To determine if subchondral bone damage can influence the clinical results of intraarticular platelet-rich-plasma (PRP) treatment in knee osteoarthritic patients.
Material and methodsA retrospective review of patients treated with intraarticular PRP injections for knee osteoarthritis who previously underwent a magnetic resonance (MR) of the knee was performed. Visual Analogic Score (VAS) was assessed for pain, whereas WORMS MR score was adapted to assess the damage to the subchondral bone (WORMSsc score).
ResultsSixty-one patients were treated with 3 weekly injections of PRP. Mean VAS reduction was 27.67±13.13 points (p<.005). WORMS sc mean score was 32±18.5 points. No correlation between WORMSsc and VAS was found. A moderate correlation between WORMSsc score and preoperative VAS was found (r=.43; p<.005).
ConclusionThere is no correlation between the damage to the subchondral bone assessed by MR and pain relief at 12 weeks in patients treated with intraarticular platelet-rich plasma in patients with knee osteoarthritis. A greater damage to the subchondral bone could be associated with more pain.
Determinar si las lesiones en el hueso subcondral en la artrosis de rodilla pueden condicionar el resultado del tratamiento con plasma rico en plaquetas (PRP) intraarticular.
Material y métodosSe revisó retrospectivamente a los pacientes con artrosis de rodilla tratados con PRP intraarticular sometidos previamente a una resonancia magnética (RM). Se evaluó la escala visual analógica (EVA) y las imágenes de resonancia mediante una adaptación de la escala WORMS graduando el daño al hueso subcondral (WORMSsc).
ResultadosSe estudiaron 61 pacientes tratados con PRP intraarticular en 3 sesiones. Se obtuvo una mejoría en la escala EVA de 27,67±13,13 puntos (p<0,005). La puntuación de los ítems de la escala WORMSsc fue de 32±18,5 puntos, no encontrándose correlación con la escala EVA. Se encontró una correlación moderada (r=0,43; p<0,005) entre la escala WORMSsc y la escala EVA pretratamiento.
ConclusionesNo existe correlación entre el resultado clínico a las 12 semanas y el daño del hueso subcondral evaluado mediante RM en los pacientes con artrosis de rodilla tratados con PRP intraarticular. Un mayor daño del hueso subcondral podría estar asociado con mayor dolor.
Osteoarthritis is a very common disease and a recognised cause of pain and disability in the population. Recent studies in Spain have estimated the prevalence of osteoarthritis of the knee in the general population to be around 13%, with a higher incidence in women, in people who are overweight and obese, and with age.1 Treatment of osteoarthritis of the knee includes pharmacological treatment, physical therapy, joint injection and, ultimately, joint replacement surgery.2 Of the intra-articular infiltrations, there is extensive clinical experience with corticosteroids and hyaluronic acid, and blood-derived biological products such as platelet-rich plasma (PRP) appear to show promising results and their clinical use is increasing. However, the scientific evidence is controversial in some cases and there is still no consensus between the recommendations of different societies regarding the ideal formulation, dosage, or administration frequency, or the physiological mechanism by which it promotes clinical improvement in patients.3
Osteoarthritis of the knee is characterised by the classical radiological findings of reduced joint space, the presence of subchondral geodes and cysts, osteophyte formation, and sclerosis of the subchondral bone. The introduction of magnetic resonance imaging (MRI) for the diagnosis of knee osteoarthritis has made it possible to obtain more detailed information on the shape and distribution of osteophytes, the state of the subchondral bone, and the presence of cartilage and bone marrow changes at time of diagnosis. This has led to the development of scoring systems to assess MRI findings in osteoarthritis of the knee, such as the Whole-Organ Magnetic Resonance Score (WORMS), which was developed in 2004 as a semi-quantitative method of assessing the condition of the osteoarthritic knee for use in epidemiological studies and clinical trials.4 Several authors have been interested in the role of MRI as a predictor of patient prognosis and the outcome of orthobiologic therapy.5–8
Subchondral bone has gained importance in recent years as its involvement in osteoarthritis of the knee has become more widely understood. Subchondral bone comprises the bone tissue down to the calcified layer of the subchondral plate, and is involved in processes of homeostasis, weightbearing, and cartilage nutrition.9 Articular cartilage disorders also include a number of changes in the subchondral bone that result in changes that influence the progression of knee osteoarthritis. Some of these changes, such as the presence of bone marrow lesions, appear to be associated with worsening of the condition and the need for knee replacements in the future.7 For this reason, a combined approach to this type of lesion has been proposed within the field of orthobiologics, using both joint and subchondral bone treatment.10 However, the efficacy of combined intra-articular and intra-osseous therapy compared with intra-articular treatment, the best biological treatment, and the doses and administration frequency are still to be determined.
