Total hip arthroplasty (THA) in patients with residual poliomyelitis (RP) is a surgical challenge. Dysplastic morphology, osteoporosis and gluteal weakness hinder orientation, increase fracture risk and reduce implant stability. The aim of this study is to describe a series of patients with RP treated by THA.
Material and methodsRetrospective descriptive study of patients with RP treated with THA between 1999 and 2021 in a tertiary hospital, with clinical and radiological follow-up and functional and complication evaluation until present or death, with a minimum of 12 months.
ResultsSixteen patients underwent surgery, with 13 THA implanted in the paretic limb, 6 for fracture and 7 for osteoarthritis, while the remaining 3 were implanted in the contralateral limb. Four dual mobility cups were implanted as an antiluxation measure. At 1 year postoperatively, 11 had complete range of motion with no increase in Trendelenburg cases. The Harris hip score (HHS) improved 32.1 points, the visual analogue scale (VAS) 5.25 points, and the Merlé-d’Augbiné-Poste scale 6 points. The length discrepancy correction was 13.77mm. Median follow-up was 3.5 years (1–24). Two cases were revised for polyethylene wear and two for instability, with no infections, periprosthetic fractures, or cup or stem loosening.
ConclusionsTHA in patients with RP allows improvement of the clinico-functional situation with an acceptable complication rate. The risk of dislocation could be minimised with dual mobility cups.
La prótesis total de cadera (PTC) en pacientes con secuelas de poliomielitis (SP) supone un reto quirúrgico. La morfología displásica, la osteoporosis y la debilidad glútea dificultan la orientación, incrementan el riesgo de fractura y reducen la estabilidad del implante. El objetivo de este estudio es describir una serie de pacientes con SP tratados mediante PTC.
Material y métodosEstudio descriptivo retrospectivo de pacientes con SP intervenidos mediante PTC entre 1999 y 2021 en un hospital de tercer nivel, con seguimiento clínico y radiológico, y evaluación funcional y de las complicaciones hasta el presente o hasta el fallecimiento, con un mínimo de 12 meses.
ResultadosSe intervinieron 16 pacientes, implantándose 13 PTC en el miembro parético, 6 por fractura y 7 por coxartrosis, mientras que las otras 3 PTC se implantaron en el miembro contralateral. Se implantaron 4 cotilos de doble movilidad como medida antiluxante. Al año postoperatorio, 11 presentaban un balance articular completo sin aumentar los casos de Trendelenburg. El Harris Hip Score (HHS) mejoró 32,1 puntos, la escala visual analógica (EVA), 5,25 puntos, y la escala de Merle d’Augbiné-Postel, 6 puntos. La corrección de la discrepancia de longitud fue de 13,77mm. La mediana del seguimiento fue de 3,5 años (1-24). Dos casos se revisaron por usura del polietileno y 2 por inestabilidad, sin registrarse infecciones, fracturas periprotésicas o aflojamiento del cotilo o vástago.
ConclusionesLa PTC en pacientes con SP permite mejorar la situación clínico-funcional con una tasa de complicaciones aceptable. El riesgo de luxación podría minimizarse con cotilos de doble movilidad.
Poliomyelitis is a human infection caused by poliovirus, a single-stranded RNA enterovirus transmitted via the orofecal route.1 It can be acquired at any age, but its main effects occur in children under the age of 3 years (in over 50% of cases).2 While infected individuals are most often asymptomatic, in 1% of cases the virus is able to invade the central nervous system and selectively destroy motor neurons in the spinal cord, resulting clinically in musculoskeletal flaccid paralysis. Neuromuscular paralysis, over time, leads to muscle contractures, bone deformities and joint stiffness, as well as decreased growth of the paretic limb and osteoporosis.3,4
In Spain, as in the rest of the world, polio affected children mainly in the 1950s. The introduction of the vaccination campaign in 1964 led to a marked decrease in morbidity (.19 per 100,000 inhabitants) and mortality (.13 per 100,000 inhabitants). Since 1988, no further cases have been reported in Spain.5 Although it has now been eradicated in our environment, patients with residual poliomyelitis (RP), who suffered from polio decades ago, are still being treated.
Arthritic hip pathology in patients with RP is complex and poses a surgical challenge for orthopaedic surgeons, since in addition to advanced age, there are other factors such as bone fragility in the paretic limb, the dysplastic morphology of these hips, overuse of the contralateral limb, gluteal weakness and the increase in falls due to musculoskeletal and balance alterations in these patients.6 For this reason, and because of the current low prevalence of this pathology, there are few orthopaedic surgeons with experience in this type of patient.7
It is possible that due to its low prevalence, there are currently not many scientific publications in the literature on the treatment of coxarthrosis in these patients using total hip replacements (THA).8–13 However, analysis is relevant due to its particular characteristics and possible associated complications. The aim of the present study is to describe a series of patients with RP treated with THA, to describe the key aspects of surgical treatment to minimise possible complications, and to show the results and complications in relation to the total number of patients with THA and RP published to date, thus facilitating the management of new cases.
Material and methodsA retrospective descriptive study of patients with RP following infection in childhood, operated on by implantation of a THA, in the paretic or contralateral limb, in a tertiary hospital between 1999 and 2021, was performed. Patients with clinical and radiological follow-up up to the present or until death were included. Patients with incomplete clinical or radiological follow-up were excluded, as well as cases with follow-up of less than 12 months.
