Hip arthroplasty instability is one of the most worrisome complications and one of the main indications for revision surgery. We present a retrospective study evaluating the results of revision hip replacement surgery performed for instability.
Material and methodsObservational, retrospective study from 1/12/2010 to 1/12/2022. Fifty-nine medical records of patients operated for hip dislocation were reviewed. Epidemiological variables and data such as type of dislocation based on Wera classification, cup position based on Lewinnek, type of implants, associated surgical techniques and the results in terms of recurrence of dislocation or reoperation were recorded.
ResultsFifty-nine patients: 33 women, 26 men, mean age 77.0 years. Mean follow-up 3.2 years (range 1.6–13.1). Based on Wera: had a single cause 37 cases, 2 causes 19 and 3 causes or more, 3 cases. In 61% of the cases in the series, malposition of the cup played an essential role in the dislocation (type I Wera). In the series, the Lewinnek zone could not be evaluated in 7 cases. For the remaining patients, 30% were within the Lewinnek zone. Only one patient in the series had a history of lumbar instrumentation. Implant used: double mobility (DM) in 17 cases (28.8%) and a constrained system in 38 cases (64.4%). Heads with adaptive cone were used in 2 cases (3%). In 4 cases (6%) a modified Whiteside type plasty was associated. Girdlestone was indicated in 2 cases (3%). Recurrence of dislocation 1 occasion: 18 cases (31%); 2 or more occasions: 7 cases (12%). Reoperation 15 cases (25%) range (1–5), main reasons: instability, infection or peri-prosthetic fractures. Probability of success defined as no recurrence: at one year is 80.5%, and at two years is 70.6%, showing no differences between constrained or dual-mobility implant.
Comments and conclusionsHip prosthesis dislocation is multifactorial in origin, although in most cases in the series the key factor was malposition of the acetabulum. Constrained and DM implants showed similar effectiveness. The results of this study emphasize the need for techniques that allow adequate positioning and orientation of the acetabular component to prevent, in a high percentage of cases, the need for this type of revision surgery.
La inestabilidad de la artroplastia de cadera es una de las complicaciones más preocupantes y una de las principales indicaciones de la cirugía de revisión. Presentamos un estudio retrospectivo que evalúa los resultados de la cirugía de revisión de prótesis de cadera efectuada por motivo de inestabilidad.
Material y métodosEstudio observacional, retrospectivo del periodo de 1/12/2010 a 1/12/2022. Se revisaron 59 historias clínicas de pacientes operados por luxación de cadera. Se registraron las variables epidemiológicas, y los datos como el tipo de luxación en función de la clasificación de Wera, la posición del cotilo en base a Lewinnek, el tipo de implantes, las técnicas quirúrgicas asociadas y los resultados en cuanto a la recidiva de luxación o re-operación.
ResultadosCincuenta y nueve pacientes: 33 mujeres y 26 varones, con edad promedio de 77,0 años. Seguimiento medio de 3,2 años (rango: 1,6-13,1). En función de Wera: tenían una única causa 37 casos, 2 causas 19 y 3 causas o más, 3 casos. En el 61% de los casos de la serie, la malposición del cotilo jugó un papel esencial en la luxación (tipo I Wera). En la serie, en 7 casos no se pudo evaluar la zona de Lewinnek. Para el resto de los pacientes, el 30% estaban dentro de la zona de Lewinnek. Solo un paciente de la serie tenía como antecedente una instrumentación lumbar. Implante utilizado: doble movilidad (DM) en 17 casos (28,8%) y un sistema constreñido en 38 casos (64,4%). Se usaron cabezas con cono adaptativo en 2 casos (3%). En 4 casos (6%) se asoció una plastia tipo Whiteside modificada. En 2 casos (3%) se indicó Girdlestone. Recidiva de luxación una ocasión: 18 casos (31%); 2 ocasiones o más 7 casos (12%). Re-operación 15 casos (25%) rango de (1-5), principales motivos: inestabilidad, infección o facturas periprotésicas. Probabilidad de éxito definido como no tener recidiva: al año es del 80,5%, y a los 2 años es del 70,6%, sin mostrar diferencias entre implante constreñido o de DM.