Given the role of subchondral bone in knee osteoarthritis, it could be suggested that the presence of such lesions may reduce the efficacy of intra-articular PRP infiltration in knee osteoarthritis. Some authors associate the presence of bone marrow lesions with poorer outcomes of biological treatments.5,8 However, other subchondral bone lesions that can be found in radiological assessment scales have not been studied.
The aim of the present study is to quantitatively analyse subchondral bone damage on MRI in patients with osteoarthritis of the knee, and to determine whether there is a negative correlation between the presence of this damage and the outcome of treatment with intra-articular PRP.
Material and methodsPatient selectionWe conducted a retrospective review of a selection of patients treated with PRP infiltrations for osteoarthritis of the knee at our centre between 2023 and 2024. Patients were selected for the retrospective review if they had osteoarthritis of the knee and had undergone MRI prior to admission for treatment. Patients with post-traumatic osteoarthritis, patients with previous surgery on the affected knee, and patients with concomitant rheumatic disease were excluded.
All the patients were included for treatment after they gave their express consent. After screening for blood-borne diseases, the patients were scheduled to start treatment.
Platelet-rich plasma treatmentAll patients underwent 3 sessions of intra-articular PRP infiltration into the affected knee, one week apart. Twenty ml of peripheral blood was collected and centrifuged at 8000rpm and the platelet fraction was isolated in a laminar flow hood. A total of 8ml of platelet concentrate without leucocyte fraction was used, after prior activation with 3ml of calcium chloride.
The patients were discharged after each infiltration and were advised to apply cold, keep the knee relatively still for 24h after the injection, and to avoid anti-inflammatory drugs during the entire treatment period. After the third infiltration, the patients were scheduled for a 12-week follow-up with their treating physician.
The patients’ pain was assessed using a visual analogue scale (VAS) at baseline and at 3 months after treatment, and improvement was measured as the difference in score between baseline and end of treatment (DifVAS).
To confirm that the effect of PRP treatment was not due to chance, a control group with similar demographic characteristics to the study group was established, treated conservatively with a corticosteroid infiltration of 2mg betamethasone. Patients were assessed at 3 months using the same pain parameters as the study group.
