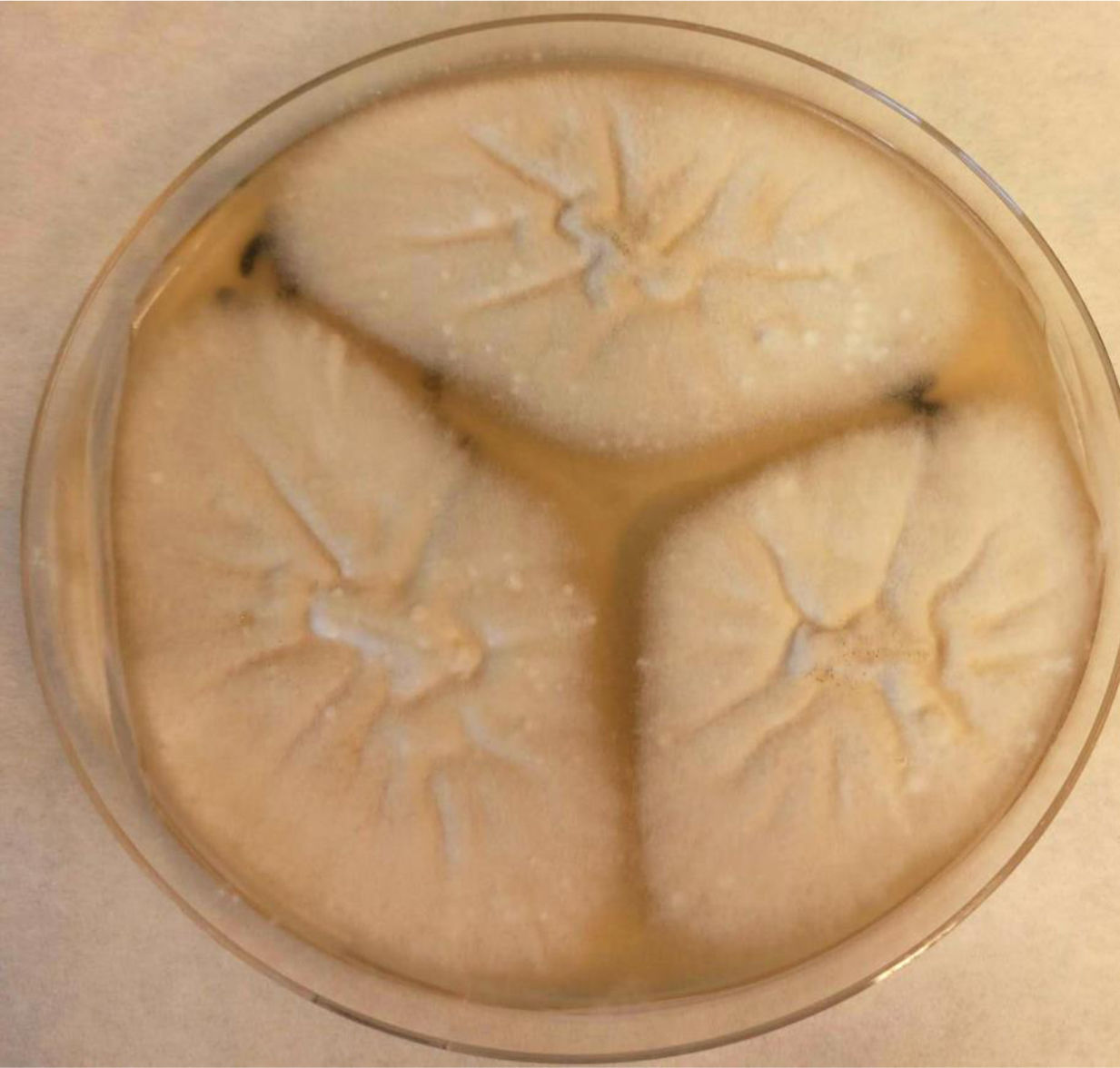
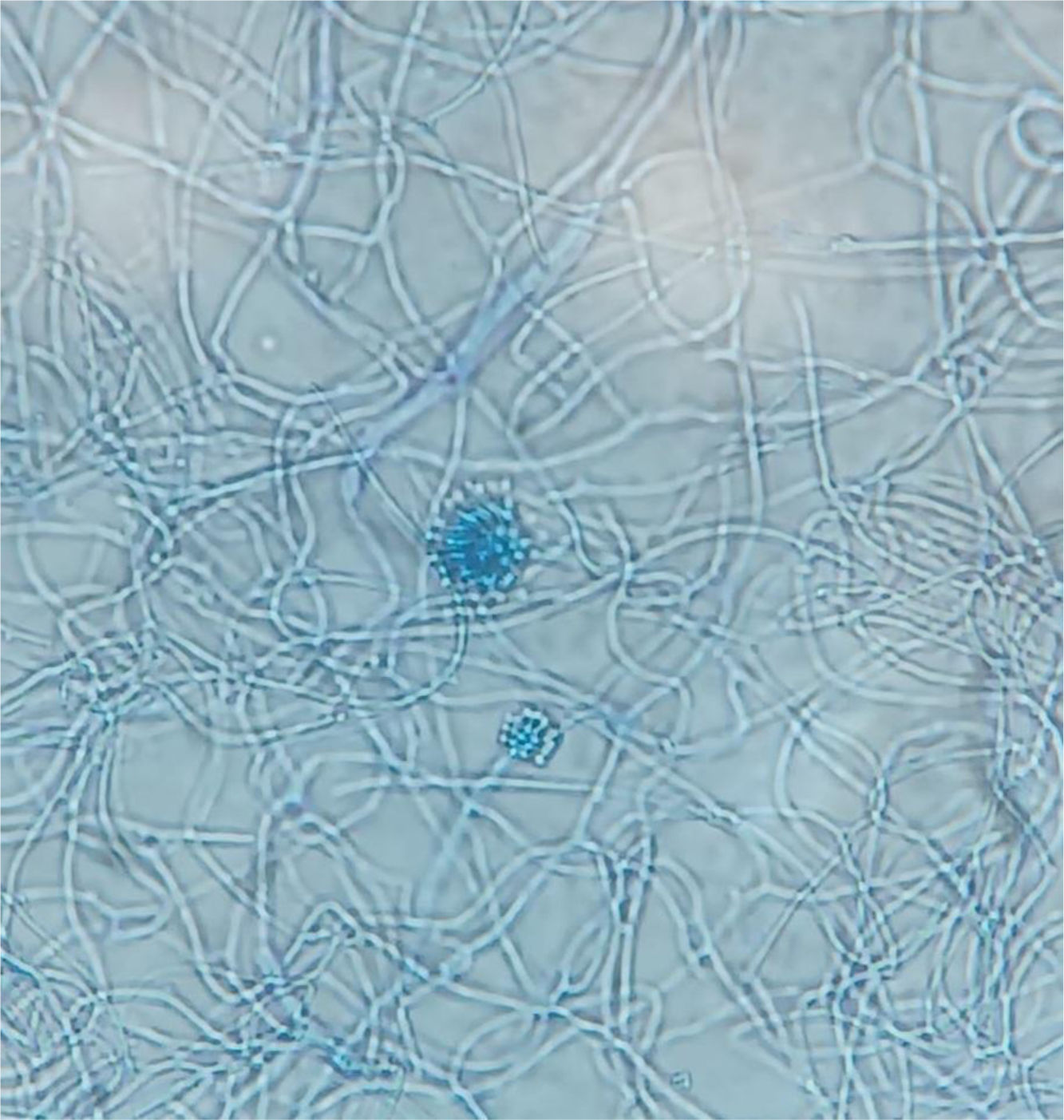
Samples of vitreous humor, aqueous humor and the IOL carried by the patient, all taken during the vitrectomy, were subjected for culture. After evisceration, two samples of infected intraocular tissue were also submitted to the laboratory. After 7 days of incubation at 30°C, a fungal growth in the brain heart infusion broth medium of the intraocular lens was observed, as well as in one of the tissue samples. Subcultures on Sabouraud and potato dextrose agar grew after 3 days (Fig. 1). Microscopically, conidial heads suggestive of Aspergillus were observed. Preparation with lactophenol blue revealed septate hyaline hyphae with smooth-walled conidiophores and spherical vesicles. The conidiogenous cells were uniseriate and covered the upper two thirds of the vesicles (Fig. 2). The final identification was achieved by amplifying and sequencing the ITS1-5.8S-ITS2 spacer region (using ITS1 and ITS4 primers), and the ribosomal large subunit D1–D2. The amplified fragments were processed on the Applied Biosystems 3500/3500XL Genetic Analyzer sequencer (Applied Biosystems), and the consensus sequences were used for local alignment by Basic-Local-Alignment-Search-Tool (BLAST), obtaining the definitive identification of A. hiratsukae. The strain is available for consultation at the National Microbiology Center under the accession number CNM-CM11416. The ITS sequence was deposited in the GenBank database with the accession number PQ164401.