Comentarios y conclusionesLa luxación de prótesis de cadera tiene un origen multifactoriales, aunque en la mayoría de los casos de la serie el factor clave fue la malposición del acetábulo. Los implantes constreñidos y de DM mostraron efectividad similar. Los resultados de este estudio enfatizan la necesidad de técnicas que permitan un adecuado posicionamiento y orientación del componente acetabular para prevenir, en un elevado porcentaje de casos, la necesidad de este tipo de cirugías de revisión.
The surgical procedures for hip joint replacements have a high success rate, and a satisfaction rate of 93%. To achieve optimal outcomes, it is essential to restore the centre of rotation, place the components in the optimal position and orientation, restore the acetabular and femoral offset, and ensure adequate soft tissue tension to recreate the natural biomechanics of the hip. Instability of total hip arthroplasty (THA) is a significant problem that can severely affect patients’ quality of life and also the longevity of the implant, and may require revision surgery.1
The causes of instability are multifactorial and include factors attributable to the patient, the surgical technique, and especially those related to the implant.1,2 As the number of hip joint replacements continues to increase, preventing dislocations is crucial.3 In the case of unstable hip replacements requiring treatment, determining the success rate and the most appropriate procedure remains controversial.
This study aims to evaluate the outcomes of hip replacement revision surgery due to instability, determine the cause according to the Wera classification, and examine the outcomes based on implant type, either DM or constrained, as treatment options.
Materials and methodsThe study was approved by the Hospital Institution's Ethics Committee for data management, which was collected by our department. We present an observational, descriptive, and retrospective study.
Clinical data were collected from each patient's electronic medical records. Clinical variables included age; sex; laterality; body mass index (BMI); associated comorbidities; smoking; obesity; lumbar spine fusion and the year of primary prosthesis replacement; number of previous dislocations; number of re-dislocations, and reoperations. Comorbidity was assessed using the American Society of Anaesthesiology (ASA) scale.
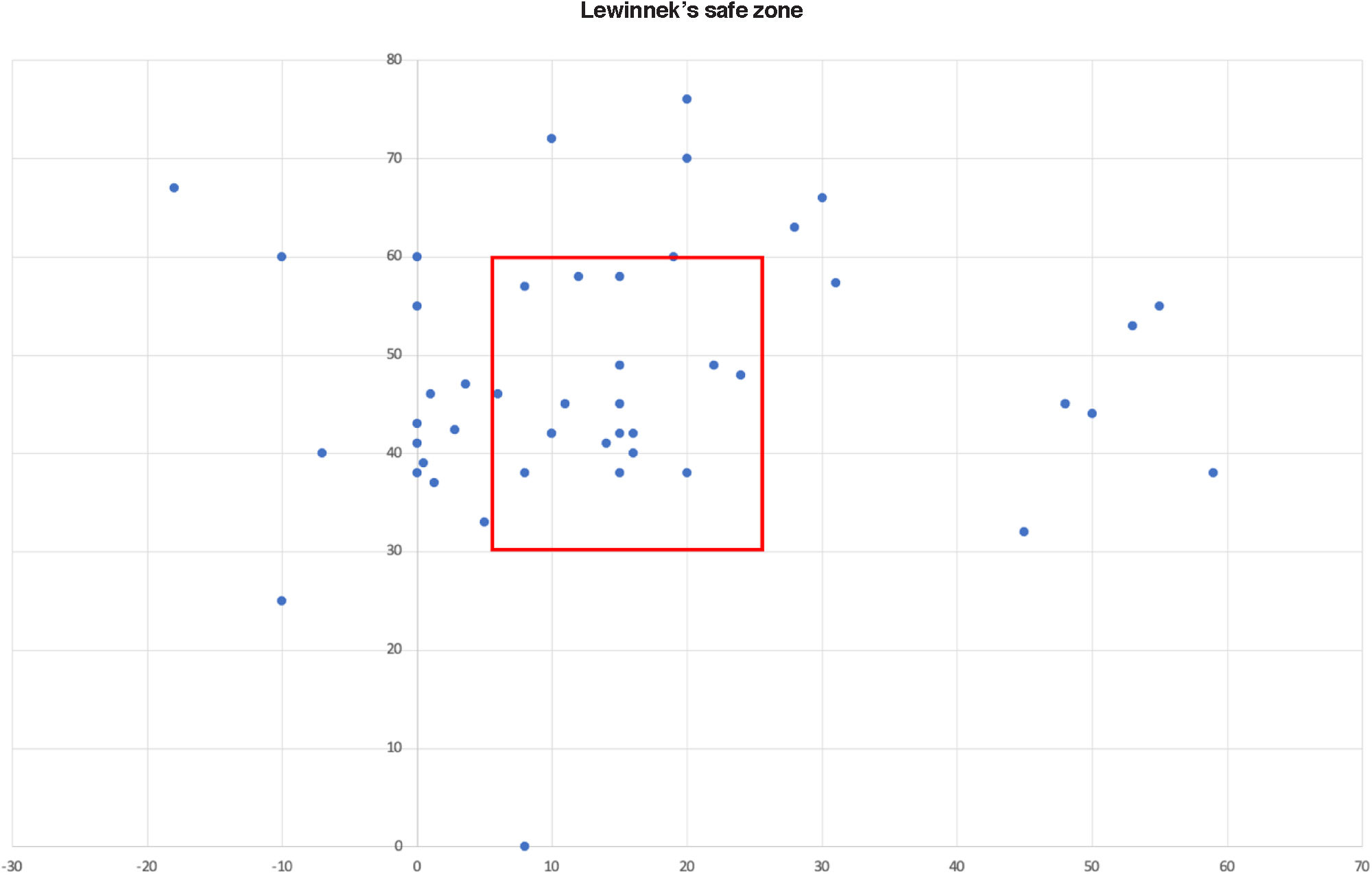
Radiographic evaluation included anteroposterior (AP) projection of the pelvis in a standing position with 15° internal rotation and axial projection of the affected hip. The affected hip was evaluated using three-dimensional (3D) computed tomography (CT) in all cases where this test had been performed, and the acetabular component version and inclination values were measured; considering the area described by Lewinnek et al.: anteversion of 10±5° and acetabular inclination of 35±10°.4,5
Study populationCriteria and selectionAll medical records of patients who underwent hip prosthesis replacement due to hip prosthesis dislocation were reviewed from December 1, 2010, to December 1, 2022. Fifty-nine cases were identified, including those who underwent surgery for hip prosthesis dislocation or any other type of prosthetic instability.