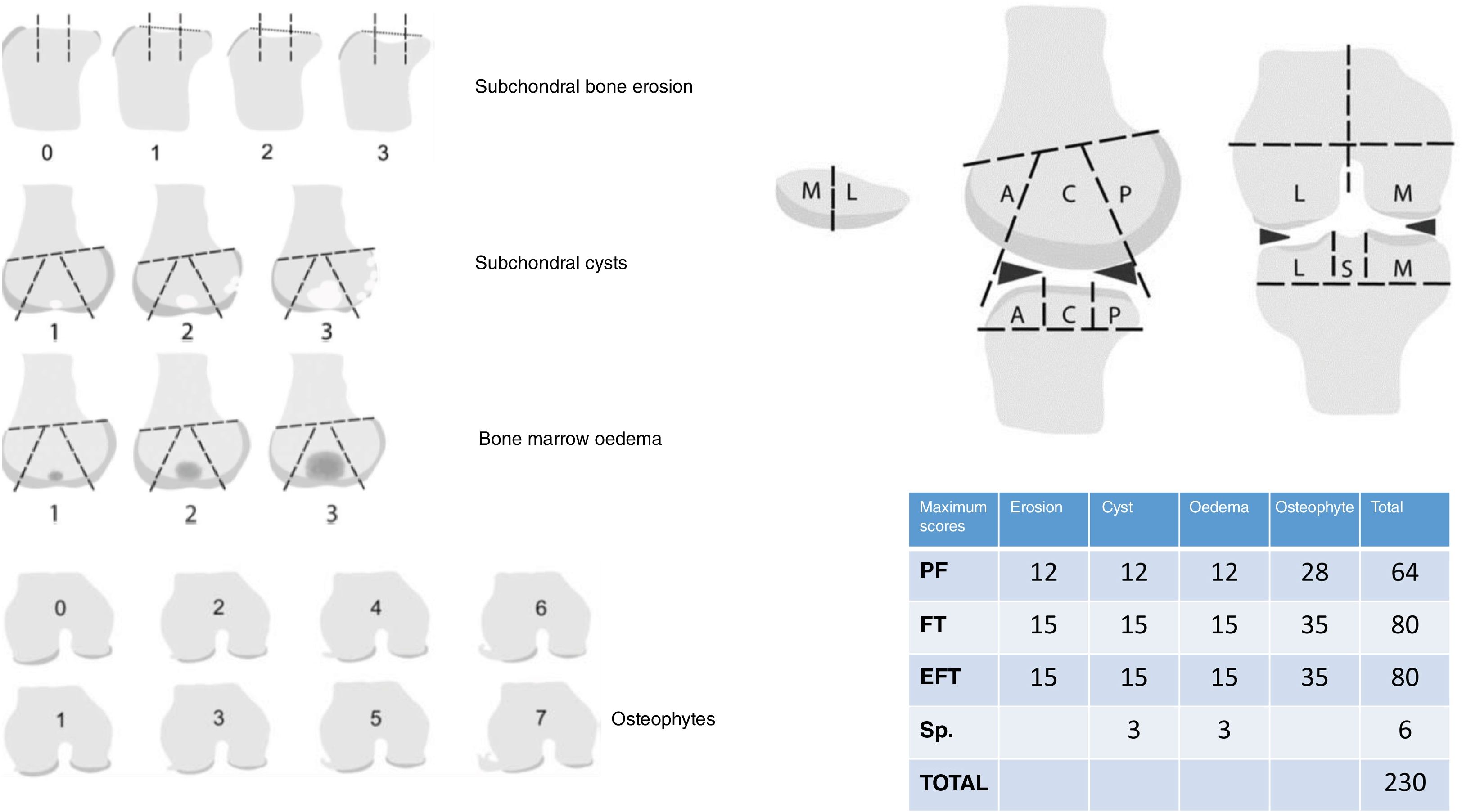
MRI and adapted WORMS scaleAt the time of inclusion for treatment the patients had been assessed by MRI. The WORMS scale was used to assess the subchondral bone status prior to treatment. To simplify the review and to focus on the subchondral bone, the WORMS score was adapted to include only the 4 items that score subchondral bone status (WORMSsc): cyst formation, bone marrow lesions, subchondral bone attrition, and shape and size of marginal osteophytes. These items were scored on each patient's MRI following the division of the knee into areas suggested by the WORMS scale (Fig. 1).
Modified WORMS assessment scale using only the aspects related to the subchondral bone (WORMSsc). Aspects related to the left side (bone erosion, bone oedema, presence of cysts, and appearance of osteophytes) are measured according to the drawings for each item, scoring each in the following areas of the knee: condyles (subdivided into anterior [A], central [C], and posterior [P] area), plateaus (subdivided into anterior [A], central [C], and posterior [P]), patellofemoral (medial [M] and lateral [L]), and tibial spines (S). The maximum possible scores are listed in the table below right. EFT: external femorotibial; IFT: internal femorotibial; PF: patellofemoral; Sp: spines.
Statistical analysis was performed on a database in Excel® (Microsoft Corporation, California, USA) with the help of an artificial intelligence model based on Chat GPT 4.0 (www.OpenAI.org).
The Student's t-test was used to compare VAS values pre and post treatment. Analysis of variance was used to compare pain improvement with respect to the Ahlbäck scale. The distribution of the WORMSsc values did not pass the normality tests, so the Kruskal–Wallis test was used to compare between the WORMS and Kellgren scores. A correlation analysis was also performed between the WORMSsc total score, the VAS scores, and the improvement in the patients’ pain (DifVAS) using Spearman's test.
Moreover, a multiple linear regression analysis was performed to try to demonstrate the influence of each of the WORMSsc items on the DifVAS variable.
For all tests, a value of p=.05 was used to indicate statistical significance.
ResultsA sample of 61 patients with osteoarthritis of the knee treated with PRP infiltration in our centre between January and August 2023 was selected.
Thirty patients were female, and 31 patients were male. Thirty-seven (60.66%) were right knees and 24 (39.34%) were left knees.