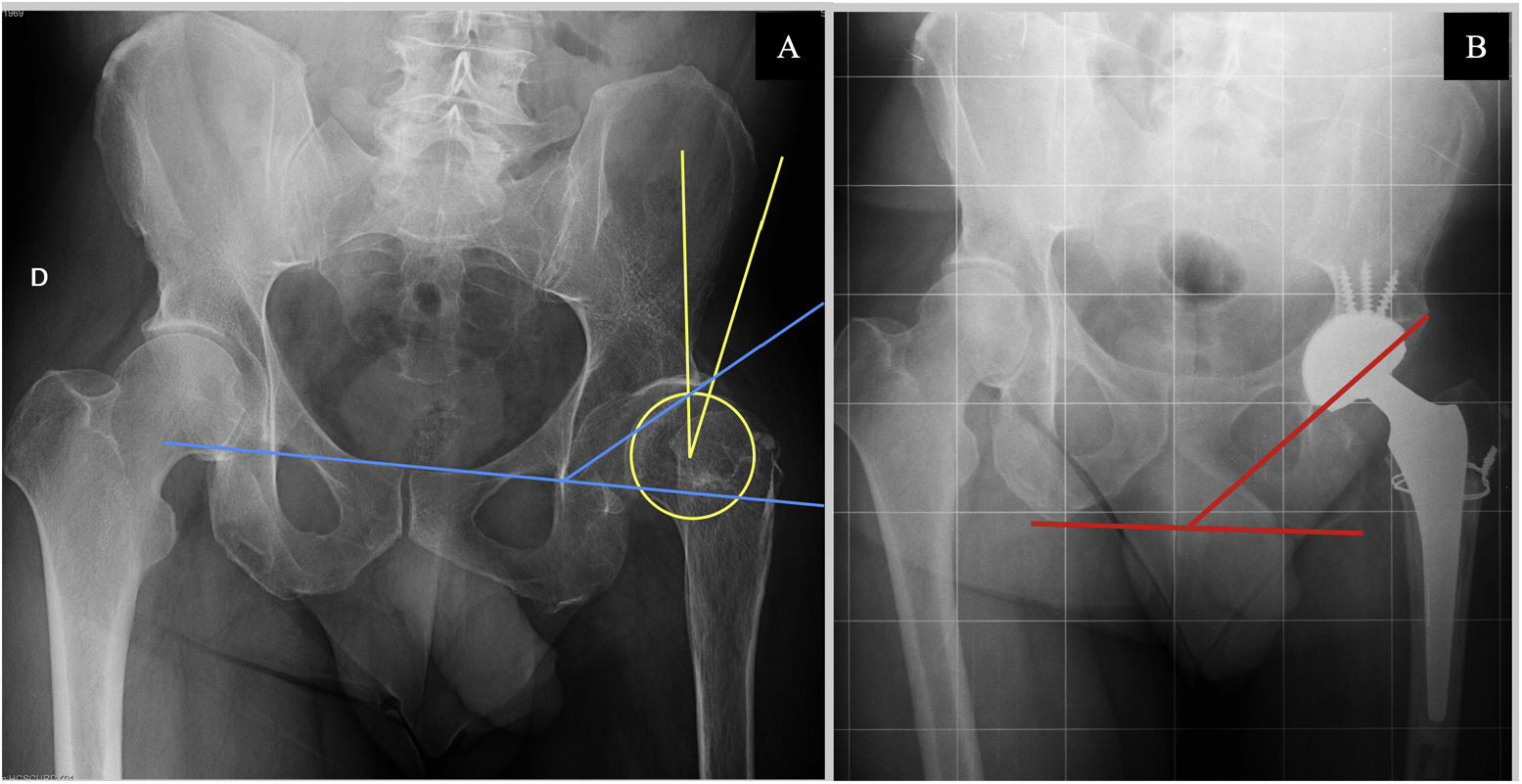
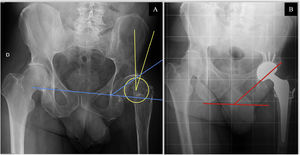
Various demographic variables such as age, sex, weight, body mass index (BMI), and clinical data such as paretic side, type of poliomyelitis involvement (musculoskeletal and visceral), hip joint balance, previous poliomyelitis surgeries, and previous hip surgeries were collected from the medical records. Data were also collected on the patient's preoperative functionality: the type of gait, the need for technical aids prior to surgery and the Harris hip score (HHS), the Merlé-d’Augbiné-Poste scale and the visual analogue scale (VAS). The following preoperative radiological parameters were measured on anteroposterior radiographs of the pelvis: Sharp's angle or acetabular tilt and Wiberg centre-edge angle (Fig. 1), radiological coxarthrosis grade according to the Tönnis classification, radiological characterisation of the degree of hip dysplasia using the Crowe and Hartofilakidis classifications. Lower limb length discrepancy (LLLD) was measured on preoperative telemetry in patients who did not undergo surgery due to a proximal femur fracture.
Radiological measurements. (A) Preoperative anteroposterior X-ray of the patient 9's pelvis. Wiberg angle measurement (yellow): angle between the vertical with the centre of rotation of the femoral head and the superolateral edge of the acetabulum. Sharp's acetabular angle measurement (blue): intersection of a horizontal line through the inferior edge of the acetabulum (“radiological tear-drop”) and an oblique line extending from this inferior edge to the superolateral edge of the acetabular cavity. (B) Post-operative anteroposterior radiograph of the patient 9's pelvis. Measurement of the acetabular inclination angle (red): angle between a line joining the ischial spines and the oblique line tangent to the superior and inferior edge of the acetabular component.
Intraoperative variables studied included American Society of Anesthesiology (ASA) score; type of anaesthesia; mean intraoperative time; patient position; type of surgical approach and associated surgical gestures and type of implants used. In the immediate postoperative period, the mean hospitalisation time, the need for transfusion in the first 24h, immediate complications and days to the start of weight loading were recorded.
Postoperative clinical and radiological follow-up was carried out for at least 12 months, recording at one year the characteristics of functionality and the degree of satisfaction and recovery of the patients. Clinical data (pain), functional data (need for technical aids, hip joint balance, type of gait, EVA scales, HHS, Merlé-d’Augbiné-Poste scale) and degree of patient satisfaction at 12 months were collected from the clinical records. The latter variable was measured on a 4-point scale: 1 indicated excellent satisfaction (no pain, full mobility and activity), 2 indicated good (occasional pain, full mobility and activity), 3 indicated fair (discomfort after prolonged activity) and 4 poor (pain and activity limitation).
Finally, a postoperative radiological re-evaluation was performed on anteroposterior radiographs of the pelvis and telemetry, by two independent observers who did not participate in these interventions, at 1, 6 and 12 months post-surgery, measuring: the discrepancy in limb length (LLD), the degree of cup inclination (cup abduction of 40°±10° was considered satisfactory) according to Lewinnek's safety zone. The occurrence of clinical complications and, radiologically, the presence of signs of loosening of the cup and stem according to the De Lee and Gruen classifications were also studied throughout the follow-up of the patients.