Data collectionEpidemiological variables and data on the type of dislocation based on the Wera classification; cup position based on the Lewinnek criteria; implant use; technique employed; recurrence of dislocation or reoperation for any reason, and history of lumbar instrumentation were recorded.
Statistical analysisA descriptive analysis was performed, providing absolute and relative frequency distributions for qualitative variables, and position and dispersion measures for quantitative variables. Differences between qualitative variables were subsequently evaluated using Pearson's or Fisher's chi-square test, depending on whether the hypothesis regarding expected frequencies was met or not. Differences in the number of dislocations between groups were assessed using the Wilcoxon test in the event of non-normality.
The significance level used was .05.
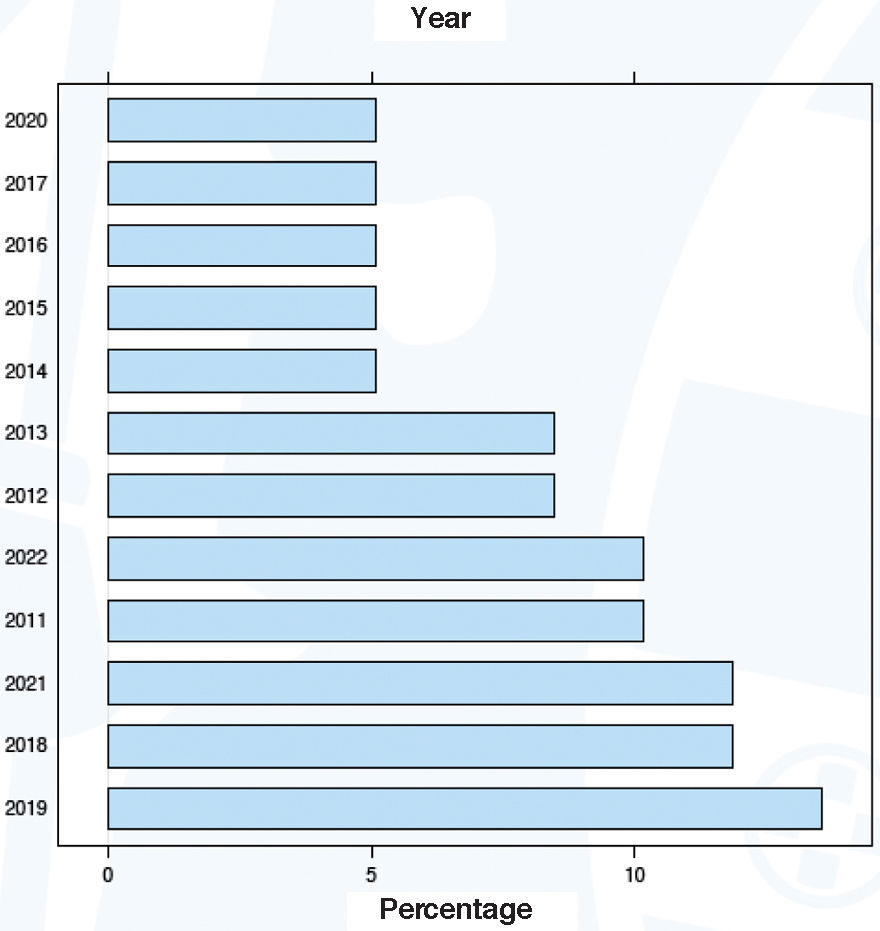
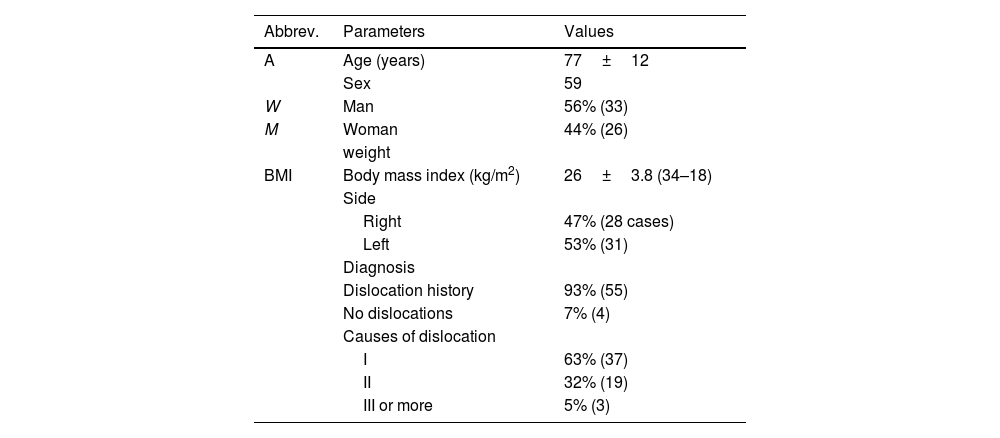
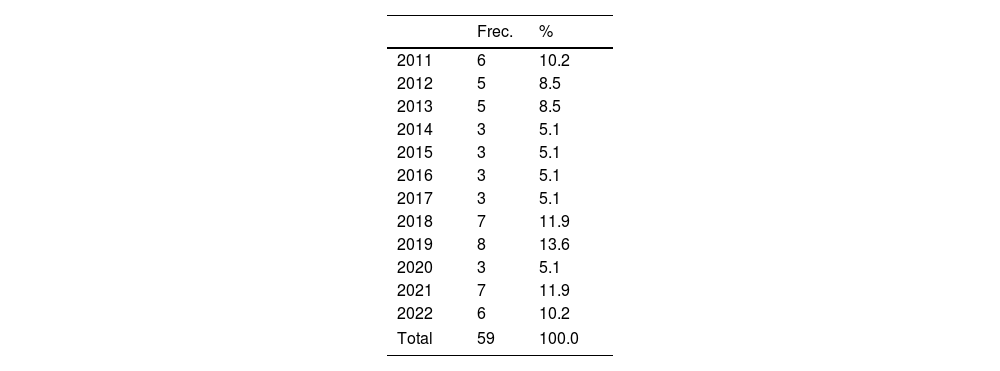
ResultsPopulation characteristicsA total of 59 patients (33 women and 26 men) were included, with a mean age of 77 years. Demographic data are summarised in Table 1. The mean follow-up was 46 months (range: 1.6–13.8). The number of cases registered per year is detailed in Table 2, and their percentage distribution is shown in Fig. 1. A stable trend in the number of indications in our healthcare area was observed.