Antifungal susceptibility testing was performed at the National Microbiology Center using the method described by EUCAST for conidia-forming molds. The minimum inhibitory concentration (MIC) values obtained were the following: itraconazole, 0.5mg/L; voriconazole, 1mg/L; posaconazole, 0.12mg/L; isavuconazole, 0.5mg/L; terbinafine, 1mg/L; micafungin, 0.25mg/L; caspofungin, 0.008mg/L; anidulafungin, 0.008mg/L; and amphotericin B, 1mg/L. These MIC values are similar to those described for A. hiratsukae,6,13 with a noteworthy susceptibility to azoles. However, some sporadic high MIC values for itraconazole have been reported in the literature.17 Thus, this susceptibility pattern contrasts with that of other species of the Fumigati complex, such as Aspergillus udagawae and Aspergillus lentulus, in which resistance to triazoles has been frequently reported.11
In a multicenter review conducted in Asia,4 two thirds of the patients with endophthalmitis due to Aspergillus species saved the eye. The factors associated with a better prognosis were the absence of corneal infiltrate, better visual acuity than that within the handmotion scale range, and primary vitrectomy. However, in Aspergillus endophthalmitis the presence of vitritis is common,7 as well as the invasion of the choroidal and retinal vessels, lack of retinal tissue organization and hypopyon.14,1
Voriconazole is the antifungal of choice to fight against infections caused by most species of the genus, as MICs are low and there are fewer adverse effects than those with amphotericin B, although some authors have proposed using them in combination.18 In our case, although the patient received voriconazole, the presence of severe vitritis associated with low visual acuity and the need to perform a second vitrectomy resulted in the final evisceration of the eye. Despite the presumably lower pathogenicity of some members in Aspergillus section Fumigati, complicated ophthalmologic infections associated with these species have been described in the literature, including a severe corneal infection by A. udagawae12 and a post-traumatic keratitis caused by Aspergillus fischeri that progressed to endophthalmitis and evisceration of the eye.3
In addition to an appropriate clinical management, a correct identification of the fungus is essential in the control of these infections. Molecular identification techniques are imperative in the discrimination of cryptic Aspergillus species. The species described within the different sections, such as Fumigati, Usti and Nigri, are highly similar in their morphological characteristics, sometimes indistinguishable, but different antifungal susceptibility profiles may exist within the same complex. Some studies describe the presence of up to 10% of cryptic species in clinical samples, which is likely to increase due to advances in molecular taxonomy.2 In the particular case of A. hiratsukae, the sequencing of the ITS spacer region is essential for the identification of the species. PCR amplification, and the subsequent partial sequencing of the β-tubulin, calmodulin and rodlet A genes, have also been proposed as a complement to the identification.16 Furthermore, A. hiratsukae has been routinely isolated from the environment and has been reported in Intensive Care Units,13 so further investigations on its geographical distribution and environmental control are necessary for the prevention of nosocomial infections.
In short, it is necessary to advance in the study of these emerging pathogens to improve clinical surveillance, establishing an early diagnosis, and starting a timely targeted antifungal therapy.
Financial supportsThe authors declare that they did not receive any grant from public, private or non-profit funding agencies for this research.