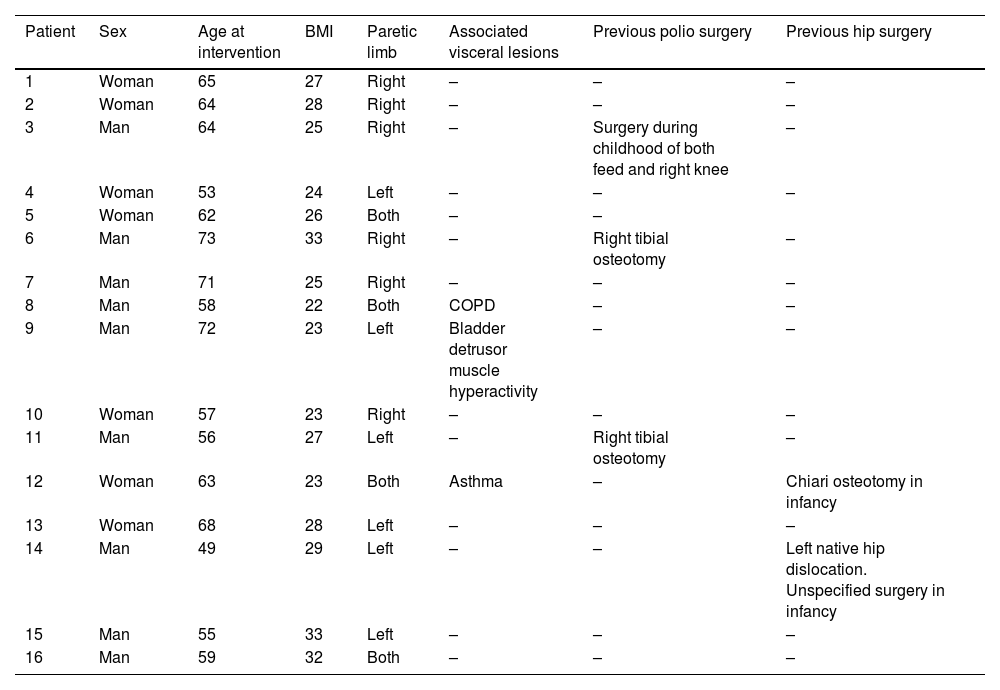
ResultsSixteen patients (9 males and 7 females) were operated on, with a mean age of 61.81 years. Twelve of them had unilateral lower limb paralysis and 4 had bilateral lower limb paralysis. Only 3 patients had visceral RP lesions associated with musculoskeletal lesions. Three of the patients had undergone lower limb interventions in childhood as a result of poliomyelitis, mainly osteotomies, arthrodesis and tendon transposition. In 2 of them the interventions involved the THA candidate hip, one treated by Chiari osteotomy and one case unspecified. The rest of the demographic findings are listed in Table 1.
Demographic data and comorbidities of the patient due to poliomyelitis.
| Patient | Sex | Age at intervention | BMI | Paretic limb | Associated visceral lesions | Previous polio surgery | Previous hip surgery |
|---|---|---|---|---|---|---|---|
| 1 | Woman | 65 | 27 | Right | – | – | – |
| 2 | Woman | 64 | 28 | Right | – | – | – |
| 3 | Man | 64 | 25 | Right | – | Surgery during childhood of both feed and right knee | – |
| 4 | Woman | 53 | 24 | Left | – | – | – |
| 5 | Woman | 62 | 26 | Both | – | – | |
| 6 | Man | 73 | 33 | Right | – | Right tibial osteotomy | – |
| 7 | Man | 71 | 25 | Right | – | – | – |
| 8 | Man | 58 | 22 | Both | COPD | – | – |
| 9 | Man | 72 | 23 | Left | Bladder detrusor muscle hyperactivity | – | – |
| 10 | Woman | 57 | 23 | Right | – | – | – |
| 11 | Man | 56 | 27 | Left | – | Right tibial osteotomy | – |
| 12 | Woman | 63 | 23 | Both | Asthma | – | Chiari osteotomy in infancy |
| 13 | Woman | 68 | 28 | Left | – | – | – |
| 14 | Man | 49 | 29 | Left | – | – | Left native hip dislocation. Unspecified surgery in infancy |
| 15 | Man | 55 | 33 | Left | – | – | – |
| 16 | Man | 59 | 32 | Both | – | – | – |
BMI: body mass index; COPD: chronic obstructive pulmonary disease.
Radiologically, 12 of the cases had moderate or advanced signs of coxarthrosis (Tönnis 2–3) in the hip to be operated on. There were 4 cases of hip dysplasia according to the Crowe classification (2 cases Crowe type 2 and 2 cases Crowe type 3) and Hartofilakidis (4 cases of dysplasia type B). The mean Wiberg centre-edge angle was 34.91°. Finally, limb length discrepancy could be assessed in 9 cases by preoperative telemetry, with a mean discrepancy of −23.4mm.