Demographic characteristics expressed in number, percentage (%) and median (range).
| Abbrev. | Parameters | Values |
|---|---|---|
| A | Age (years) | 77±12 |
| Sex | 59 | |
| W | Man | 56% (33) |
| M | Woman | 44% (26) |
| weight | ||
| BMI | Body mass index (kg/m2) | 26±3.8 (34–18) |
| Side | ||
| Right | 47% (28 cases) | |
| Left | 53% (31) | |
| Diagnosis | ||
| Dislocation history | 93% (55) | |
| No dislocations | 7% (4) | |
| Causes of dislocation | ||
| I | 63% (37) | |
| II | 32% (19) | |
| III or more | 5% (3) |
Values expressed in averages, with ranges in brackets.
According to Wera, it was shown that 37 patients (63%) had a single cause, 19 patients (32%) had two causes, and 3 patients (5%) had three or more causes of instability.
The diagnosis of abductor deficiency was guided preoperatively by radiological studies and CT scans in cases where CT was performed, but ultrasound or MRI were not performed in any case. The definitive diagnosis of abductor deficiency was made based on intraoperative findings.
Cup position and radiographic analysisIn 61% of cases, cup malpositioning was the primary cause of dislocation (Wera type I). Of the 59 cases, cup position could not be assessed in 7 cases due to the lack of complete either radiographic or CT studies. In the remaining 30% of patients, the cup position was within the safe zone defined by Lewinnek (Fig. 2).
The cup had an average verticality of 48° and an anteversion of 11°, with a combined anteversion of 59°. Acetabular verticality was also observed at a maximum of 76° and a minimum of 0°. Femoral anteversion averaged 11°, with a maximum of 38° and a minimum of −18°.
Based on the Wera classification, we obtained type I in 36 cases (61%), type II in 12 cases (20%), type III in 19 cases (32%), type IV in 0 cases (0%), type V in 7 cases (12%), and type VI in 10 cases (17%).
Use of implants and surgical approachThere were 59 patients available, with 4 missed cases (6.8%). The dual-mobility (DM) implant was used in 17 patients (28.8%), while the constrained system was used in 38 cases (64.4%). Additionally, adaptive cone heads were used in 2 patients (3%), and a modified Whiteside implant was used in 4 patients (6%). The Girdlestone procedure was used in 2 cases (3%).
The most commonly used surgical approach was the lateral approach in 41 patients (69%), followed by the posterolateral approach in 7 patients (12%), and the posterior approach in 7 patients (12%). In 4 cases (7%), we did not obtain information on the type of approach used in the revision surgery.
In 28 cases in the series, the cup replacement was partial, by cementing it into the interior of the previous cup. The remaining cup replacements were complete.
The constrained implants were the Socinser (cemented) constrained cup in 16 cases; the Stryker Trident® (cemented) constrained All-Poly 0° cup in 11 cases; the Stryker Trident® 10° (uncemented) constrained cup in 8 cases, and the G7® OsseoTi® cup with the Freedom system (Zimmer-Biomet) in 3 cases.
The DM implants were the cemented Polarcup® cup (Smith & Nephew) in one case; the G7® Osseoti® cup with a modular DM liner (Zimmer-Biomet) in 9 cases, and the Delta® TT cup (LIMA) in 7 cases. Within the group of patients who received the Delta® TT cup, the Delta® TT system with anti-protrusion wings was used in 4 cases.
For the remaining cases, other than those involving DM or constrained implants, the uncemented G7® OsseoTi® cup with the Freedom system (Zimmer-Biomet) was used, except for one case in which a flange was fabricated intraoperatively to prevent dislocation using the Olerud technique with a fragment of a Contemporary polyethylene insert (Smith & Nephew).