Regarding radiological knee involvement according to the Ahlbäck scale, 12 subjects (19.67%) were a grade 1, 28 subjects (45.9%) grade 2, 18 (29.51%) grade 3, and 3 (4.92%) grade 4. The mean WORMSsc score of the sample was 32±18.5 (1–98).
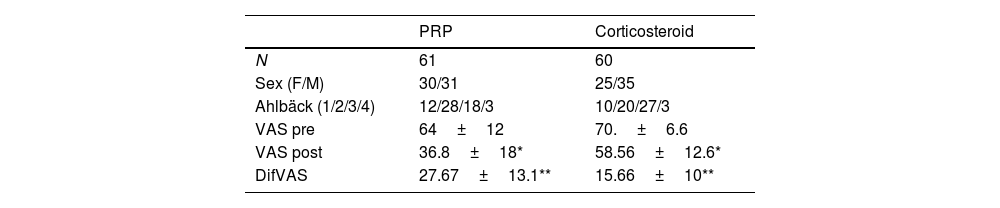
Mean pre-treatment pain measured on the VAS scale was 64.61±12.79 (32–85). At 3 months after the end of treatment, the mean VAS score was 36.8±18.45 (5–94). The mean DifVAS was 27.67±13.13 points (−10 to 56). Statistically significant differences were found between pre- and post-PRP infiltration VAS with a p<.005. The control group consisted of 60 patients with a mean age of 64.5 years, treated with corticosteroid infiltration. The proportion of different grades of radiological involvement was similar to the PRP group. The mean pre-treatment VAS score was 74±6.61 and the post-treatment VAS score was 58.6±12.6. In both groups there were significant differences before and after treatment with a p<.05. The mean VAS difference for the corticosteroid group was 15.66±10 points. When comparing the degree of improvement of both groups, significant differences were found (p<.005) suggesting that the effect of PRP was superior to that of corticosteroids at 12 weeks (Table 1).
Comparison of the cohort of patients treated with PRP with the control group treated with corticosteroid infiltration.