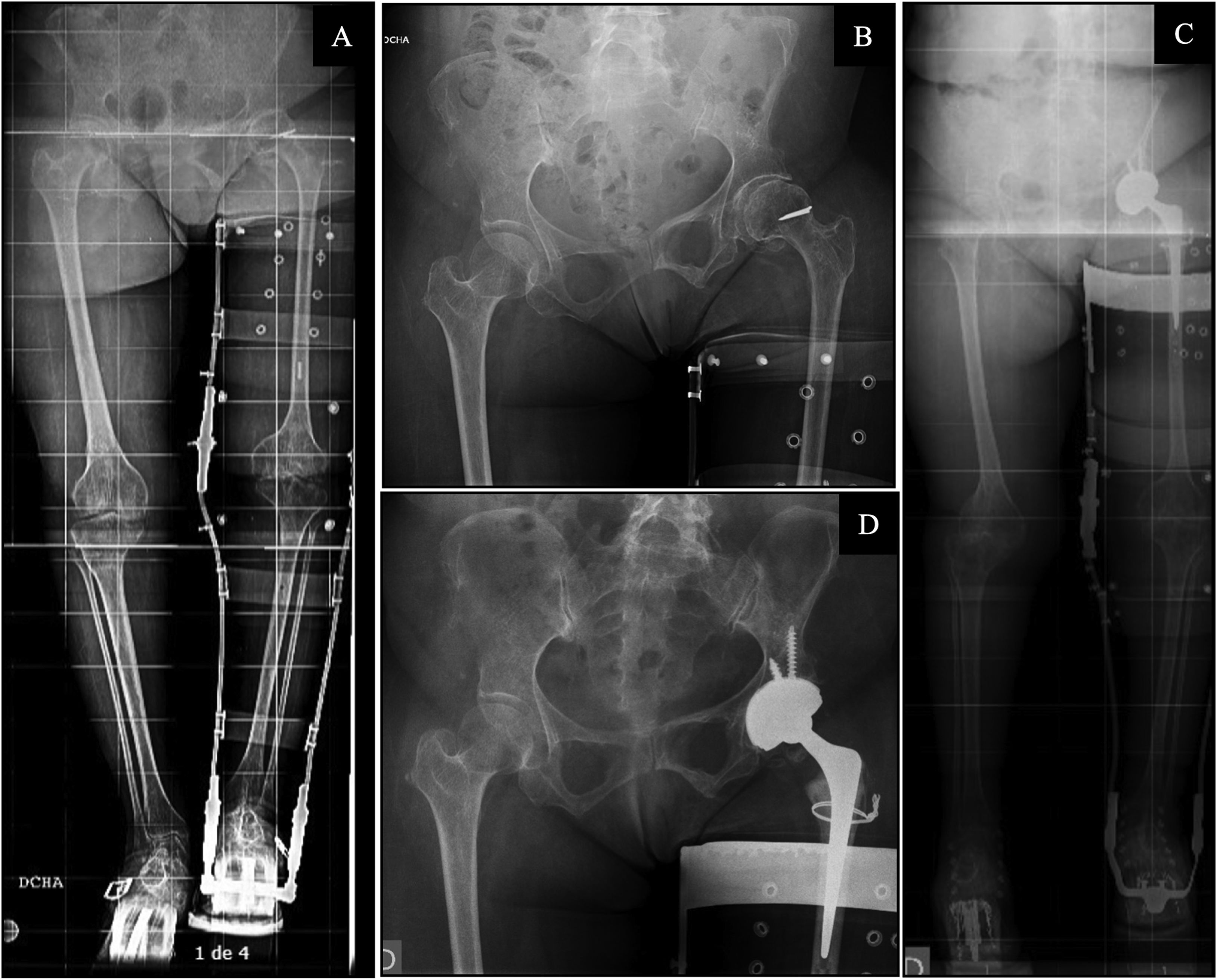
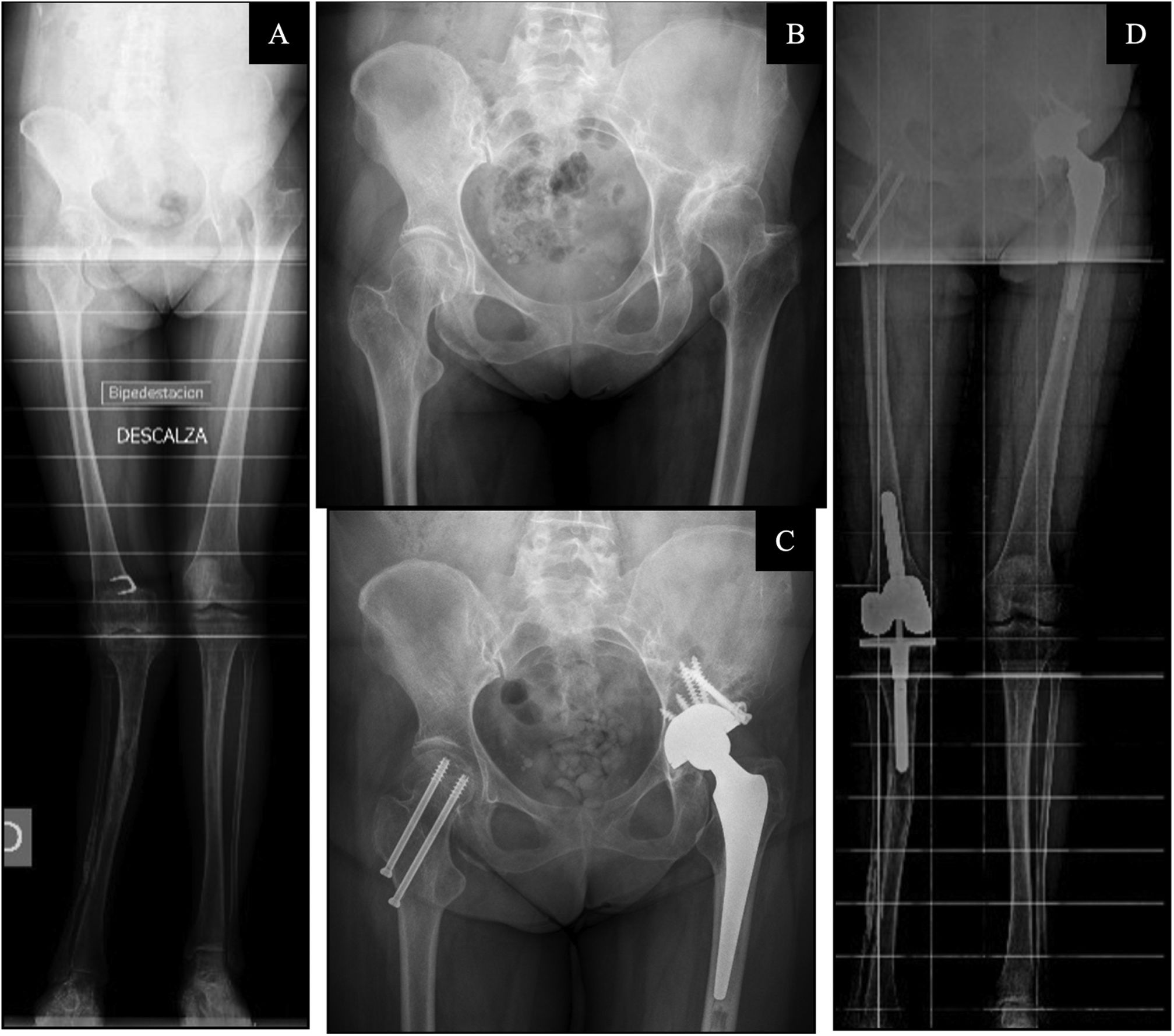
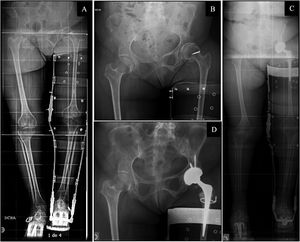
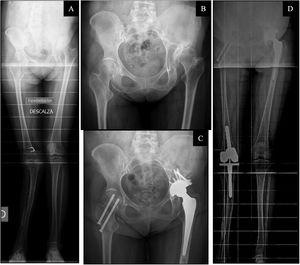
Of the 16 cases operated, 13 prostheses were implanted in the paretic limb, 6 of the cases for subcapital fracture and the other 7 cases for early coxarthrosis, while the other 3 THA were implanted in the contralateral limb, one case for subcapital fracture and 2 for early coxarthrosis. All operated patients had an ASA II score, locoregional anaesthesia was used in 14 of the 16 cases, 2 of them requiring general anaesthesia. The patient position was lateral decubitus in 13 cases and supine in 3 cases, all of them using a direct lateral Hardinge approach. The mean intraoperative time was 114min. As associated surgical procedures, a prophylactic femoral cerclage was performed in 4 patients due to an intraoperative perception of poor bone quality (Fig. 2) and an acetabular cancellous allograft was used in 2 cases (Fig. 3). In 4 cases, the most recently operated cases, a double mobility cup was implanted. Other features related to the operation are listed in Table 2.