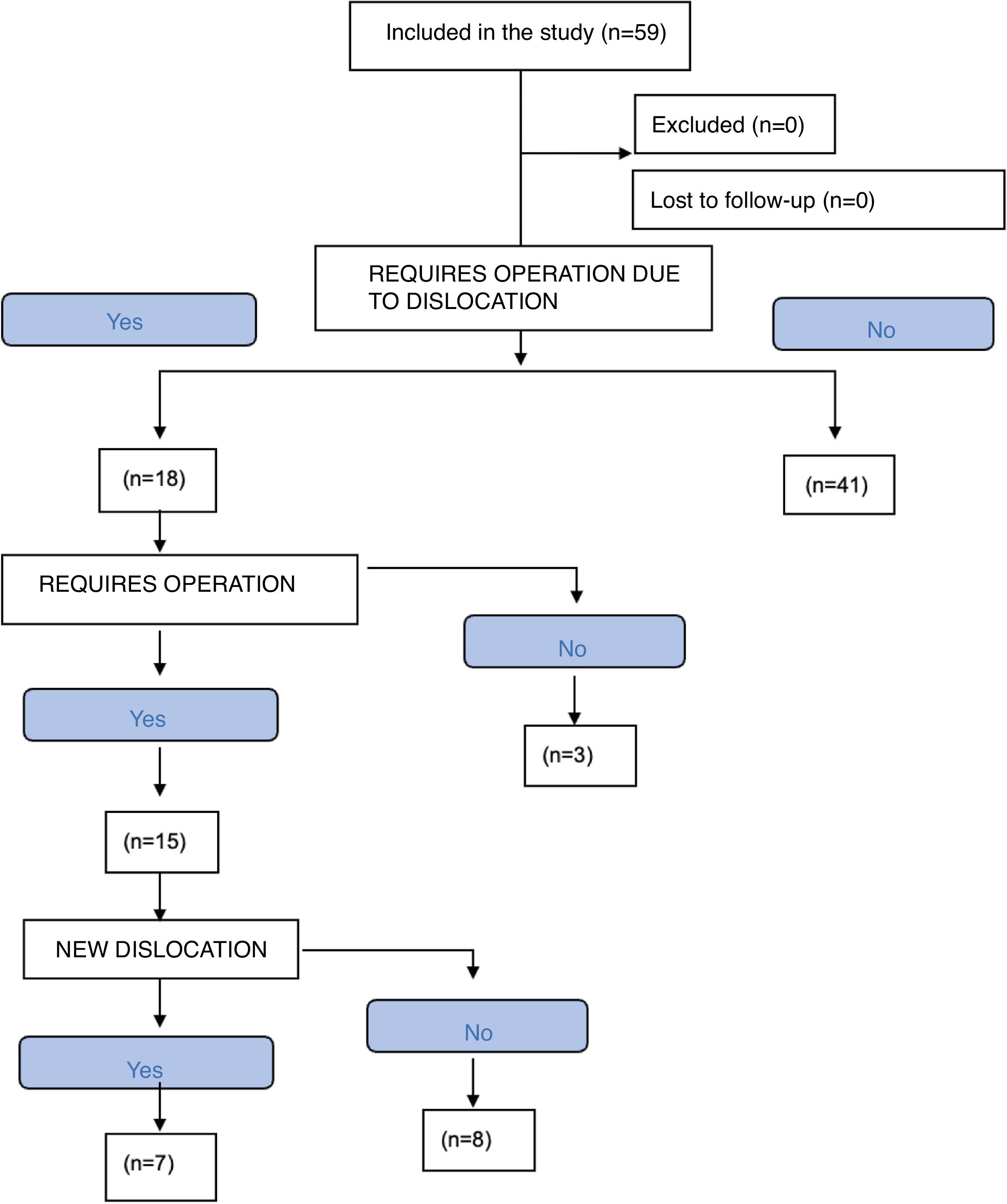
Dislocation recurrence and reoperationOf a total of 59 cases included in our series, dislocation recurrence was observed in 18 patients (30.5%) on one occasion, while 7 patients (12%) experienced recurrences in two or more episodes. Reoperation was performed in 15 cases (25%), with a range of 1–5. The main factors leading to reoperation were prosthetic instability, infection, and peri-prosthetic fractures (Fig. 3).
Only one case had a history of lumbar instrumentation (1.69%). Of all the patients evaluated, we identified 0 dislocations in the group with lumbar instrumentation and one dislocation in the group without lumbar instrumentation.