| PRP | Corticosteroid | |
|---|---|---|
| N | 61 | 60 |
| Sex (F/M) | 30/31 | 25/35 |
| Ahlbäck (1/2/3/4) | 12/28/18/3 | 10/20/27/3 |
| VAS pre | 64±12 | 70.±6.6 |
| VAS post | 36.8±18* | 58.56±12.6* |
| DifVAS | 27.67±13.1** | 15.66±10** |
VAS post: VAS at 12 weeks of treatment; VAS pre: VAS prior to treatment; DifVAS: difference between VAS scores pre and post; PRP: platelet-rich-plasma.
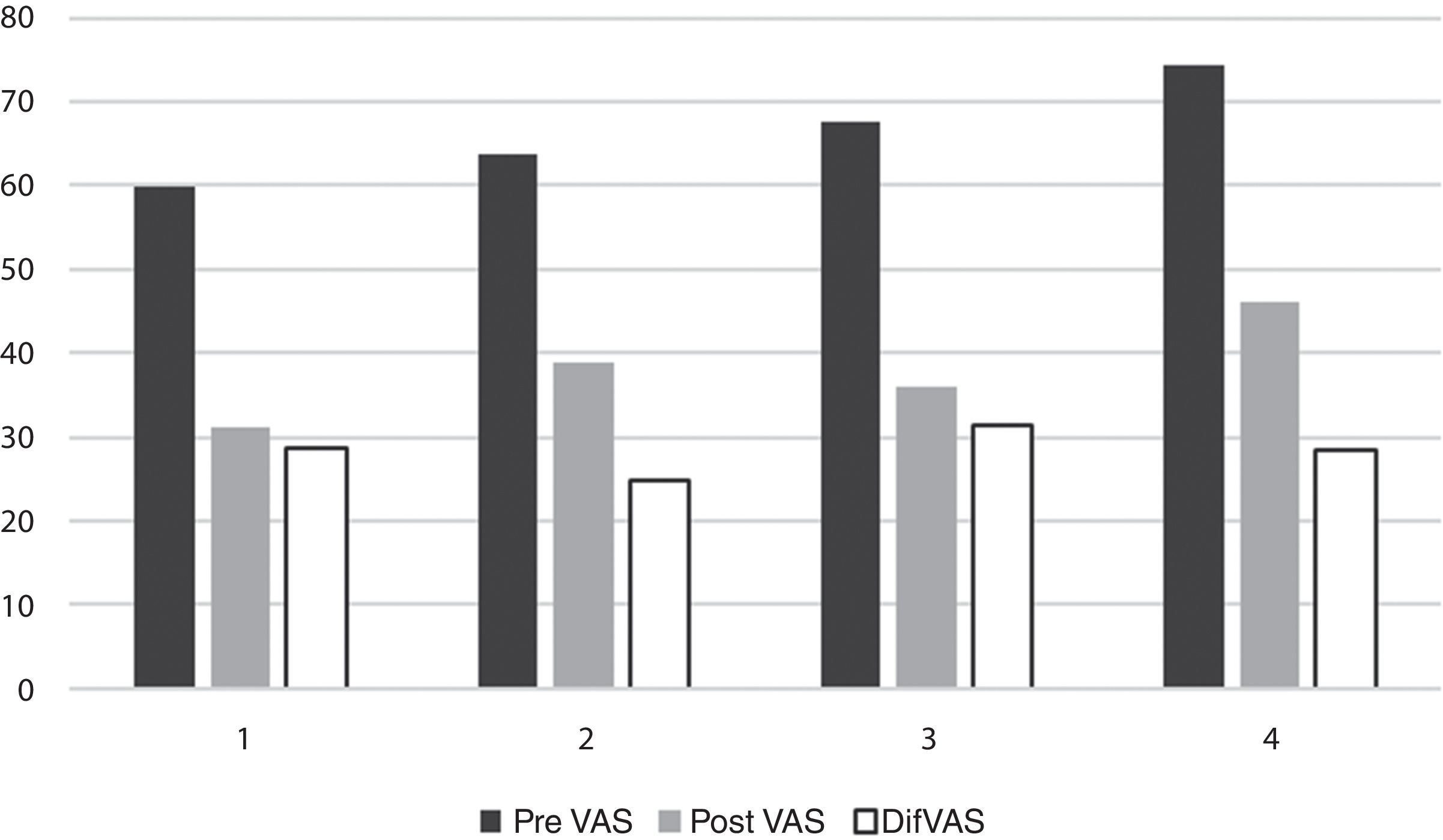
When the mean improvement was stratified according to the Ahlbäck scale, it was found that the mean improvement was similar across all grades, with no significant differences: 28.75 points in grade 1; 24.75 in grade 2; 31.39 in grade 3, and 28.33 in grade 4 (p=.41). No significant differences were found between pre- and post-treatment VAS scores for each Ahlbäck grade (Fig. 2).
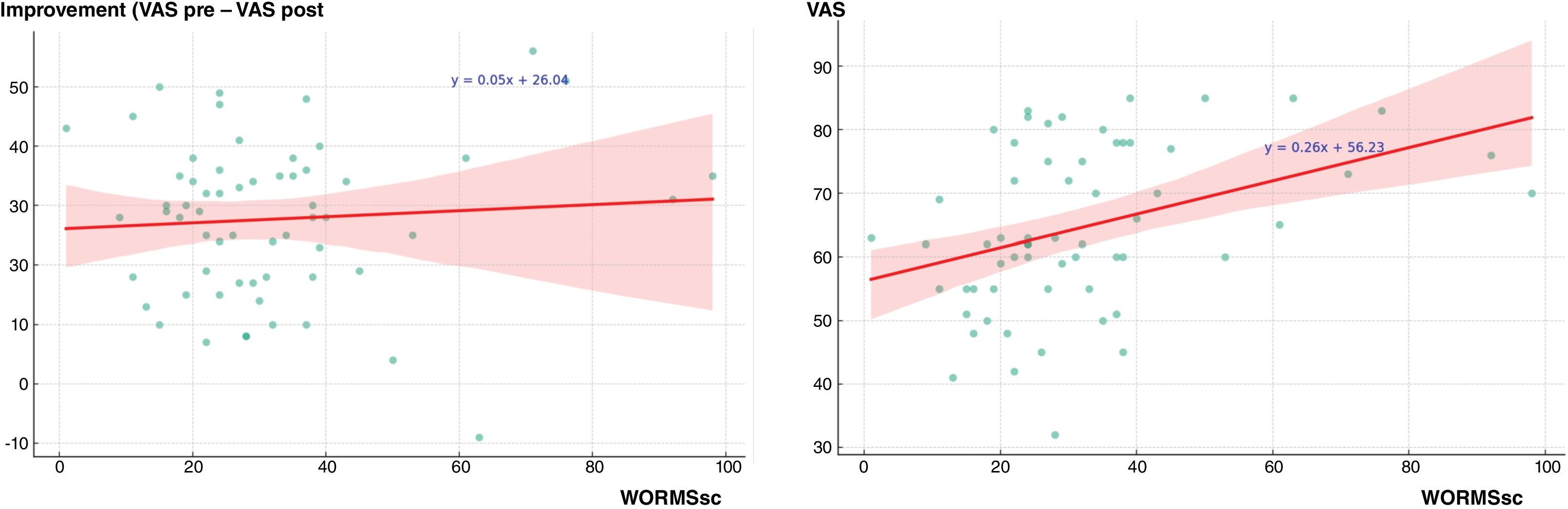
Spearman's correlation test was performed to determine whether there was a correlation between clinical parameters and the WORMSsc. No correlation was found between DifVAS and the WORMSsc score (r=.02; p=.81). However, a statistically significant moderate correlation was found between pre-treatment VAS and the WORMSsc, suggesting that patients with more pain might have greater subchondral bone involvement on MRI. The r-value was .43 with p<.005 (Fig. 3).