(A) Preoperative telemetry of lower limbs in patient with inguinal support brace and lift. (B) Preoperative anteroposterior X-ray of the pelvis. (C) Post-operative lower limb telemetry in patient with inguinal support brace and lift. (D) Postoperative anteroposterior radiography of the pelvis. A 68-year-old woman with sequelae of poliomyelitis in the left lower limb. She presented with Tonnis type II left hip coxarthrosis in Crowe type I and Hartofilakidis type A hip dysplasia. A preoperative Wiberg angle of 29.5° and a LLD of −3.1cm was measured on preoperative telemetry. She underwent left total hip arthroplasty with a Tritanium Stryker® double mobility cup, Exeter stem and Stryker® metal head with cerclage over the greater trochanter with wire. Postoperatively she had a LLD of .73cm and a cup inclination of 38.6°.
(A) Preoperative telemetry of the lower limbs. (B) Preoperative anteroposterior X-ray of the pelvis. (C) Post-operative lower limb telemetry. (D) Post-operative anteroposterior pelvis X-ray. A 63-year-old woman with sequelae of poliomyelitis in both lower limbs, operated on in childhood for Chiari type osteotomy in the left hip. She presented with Tonnis type III coxarthrosis of the left hip in Crowe type II and Hartofilakidis type A hip dysplasia. A preoperative Wiberg angle of 30.7° and a LLD of −4.7cm was measured on preoperative telemetry. She underwent Continuum Zimmer® left total hip arthroplasty, Furlong JRI® cemented stem and ceramic-alumina head and cup reconstruction with screw-retained femoral head autograft. Postoperatively, the patient had a LLD of 2.2 and a cup inclination of 35.2°. On the contralateral side she had an arthritic genu valgum treated with a semi-constrained knee prosthesis and a hip fracture treated with cannulated screws.
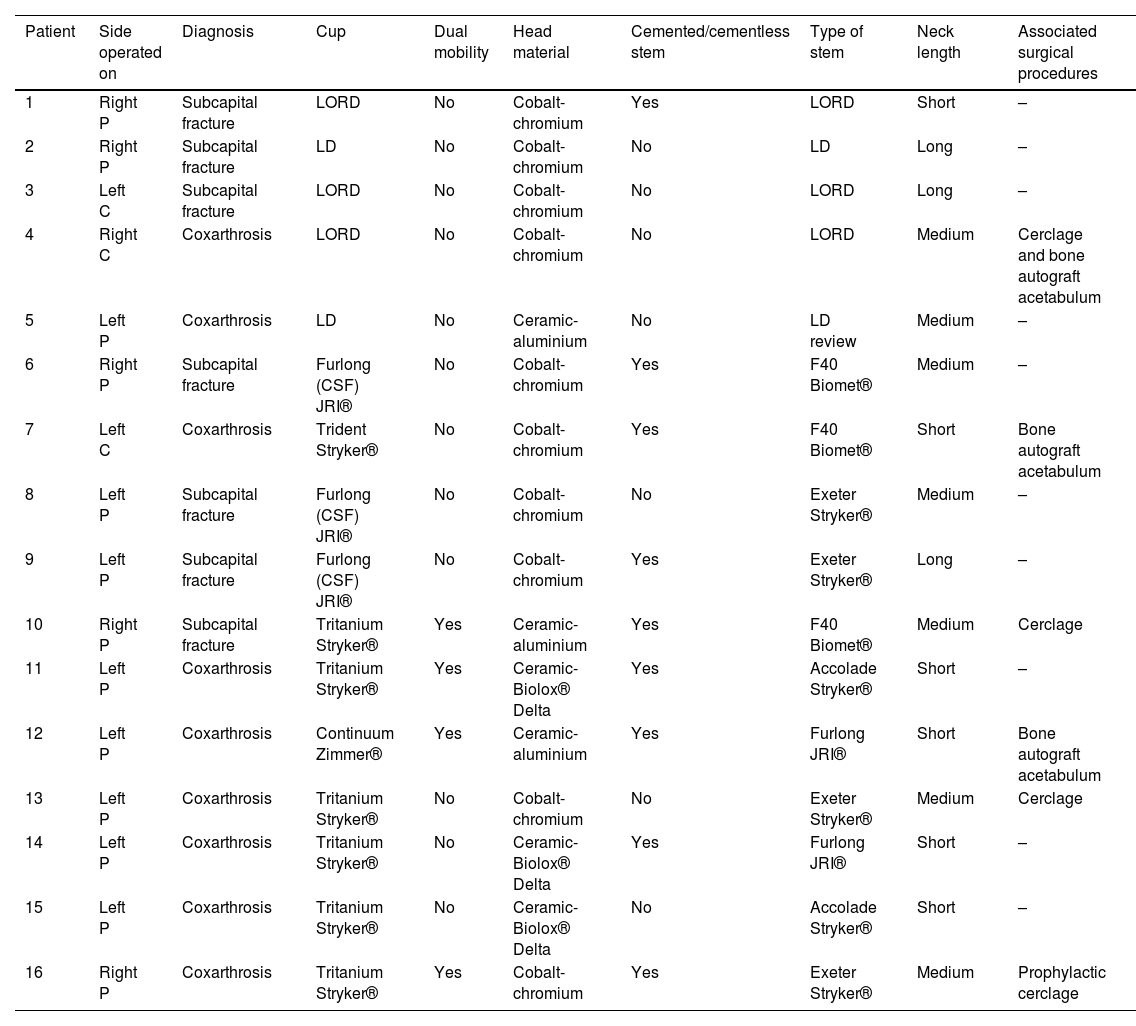
Side operated on, diagnosis and type of arthroplasty.