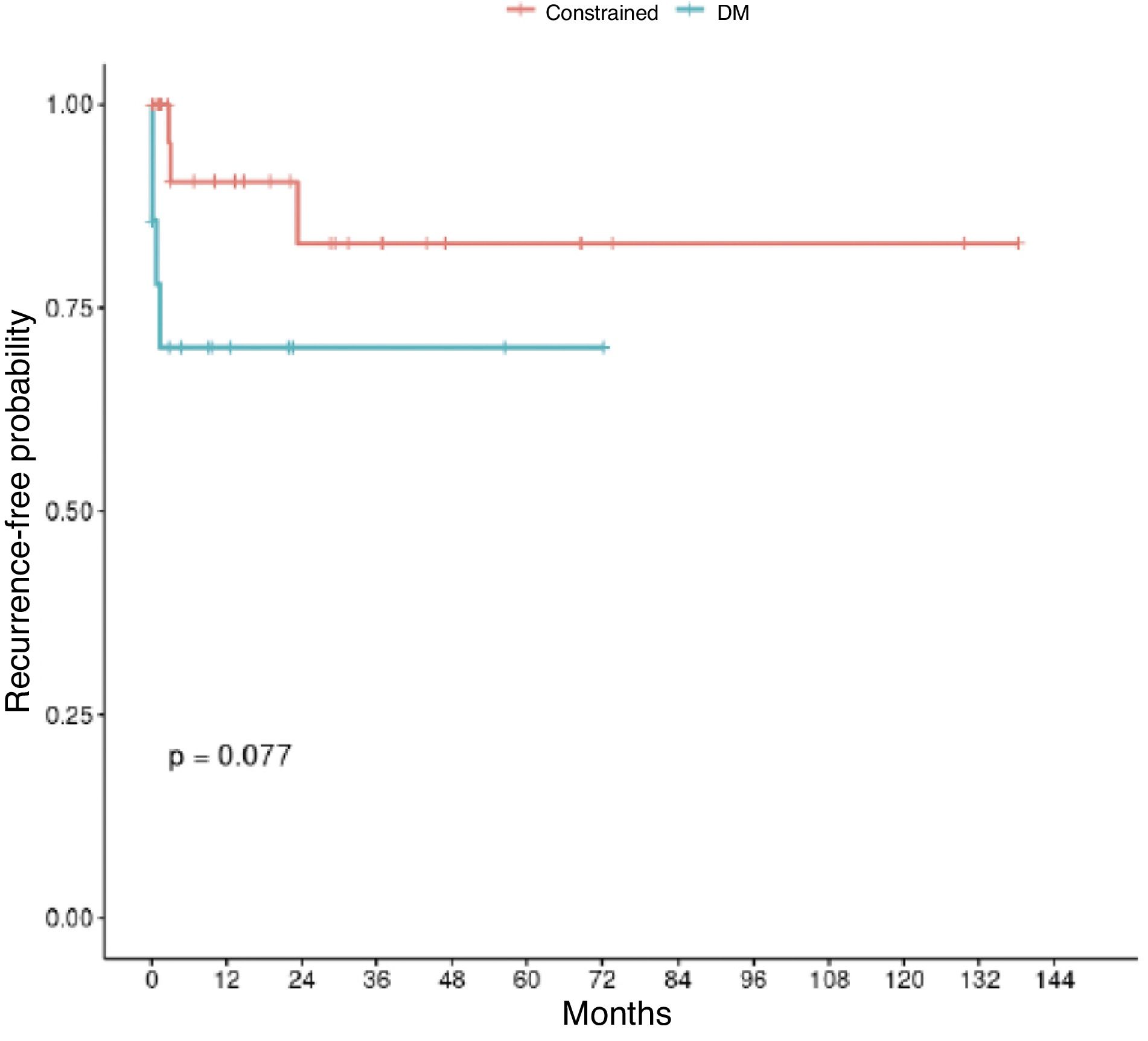
Statistical analysis characteristicsA significant relationship was identified between the year of surgery and the type of implant used (Fisher's test; p=.042). However, no association was found between dislocation recurrence and implant type (Fisher's test; p=.51). Regarding recurrence on two or more occasions, no significant association was observed with implant type (Pearson's chi-squared test; p=.524).
We analysed recurrence due to dislocation, and the follow-up time was the difference between the date of surgery and the date of recurrence, if it occurred, or the date of last contact in other cases. The recurrence-free probability at one year was 80.5% and at two years, 70.6%. No significant differences were detected between the groups (p=.077) (Fig. 4).
The sample size of patients with lumbar instrumentation did not allow conclusions to be drawn regarding the risk of dislocation in patients with instrumentation.