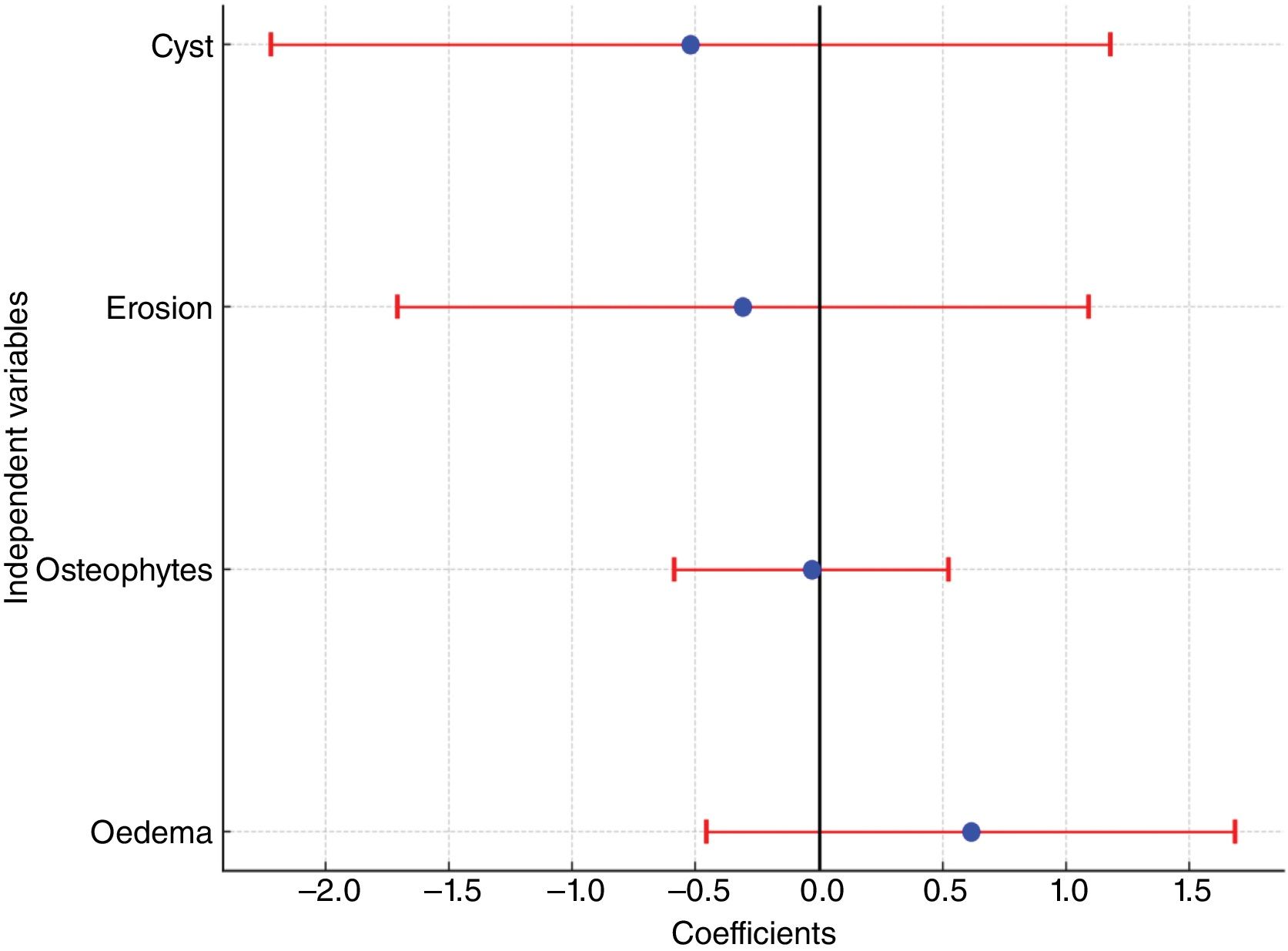
In the multivariate model, the R2 value was −.024. The coefficients for each of the scale items were oedema: .61 (−.46 to 1.79); erosion −.31 (−1.71 to 1.09); cyst −.52 (−2.22 to 1.18), and osteophytes −.03 (−.59 to .52) (Fig. 4). No statistically significant differences were found.