| Patient | Side operated on | Diagnosis | Cup | Dual mobility | Head material | Cemented/cementless stem | Type of stem | Neck length | Associated surgical procedures |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Right P | Subcapital fracture | LORD | No | Cobalt-chromium | Yes | LORD | Short | – |
| 2 | Right P | Subcapital fracture | LD | No | Cobalt-chromium | No | LD | Long | – |
| 3 | Left C | Subcapital fracture | LORD | No | Cobalt-chromium | No | LORD | Long | – |
| 4 | Right C | Coxarthrosis | LORD | No | Cobalt-chromium | No | LORD | Medium | Cerclage and bone autograft acetabulum |
| 5 | Left P | Coxarthrosis | LD | No | Ceramic-aluminium | No | LD review | Medium | – |
| 6 | Right P | Subcapital fracture | Furlong (CSF) JRI® | No | Cobalt-chromium | Yes | F40 Biomet® | Medium | – |
| 7 | Left C | Coxarthrosis | Trident Stryker® | No | Cobalt-chromium | Yes | F40 Biomet® | Short | Bone autograft acetabulum |
| 8 | Left P | Subcapital fracture | Furlong (CSF) JRI® | No | Cobalt-chromium | No | Exeter Stryker® | Medium | – |
| 9 | Left P | Subcapital fracture | Furlong (CSF) JRI® | No | Cobalt-chromium | Yes | Exeter Stryker® | Long | – |
| 10 | Right P | Subcapital fracture | Tritanium Stryker® | Yes | Ceramic-aluminium | Yes | F40 Biomet® | Medium | Cerclage |
| 11 | Left P | Coxarthrosis | Tritanium Stryker® | Yes | Ceramic-Biolox® Delta | Yes | Accolade Stryker® | Short | – |
| 12 | Left P | Coxarthrosis | Continuum Zimmer® | Yes | Ceramic-aluminium | Yes | Furlong JRI® | Short | Bone autograft acetabulum |
| 13 | Left P | Coxarthrosis | Tritanium Stryker® | No | Cobalt-chromium | No | Exeter Stryker® | Medium | Cerclage |
| 14 | Left P | Coxarthrosis | Tritanium Stryker® | No | Ceramic-Biolox® Delta | Yes | Furlong JRI® | Short | – |
| 15 | Left P | Coxarthrosis | Tritanium Stryker® | No | Ceramic-Biolox® Delta | No | Accolade Stryker® | Short | – |
| 16 | Right P | Coxarthrosis | Tritanium Stryker® | Yes | Cobalt-chromium | Yes | Exeter Stryker® | Medium | Prophylactic cerclage |
C: contralateral; P: paretic.
The mean length of hospital stay was 10.27 days, all patients had good postoperative pain control, and during admission only one case of superficial infection of the surgical wound was recorded as a complication. This was resolved with intravenous antibiotherapy. Nine of the patients required transfusion of two red blood cell concentrates in the immediate postoperative period (in the first 24h) with good recovery. Most patients (13 out of 16) started ambulation with two technical aids in the first 48h postoperatively with the collaboration of the available physiotherapist team. All patients were ambulating with crutches or a walker before hospital discharge.
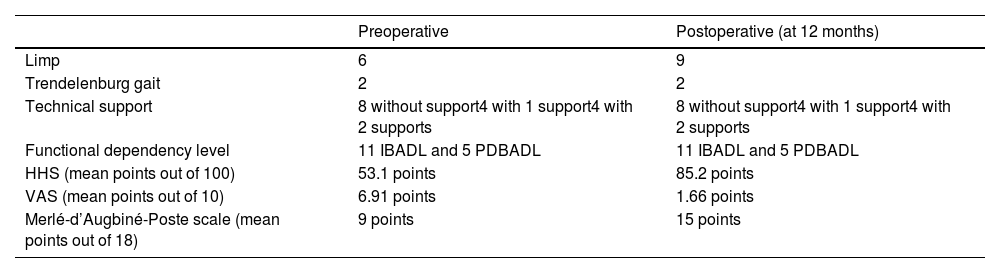
Follow-up data at 12 months are shown in Tables 3 and 4. Eleven patients were found to have required outpatient rehabilitation and all had the same need for technical aids as preoperatively. Cases of Trendelenburg gait were the same as preoperatively (2 cases), and 2 patients used a walking aid both preoperatively and postoperatively. The HHS improved by a mean of 32.1 points, the VAS score improved by a mean of 5.25 points and the Merlé-d’Augbiné-Poste scale improved by a mean of 6 points.
Pre and postoperative clinical and functional aspects.
| Preoperative | Postoperative (at 12 months) | |
|---|---|---|
| Limp | 6 | 9 |
| Trendelenburg gait | 2 | 2 |
| Technical support | 8 without support4 with 1 support4 with 2 supports | 8 without support4 with 1 support4 with 2 supports |
| Functional dependency level | 11 IBADL and 5 PDBADL | 11 IBADL and 5 PDBADL |
| HHS (mean points out of 100) | 53.1 points | 85.2 points |
| VAS (mean points out of 10) | 6.91 points | 1.66 points |
| Merlé-d’Augbiné-Poste scale (mean points out of 18) | 9 points | 15 points |
VAS: visual analogue scale; HHS: Harris hip score; IBADL: independent for basic activities of daily living; PDBADL: partially dependent for basic activities of daily living.
