Hypercalcemia is a rather common finding (up to 39 cases per 1000 inhabitants1), and when detected, a differential diagnosis must be made between hyperparathyroidism and malignancy, which together are responsible for over 90% of all cases. Clinically, hypercalcemia can be the cause of diverse neurobehavioral symptoms, ranging from lethargy, depressed mood, psychosis and cognitive dysfunction.2 The exact prevalence is not well defined due to the lack of rigorous assessment, the small size of the studies, and the wide variations in the instruments used to assess such disturbances. Depending on both the calcium concentration as well as the speed with which it was acquired, this disease can be life threatening, but yet, treatable during early stages, and thus, a high index of suspicion is required.
We herein report a case of a 78-year-old Caucasian woman who presented in the emergency department with progressive decline of consciousness in the last couple of weeks. Relevant personal history included arterial hypertension, diabetes mellitus type 2, hypothyroidism, osteoporosis, Alzheimer's disease was diagnosed 3 years ago and she was partially dependent in activities of daily living (Global Deterioration Scale – GDS of 6). Our patient also presented with changes in bowel habit since the last 2 years, having underwent a recent endoscopic and CT scan study, revealing only normal findings. Her usual treatments included enalapril–hydrochlorothiazide 20mg/25mg od; levothyroxine 25mcg od, metformine/linagliptine 850mg/2.5mg bid and galantamine 8mg od.
The family revealed that after one month, and after having passed a respiratory tract infection, treated with quinolones during 2 weeks, our patient experienced a progressive deterioration of her general health status, associated with confusion, nausea, vomiting and worsening of her physical dependence.
The physical examination revealed no abnormalities, except for a deterioration of consciousness and a slight dehydration of skin and mucosae. Laboratory workup only showed glucose level of 130mg/dL [range: 70–100], and corrected calcium level (with protein) of 14.2mg/dL [range: 8.5–10.6]. The ECG showed a sinusal rhythm, without any other conductive abnormalities. The patient was admitted and treatment with intravenous fluids and loop diuretics was initiated. Her usual antihypertensive treatment with hydrochlorothiazide was discontinued.
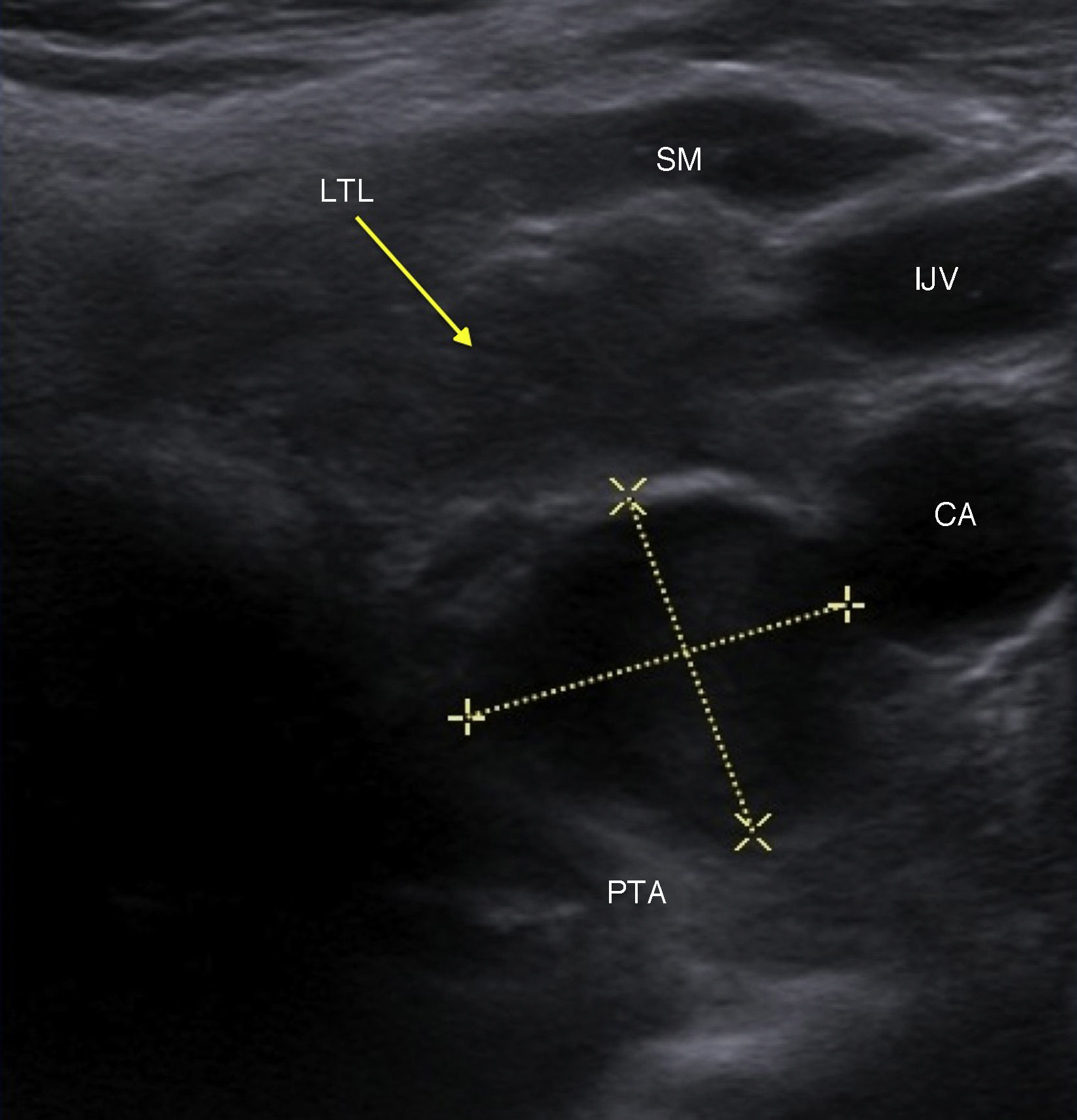