Of the 61 patients, 7 (11.5%) required further invasive treatments for pain control after treatment with PRP, 4 underwent ultrasound-guided genicular nerve block, 2 patients underwent arthroscopy, and one patient was scheduled for total knee replacement.
DiscussionIn the present study carried out on a sample of patients with knee osteoarthritis treated with intra-articular infiltrations of PRP, an overall improvement in pain was observed without this improvement being related to the radiological grade of the disease or to the degree of subchondral bone involvement on MRI.
Knee osteoarthritis is no longer considered a disease of mechanical stress on the joint, but rather a multifactorial biological process, with several not fully understood triggers that lead to cartilage degeneration.11 PRP used as an intra-articular treatment appears to have a clinical effect in improving pain and function in patients, but its role at the biological level is not fully understood. Cole et al.12 demonstrated in a clinical trial comparing PRP with intra-articular hyaluronic acid that PRP promoted the downregulation of some of the proteins involved in the intra-articular inflammatory process.
However, if we consider the knee as an organ whose various components may be involved in the osteoarthritic process, we must also consider the involvement of components of the knee other than the joint cavity itself. The subchondral bone, because of its anatomical relationship with the articular cartilage and because of the biological processes that appear to be established between it and the cartilage, may be a potential player in the degenerative process, and has therefore been considered a potential therapeutic target.10 Sanchez et al., in a clinical study on 19 patients, used a combined approach injecting intra-articular and intra-osseous PRP into the subchondral bone of the femur and tibia, and obtained a significant improvement in the patients at 6 months.13
The hypothesis of our study was that greater subchondral bone involvement as measured by the WORMS scale would be associated with less pain relief in patients with knee osteoarthritis treated with intra-articular PRP. As the WORMS scale takes into account many aspects of knee osteoarthritis, to simplify the interpretation of the MRI scans we decided to focus the analysis on the sections of the classification that describe subchondral bone involvement.
We found a significant correlation of some significance between the pre-treatment pain scale and our WORMSsc score, suggesting that greater subchondral bone involvement may be directly related to greater pain. However, greater subchondral bone involvement in patients does not appear to influence clinical outcome 12 weeks after PRP injection, with no correlation between the degree of improvement in patients and the WORMSsc score on MRI. Similarly, none of the variables that make up the WORMSsc questionnaire items had a significant influence on pain improvement, according to the results of the multivariate analysis. There was also no correlation between patient improvement and Ahlbäck classification. A study by Burchard et al.14 also found no correlation between the degree of osteoarthritis of the knee as measured by the WORMS scale—although they considered it in its entirety—and the improvement obtained after the administration of intra-articular PRP, concluding that the efficacy of intra-articular PRP was not associated with the degree of involvement on MRI.
