When Marjorie Warren started to manage older patients in ways different than other practitioners of health care, two main characteristics of this new way of doing the things became clear.1,2 The first was the focus on functional status instead of clinical diagnoses and the second was a focus on developing a response to the high complexity at the interface of ageing, chronic disease, life styles and social environment.
Since that early alteration in practice patterns, it has become clear that functional deterioration was the best marker of adverse events in older adults, and among the first conditions associated with a poor quality of life.3,4 It was also increasingly evident that being disabled markedly decreased the chance of recovering towards robustness. This is especially true as the disability becomes more severe and it is firmly established.5
When considering the pathophysiological basis of functional impairment, this observation makes sense: the same factors that likely cause disability and the loss of functional reserve, are likely the main obstacles for the recovery.6,7 Taken as a whole, the prognostic value of disability and its difficulty for recovery, moved the focus from diagnosing and managing disability towards the pre-disability conditions. This new focus allows preventive strategies to be developed. As in many realms of medicine, where the identification of risk factors and their treatment are among the most successful strategies (such as reduction in risk factors for cardiovascular disease, or cancer screening tools). This is also the case for both disability and frailty, and a useful paradigm for the development of appropriate strategies for the management of predisposing conditions of disability and frailty.
Disability and frailty are different, often overlapping, stages of the same disabling process.8,9 With increasing age, the changes in several physiological systems augment our vulnerability to even minor stressors.10 When this difficulty in maintaining our internal homeostasis in response to stressors overcome a threshold, the likelihood of becoming disabled and dependent increases in a logarithmic way. This likelihood becomes a certainty when we overcome an indeed lower threshold, below 30–35% of our functional capacity.6 In a very synthetic way, without putting names to the facts, this is the most likely pathway that leads from robustness to the most severe disability. This pathway certainly includes age and chronic disease as the main etiologic factors, as well as environmental and socioeconomic conditions as its main modulators.
The gradual advancement of disability with increasing age has provided a conceptual framework to the theory and practice of Geriatric Medicine since its early days. Indeed, several terms and names for designating the several stages towards disability have been developed over the past several years. Terms related to function like functional reserve, intrinsic capacity, resilience, physical and cognitive impairment or decline, frailty, disability and some others have come into common use over the past few decades.
Although most of these terms are recognized and commonly used by health care providers, most do not have exacting definitions. Frailty is a good case in point. Although dozens of screening and measurement tools for frailty have been developed, minimal consensus around formal definitions of frailty have been obtained and most validated tools have only been utilized for risk assessment in population studies.11–13
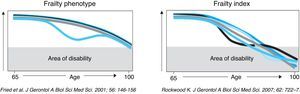
Over the past decade, two main conceptual frameworks for the term frailty in the Geriatric literature have arisen (Fig. 1).11,14
- 1)
Frailty Index: In this model, frailty is a process driven by increasing illnesses and conditions (i.e. deficits) that in sum lead to frailty, that it is clinically manifest by the presence of added deficits and that it is measured using an index or collection of related or unrelated variables, without a clear cut-off point.15–17 In the clinical practice, the assessment of function, cognition, multimorbidity and geriatric syndromes, sense organs, polypharmacy and social items is aggregated to get an index score.