Forty-eight hours after, she exhibited an acutely cognitive improvement (GDS of 4), together with a normalization of the serum calcium level (10.9mg/dL). The rest of the analysis revealed phosphorus level of 1.3mg/dL [range: 2.4–4.1], 25-OH-d level of 4.5ng/mL [range: 30–74], parathormone of 251.10pg/mL [range: 10–65pg/mL], calciuria 150mg/24h [range: 100–300]. We performed a point-of-care ultrasound of the thyroid, which showed a well-defined hypo-echoic nodular lesion, measuring 14mm×12mm×18mm (H×W×D) and located in the left posterior inferior thyroid lobe (see Fig. 1 and Video 1).
Supplementary Video 1 related to this article can be found, in the online version, at http://dx.doi.org/10.1016/j.regg.2015.07.011.
Hyperparathyroidism due to parathyroid adenoma was diagnosed on the basis of these results. Reviewing the patient's personal history, we noted that the last two years prior to her recent admission, she had presented herself on various occasions to the emergency department, fundamentally with neurological or gastrointestinal symptoms. We also observed elevated calcium levels since 2013 (10.6mg/dL), without the subsequent initiation of a specific treatment. After obtaining clinical stability, the patient was discharged from the hospital, and she is currently on a waiting list for parathyroid adenoma resection and a neuropsychological reevaluation.
Secondary hypercalcemia caused by parathyroid adenoma can present itself with a wide range of clinical manifestations, although it tends to lead a chronic and mild course, only rarely requiring urgent hospitalization.
In the diagnostic evaluation, ultrasound can be of use, when employed to localize and evaluate parathyroid glands. It's a sensitive, non-invasive and reproducible test, and it permits an evaluation of concomitant thyroid pathology (present in 20–30%), which could modify the surgical treatment.3 Typically, adenomas are identified as homogenous hypo-echogenic lesions.
A recently published study analyzed a series of cases with hypercalcemia attended in the emergency department.4 They found that up to 81% of patients were symptomatic, although only 3.5% were diagnosed with hyperparathyroidism and up to 24% of patients had no follow-up plan at the time of discharge. With an estimated prevalence of 20%, we are probably dealing with an underdiagnosed disease.
Global cognitive decline in the elderly due to parathyroid adenoma it is remarkably underdiagnosed, since changes in behavioral and cognitive function are usually attributed to aging, dementia and frailty, which makes the diagnosis challenging. Nevertheless, because many of these patients could benefit from a medical or surgical treatment, as was the case in our patient, it would be advisable to integrate emergency department and care pathways and protocols, in which point-of-care ultrasound could be of great importance to standardize practice.
Conflict of interestNo potential conflicts of interest were disclosed.