The study also shows a greater clinical improvement at 3 months compared to patients treated with betamethasone. This suggests that PRP may have a longer lasting effect on patients than corticosteroids. It is possible that there is no significant difference in treatment with either infiltration in the short term, but that the effect of corticosteroids tends to wear off over the weeks. This effect has been shown in other conditions such as plantar fasciitis. A meta-analysis by Hohmann et al. in plantar fasciitis found that, although corticosteroids and PRP had similar short-term effects, PRP achieved greater pain control than corticosteroids at 3 months and the result can extend to 12 months.15
A weakness of the present study is the lack of long-term follow-up, as it is a retrospective study with a 3-month follow-up. Although some patients are followed up in the longer term, the treatment protocol at our hospital provides for a fixed review 12 weeks after completion of the injections, so using this cut-off point in the clinical review allowed us to obtain a larger and more homogeneous sample. However, many patients with good outcomes are referred for follow-up by primary care beyond this period, resulting in loss to follow-up over a longer period. Therefore, the effect of intra-articular PRP beyond 12 weeks cannot be determined on the basis of this study, and the lack of correlation between pain and subchondral bone damage at 3 months does not mean it cannot play a role in long-term osteoarthritis. Boffa et al.5 found in a sample of 200 patients with osteoarthritis of the knee treated with PRP that, while patients with subchondral bone marrow lesions did not appear to have worse short- to medium-term clinical outcomes than those without, those with a higher bone marrow oedema grade were more likely to require further infiltration or surgery within one year. Similarly, Van Genechten et al.8 found that, in patients undergoing treatment with intra-articular MFAT cell concentrate for knee osteoarthritis, those with bone marrow lesions or oedema were more prone to treatment failure at one year, with efficacy dropping to 45% at 12 months. Another study by Sanchez et al. comparing the administration of intraosseous and intra-articular PRP with the administration of intra-articular PRP alone found that, although there were no short-term differences, after 6 months of treatment, patients treated with intra-osseous infiltrations of PRP had better clinical outcomes and required fewer subsequent treatments, although he does not mention which ones.16 In our case, 11% of patients required some subsequent treatment, although in series such as that of Sanchez et al.,16 the rate of patients who may need further treatment after intra-articular PRP alone was as high as 21%. Although our study cannot draw conclusions beyond 3 months, it appears that the anti-inflammatory effect of intra-articular PRP leads to short-term improvement. However, the evidence in the literature allows us to hypothesise that the subchondral bone may be an influential factor in maintaining this improvement in the long term. It would be interesting to carry out a prospective analysis of our patients in the long term to try to confirm or refute this fact.
ConclusionsPatients with knee osteoarthritis treated with 3 intra-articular PRP injections experienced a significant clinical improvement in pain 12 weeks after treatment. However, there is no correlation between subchondral bone involvement as measured by MRI, or its different lesional manifestations, and patients’ improvement in pain. A higher degree of subchondral bone involvement on MRI is associated with the presence of more pain on the VAS scale before treatment. Long-term studies comparing intra-articular PRP with intra-articular and intra-osseous PRP administration are needed to better define the role of subchondral bone in the pathogenesis of osteoarthritis.
Level of evidenceLevel of evidence iii.
Ethical considerationsThe author declares that the ethical protocols of the institution were followed. Consent was obtained from all patients to participate in the study, and patients were anonymised during data collection and processing to protect their privacy.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interestThe author has no conflict of interest to declare.




![Modified WORMS assessment scale using only the aspects related to the subchondral bone (WORMSsc). Aspects related to the left side (bone erosion, bone oedema, presence of cysts, and appearance of osteophytes) are measured according to the drawings for each item, scoring each in the following areas of the knee: condyles (subdivided into anterior [A], central [C], and posterior [P] area), plateaus (subdivided into anterior [A], central [C], and posterior [P]), patellofemoral (medial [M] and lateral [L]), and tibial spines (S). The maximum possible scores are listed in the table below right. EFT: external femorotibial; IFT: internal femorotibial; PF: patellofemoral; Sp: spines. Modified WORMS assessment scale using only the aspects related to the subchondral bone (WORMSsc). Aspects related to the left side (bone erosion, bone oedema, presence of cysts, and appearance of osteophytes) are measured according to the drawings for each item, scoring each in the following areas of the knee: condyles (subdivided into anterior [A], central [C], and posterior [P] area), plateaus (subdivided into anterior [A], central [C], and posterior [P]), patellofemoral (medial [M] and lateral [L]), and tibial spines (S). The maximum possible scores are listed in the table below right. EFT: external femorotibial; IFT: internal femorotibial; PF: patellofemoral; Sp: spines.](https://static.elsevier.es/multimedia/18884415/0000006900000002/v1_202503050803/S1888441524002054/v1_202503050803/en/main.assets/thumbnail/gr1.jpeg?xkr=ue/ImdikoIMrsJoerZ+w96p5LBcBpyJTqfwgorxm+Ow=)