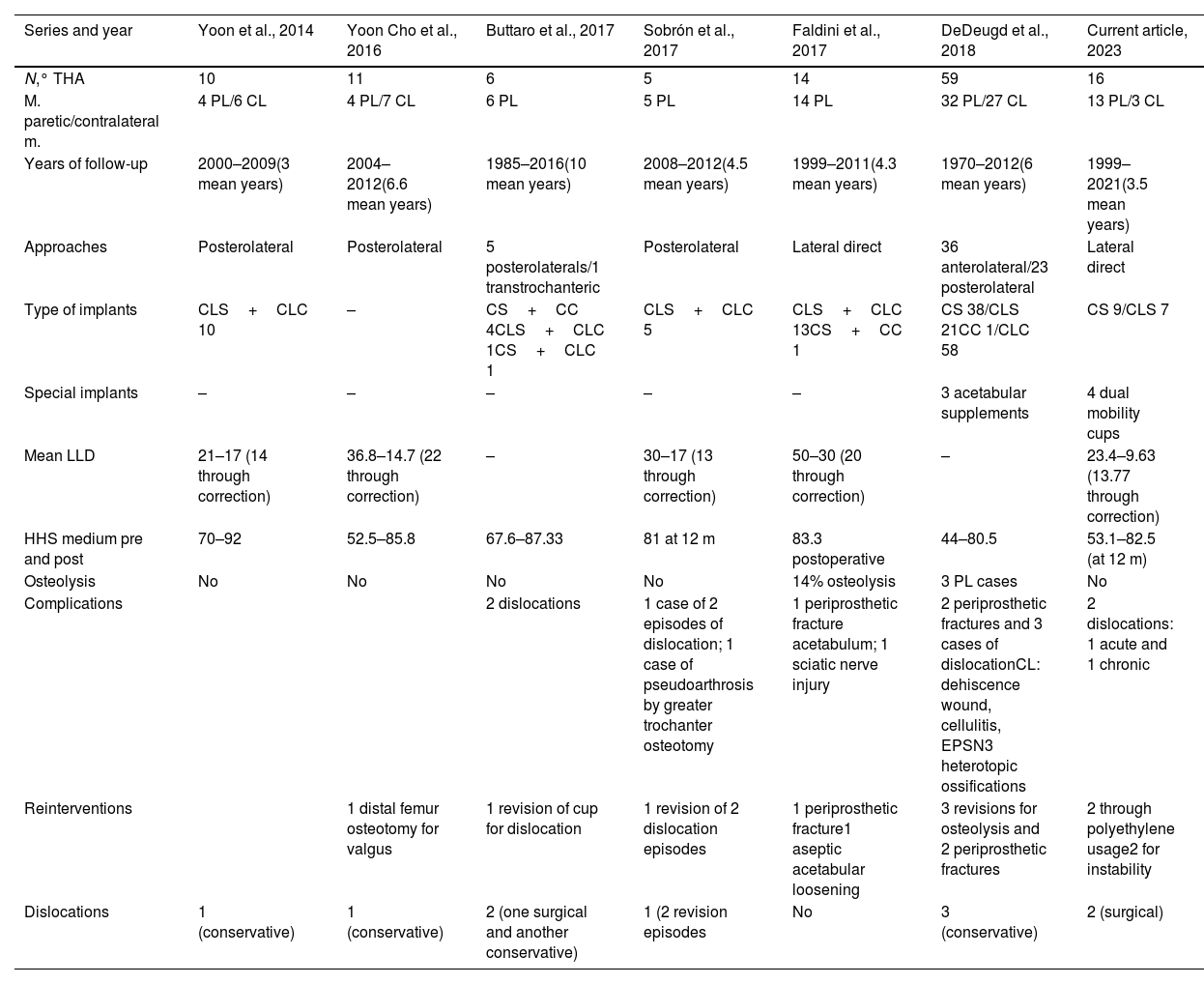
Discussion of the most recent series in the literature.8–13
| Series and year | Yoon et al., 2014 | Yoon Cho et al., 2016 | Buttaro et al., 2017 | Sobrón et al., 2017 | Faldini et al., 2017 | DeDeugd et al., 2018 | Current article, 2023 |
|---|---|---|---|---|---|---|---|
| N,° THA | 10 | 11 | 6 | 5 | 14 | 59 | 16 |
| M. paretic/contralateral m. | 4 PL/6 CL | 4 PL/7 CL | 6 PL | 5 PL | 14 PL | 32 PL/27 CL | 13 PL/3 CL |
| Years of follow-up | 2000–2009(3 mean years) | 2004–2012(6.6 mean years) | 1985–2016(10 mean years) | 2008–2012(4.5 mean years) | 1999–2011(4.3 mean years) | 1970–2012(6 mean years) | 1999–2021(3.5 mean years) |
| Approaches | Posterolateral | Posterolateral | 5 posterolaterals/1 transtrochanteric | Posterolateral | Lateral direct | 36 anterolateral/23 posterolateral | Lateral direct |
| Type of implants | CLS+CLC 10 | – | CS+CC 4CLS+CLC 1CS+CLC 1 | CLS+CLC 5 | CLS+CLC 13CS+CC 1 | CS 38/CLS 21CC 1/CLC 58 | CS 9/CLS 7 |
| Special implants | – | – | – | – | – | 3 acetabular supplements | 4 dual mobility cups |
| Mean LLD | 21–17 (14 through correction) | 36.8–14.7 (22 through correction) | – | 30–17 (13 through correction) | 50–30 (20 through correction) | – | 23.4–9.63 (13.77 through correction) |
| HHS medium pre and post | 70–92 | 52.5–85.8 | 67.6–87.33 | 81 at 12 m | 83.3 postoperative | 44–80.5 | 53.1–82.5 (at 12 m) |
| Osteolysis | No | No | No | No | 14% osteolysis | 3 PL cases | No |
| Complications | 2 dislocations | 1 case of 2 episodes of dislocation; 1 case of pseudoarthrosis by greater trochanter osteotomy | 1 periprosthetic fracture acetabulum; 1 sciatic nerve injury | 2 periprosthetic fractures and 3 cases of dislocationCL: dehiscence wound, cellulitis, EPSN3 heterotopic ossifications | 2 dislocations: 1 acute and 1 chronic | ||
| Reinterventions | 1 distal femur osteotomy for valgus | 1 revision of cup for dislocation | 1 revision of 2 dislocation episodes | 1 periprosthetic fracture1 aseptic acetabular loosening | 3 revisions for osteolysis and 2 periprosthetic fractures | 2 through polyethylene usage2 for instability | |
| Dislocations | 1 (conservative) | 1 (conservative) | 2 (one surgical and another conservative) | 1 (2 revision episodes | No | 3 (conservative) | 2 (surgical) |
CC: cemented cup; CL: contralateral limb; CLC: cementless cup; CLS: cementless stem; CS: cemented stem; HHS: Harris hip score; LLD: limb length discrepancy; PL: paretic limb; THA: total hip arthroplasty.
Finally, postoperative radiological assessment showed a LLD of -9.63mm, compared to the preoperative mean of −23.4mm. The mean radiographic abduction was 4.5° (30°–59.4°), with 15 of the 16 cases falling within the safe orientation range according to Lewinnek.