DiscussionInstability in total hip arthroplasty (THA) can be due to a variety of factors, including surgical approach; lack of posterior capsular repair; patient factors; surgeon factors, and implant positioning. Achieving the ideal position of prosthetic implants is challenging, even for the most experienced surgeons.5,6
Treatment of instability depends on the timing of presentation, whether early or late. Treating chronic instability after primary THA is a difficult task, even for experienced surgeons. Wera et al. provide guidance on the management of this complication, although optimal treatment options may vary by case.7
The results of our study determined that the main cause of instability after THA is acetabular, followed by injury to the abductor mechanism, which correspond to types I and III of the Wera classification, respectively.7–9 Saiz et al. stated that the acetabular cause alone does not guarantee instability, since its aetiology is multifactorial.10 Currently, a comprehensive review has been conducted on the relationship between pelvic imbalance and acetabular anteversion, which has become a topic of further research. Zanirat et al. presented a meta-analysis showing that patients with lumbar fusion have a higher risk of dislocation with an OR of 2.5, and its value increases in direct relation to the number of levels fused before or after THA.11 It is striking how there is a growing number of articles in the literature that emphasise lumbar instrumentation and its relationship with the increased incidence of dislocation.12–14 In our series, only one patient had this history, so we could consider it a non-relevant history in our setting.
The use of DM implants in THA has been increasing and has been shown to be effective in reducing instability in high-risk patients. Heckmann et al. reported that the use of DM implants in primary THA increased from 5.7% in 2012 to 12.0% in 2018, and from 19.5% to 30.6% in revision THA.15 In our centre, 11.7% (2/17 cases) of revision THAs were observed due to instability with the use of DM implants compared to 3.2% (1/31 cases) with constrained implants. Both have been shown to be highly effective in reducing instability in high-risk patients.
Donovan et al. demonstrated that DM implants in the context of revision THA have lower incidences of dislocation (3% vs. 9%), re-revision for dislocation (2% vs. 9%), and revision for any cause (8% vs. 19%) compared to constrained acetabular components.16 Similarly, Pai et al. demonstrated that their properties contribute to greater stability of the THA, providing improved mid-term survival with improved clinical performance.17 Similar results were presented by Gallego et al.18
Although there has been a higher prevalence of constrained implant use in our centre, DM implants have been preferred, especially since 2020, following trends suggested in the medical literature. However, although not statistically significant, the success rate in preventing dislocation has been lower than that of constrained implants.
LimitationsThis study presents the limitations inherent to a retrospective study, such as the lack of CT scans for all patients, the potential variability in surgical indications based on the surgeon's preference for a DM or constrained implant, and the lack of a standardised tool for patient-perspective outcome measurement (PROMs) or quality of life measurement, which would provide more detailed information on outcomes with one system or another.
ConclusionsThis study confirms that hip prosthesis dislocation has a multifactorial aetiology, with malposition of the acetabular component being the primary cause in 61% of cases, and only 30% of dislocations were within the Lewinnek zone.
This finding underscores the need to improve the accuracy of cup orientation through the use of advanced technologies such as navigation or robotics. Although constrained and DM implants were the predominant strategies for treating instability, and both showed similar effectiveness, dislocation recurrence remained at 31%, revealing that instability remains a significant challenge in revision surgery.
The overall success rate was 69%, slightly higher in constrained cups (74.29%) than in DM cups (62.50%), but the statistical relationship was not significant in terms of preventing the first dislocation (p=.51) or recurrence on two or more occasions. Similarly, no significant association was found (p=.524). This shows that the type of implant does not affect the frequency of dislocations. Furthermore, our study showed that the probability of not experiencing recurrence at one year was 80.5%, and at two years, it was 70.6%. This means that the majority of patients did not experience recurrences, although no significant differences were found between the study groups (p=.077).
These results highlight the importance of precision in primary hip prosthesis implantation to prevent dislocations, with more precise surgical techniques. Furthermore, our experience with success in preventing dislocation is similar between DM and constrained cup systems.
Level of evidenceLevel of evidence III.
Ethical considerationsThe study was approved by the Ethics Committee of the Hospital Clínic Barcelona. Data confidentiality will be guaranteed.
FundingThe study did not receive any external funding.
Conflict of interestsThe authors have no conflict of interests to declare in this study.