- 2)
Frailty Phenotype: This is hypothesized to stem from a deeply biological process that specifically drives the vulnerability to chronic illnesses and disability. Frailty in this sense reflects the progressive deterioration of the underlying physical substrate and hence functional capacity of human beings. In this conceptual framework, frailty is a stage in the disabling process, that is clinically manifest by the presence of a deterioration in physical performance and energy levels, and that often precedes the development of disability. It was initially operationalized using core signs and symptoms of fatigue, weight loss, weakness, slowness, and low activity level using clear cut-off points.8
In the article by Amblas et al. in this issue of Revista Española de Geriatría y Gerontologia,18 the frailty index model is utilized. Each frailty measurement is a combination of items, that can change according to the setting and the characteristics of the population. Although indexes are a useful way to aggregate a wide variety of co-morbidities, biological changes, and socioeconomic factors into a risk assessment tool, such tools do not add a significant improved prognostic value to the usual, very classic instruments that geriatricians have used over the past decades, including components of the Comprehensive Geriatric Assessment (CGA). This tool, developed, evaluated and disseminated in the last decade of the past century19 describes and embraces the characteristic complexity of the multiple conditions that can afflict older adults. As the index tools described in Amblas et al. collect and assemble well-established predictors of poor outcomes, they are in the end robustly able to predict poor outcomes. Thus, although potentially useful in clinical settings for measuring risk and showing it in a simple way,20 they are not able to challenge or produce change in the conceptual framework of the classical approach of Geriatric Medicine to the evolution of disability. In fact, because of the nature of the frailty index approach, these tools are not able to detect those older people at risk for developing disability. Hence, these tools do not provide for new approaches to the conceptual problem of what functional decline is, how it is produced and how it can be detected and managed in their earliest stages. These indexes in fact leave the matter of pre-disability detection and management unaddressed. Indeed, the critical need to find tools that help us to better identify those older people still functioning but at risk of developing functional decline remains, along with a better understanding of the biology that drives this decline. This is a population that represents nearly 50% of older people, showing the best response to interventions oriented to mobility or disability,21–23 in contrast to the 5–10% of older people suffering from significant disability. Thus, the main value of finding a pre-disability condition that is easy to recognize and with potential for intervention is to avoid the development of disability in a timely fashion. As John Maynard Keynes established, making predictions is very easy: in 100 years, everybody will die. But the purpose is to predict in the proper time, when we are still in conditions to avoid significant outcomes, including disability.
At the same time of the building of the first “Frailty Index”,15 a seminal article about a condition able to predict the risk of incident disability was published.8 The authors named this condition “frailty”, a term that had been largely used in the geriatric literature in a poorly precise way, and described a typical phenotype for this condition that provided accuracy in the characterization of the patients. Moreover, they established that this newly phenotype condition was different from comorbidity and, mainly, different from disability (as assessed by ADL dependency), in that it was present in only 27.5% of the frail people. It also predicted mobility impairment and the development of disability. In addition, they also proposed a pathophysiological framework, called the cycle of frailty.
Since then a great number of new findings has built a solid biological construct that overcome the restricted concept of a diagnostic or a prognostic tool to become a condition that is the most powerful factor predicting the risk of disability in older people who are not disabled and hence the target for several successful interventions.24 And this is what makes this concept of frailty of interest. In our view, the concept of frailty stemming from the phenotype is most useful as it adds something that (a) identifies those at the highest risk for developing disability, (b) enables the detection of patients with symptoms subtle enough, like a poor performance in tasks like gait velocity, balance or muscle strength in non-disabled people, for remaining undetected using the classical approach, (c) allows a change from the reactive management of disabilities to one of proactive prevention of disability. This is in part accomplished because phenotype measurement tools exclude disability measures when assessing for frailty, and attempts to identify at risk individuals rather than those that are already disabled as in the index approach.
With this conceptual framework in mind it is obvious that the frailty phenotype is well fitted for these purposes. Different from the multiple comorbidities or disabilities included in most index type measurements of frailty, a well-defined pathophysiological construct is increasingly being demonstrated to underlie the frailty phenotype. The identification of dysregulation in inflammation, energy balance, muscular-skeletal system, and some hormonal axes, as well as a firmly established criteria for screening and diagnoses in different ambulatory care settings and specific therapeutic strategies being developed to target that biology, the use of the frailty phenotype and its biological underpinnings represent the most important approach to decreasing the percentage of older people with incident disability and for potential improvement in the quality of life. In addition, the frailty phenotype and its biological underpinnings are also important prognosticators of other adverse outcomes like death, falls or hospitalization. These other outcomes are also predicted by many other factors like disability, multimorbidity, poor social conditions, and geriatric syndromes like delirium or immobility, all of them very well known since the past century, but showing limited opportunities for intervention.
Despite substantial progress in the field of frailty research, it is necessary to develop new knowledge on many aspects of this clinical syndrome.24–26 Among the most urgent ones is the need to more definitively clarify the conceptual misunderstanding between the index and phenotype concepts of frailty. The fact that these two vastly different concepts share the same name has hampered the improved knowledge of the main etiologies that underpin the development of disability. This clarification will help to differentiate the populations where Frailty Indexes and Frailty Phenotype should be used, because they probably respond to the needs of populations with separate characteristics.25,27 This differentiation will allow substantial progress in the field regarding the risks, the diagnostic tools, the prognosis, the management and the response to several interventions, making more feasible the broad implementation of a clinical transition that promotes the approach to aged patients according to their functional issues rather than their specific diseases and co-morbidities.28