The median follow-up time was 3.5 years (1–24 years). There were 4 THA revision surgeries in 3 patients in the series: one case of cup revision at 9 days for acute instability of the prosthesis, one case of revision for polyethylene wear at 17 years and a last case of revision for polyethylene wear at 14 years, which 10 years later required further revision for chronic instability. No infections or periprosthetic fractures were recorded in this series. There were no signs of loosening or osteolysis at the cup or stem on radiographic examinations or other complications throughout the follow-up in this series.
DiscussionThis study provides a series of 16 patients with RP treated by THA with good functional results and an acceptable rate of complications, given the small number of patients with RP and THA published to date.
There are few patient series with RP and THA, the series with the largest number of cases being those published in the last decade,8–13 while the remaining publications have only 1–2 cases. Cases have also been reported that have been included in larger series that included patients with different neurological diseases intervened with THA,14–17 without specifying polio patients. There are only two case series with higher numbers: that of DeDeugd et al.,8 with 59 cases in both paretic and contralateral limbs, and that of Faldini et al.,11 with 14 cases, but all in the paretic limb. The common features of this study with those found in other articles in the literature are summarised in Table 4.
Six of the patients in our series had had previous interventions due to poliomyelitis, coinciding with other case series described in the literature.9–12 The mean follow-up of the series studied was 3.5 years, lower than that of the most current series,8–13 where follow-up is 6 or even 10 years on average; however, the range of years of follow-up in our sample includes follow-ups of up to 24 years. Radiologically, the intervened hips presented similar characteristics to those of case series reported in the literature, highlighting a higher frequency of hips with a more advanced degree of dysplasia (more frequently Crowe type III) in Faldini et al.11 and Buttaro et al.9 The mean lower limb LLD correction in our series is 13.77mm, coinciding with the cases presented in the literature. In most series, patients were operated on using the posterolateral approach, which has a higher rate of dislocations if capsular repair is not performed, compared to the Hardinge direct lateral approach, which, in turn, increases the incidence of Trendelenburg gait,18 which was used in all cases in our series. This approach was also used in the complete series of Faldini et al.11 and in 36 of the 59 patients of DeDeugd et al.,8 at the surgeon's discretion.
Regarding cementing or non-cementing of components, there is no consensus in the literature, nor is there a similar pattern in the case series. In many cases the reasons for cementing or not cementing the components are based on the surgeon's choice and the criterion at that time. It should be noted that in our series, 4 dual-mobility cups were implanted in the last cases operated and at the surgeon's discretion, in accordance with the current concept that THA with dual-mobility cups have a lower incidence of dislocations both in the first year19 and at 5–6 years of follow-up,20,21 with dislocation rates of between .2% and 5%. We have not found in the literature any series of patients with poliomyelitis operated with dual mobility cups, although there is one case series, that of Hernigou et al.,17 included in a larger study of patients with different neurological diseases, in which 7 of the 12 patients with poliomyelitis were implanted with constrained cups, without studying the differences between the groups that were implanted and those that were not.
In terms of functional outcomes, the improvement in HHS is consistent with the data reported in most series in the literature. In the largest series, that of DeDeugd et al.,8 the mean improvement in HHS in the paretic limb group was differentiated from that in the contralateral limb group, with no significant differences in this respect. We have not found any series using the Merlé-d’Augbiné-Poste functionality scale, which was studied in this series. In relation to pain, this was statified by means of VAS, but with variable results, with most patients reporting no pain or a VAS score of less than 2, coinciding with the results of this study.
Finally, with regard to complications, in most series no signs of osteolysis or loosening of the implants have been described during follow-up, with the exception of two series with a number of cases similar to ours and higher, probably due to the greater number of cases and longer follow-up periods: that of DeDeugd et al.,8 and that of Faldini et al.,11 with an incidence of 5% and 14%, respectively. It is likely that if the mean follow-up of our cases were longer, we would identify periacetabular or perivascular osteolysis, as occurs in THA in patients without poliomyelitis. However, patients with RP have lower functional demand than healthy patients, which may contribute to lower loosening rates. Other complications identified in the literature, although not in our series, are hererotopic ossifications, as reported in DeDeugd et al.,8 with incidences similar to the general population and without establishing poliomyelitis as a risk factor. Three cases of periprosthetic fractures have been reported in the literature (2 femoral and 1 acetabular),8,11 all of them in the paretic limb, which required revision surgery and with satisfactory evolution, with no cases observed in our series. However, although no fracture episodes have been reported in this series, patients should be informed of these risks. Prosthetic dislocation occurs more frequently than in THA in healthy patients due to dysplastic morphology and gluteal weakness, among other aspects. In our series, one case of acute and one chronic dislocation was reported, the former due to malorientation of the cup, which was revised, and the latter due to chronic weakness of the soft tissues, which ruled out infection and was also revised, and a double mobility cup was implanted. In the largest series, that of DeDeugd et al.,8 three episodes of dislocation were described in 3 of the THAs implanted in paretic limbs, all of which were treated conservatively. In the series of Buttaro et al.9 of 6 patients, 2 episodes of dislocation were recorded in 2 of the patients: one of them in relation to an excessively verticalised cup, which was revised, and the other in a stable hip with good component orientation, which was treated conservatively. In the series by Sobrón et al.,10 2 episodes of dislocation were recorded in one patient, requiring revision of the prosthesis, with insufficient femoral anteversion of the stem. This was one of the main causes associated with the risk of dislocation in posterolateral approaches, along with loss of the posterior capsule.22,23 Finally, two episodes of dislocation in the series of Yoon Cho et al.12 and Yoon et al.13 were treated conservatively, using a spica for 2 months. All episodes of dislocation found in the literature occurred in the first few weeks after surgery, consistent with the overall incidence data reported in the literature.24
The limitations of this study are firstly its retrospective nature and the small sample size due to the currently low prevalence of this pathology. Obtaining data from non-digitised medical records and complementary tests has contributed to the reduction of patients, due to incomplete medical records or inability to locate complementary tests.
In conclusion, according to our series, primary THA in patients with RP improves functional status and reduces pain. The musculoskeletal alterations present in these patients make it a complex procedure, but the complication rate seems acceptable. We believe that the risk of dislocation could be minimised with dual mobility cups, such as those used in the last patients in our series, but more studies with larger samples are needed to corroborate this in this type of population.
Level of evidenceLevel of evidence I.
FundingThe authors or their immediate family members, and any research foundation with which they are affiliated, did not receive any financial payment or other benefits from any commercial entity related to the subject of this article.
Conflict of interestsThe authors have no conflict of interests to declare.