Posterior malleolus fractures are frequent injuries, present in 7–44% of all ankle fractures.
The objective of this study is to review the evidence to indicate the fixation of this fracture and to choose the appropriate surgical approach.
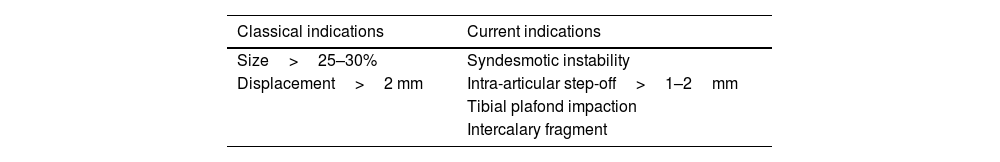
The classic indications for fixation were fragment size greater than 25–30% of the articular surface and displacement greater than 2mm. However, current evidence suggests that, rather than size, factors such as syndesmotic instability, intra-articular step-off greater than 1–2mm, plafond impaction and the presence of intercalary fragments should be considered.
When comparing the different surgical approaches, the literature supports the use of posterior approaches and reserves the recommendation of the traditional approach for exceptional cases.
For the treatment of this injury it is essential to know the anatomy of the ankle and to consider all the factors described above, in addition to the presence of concomitant injuries.
Las fracturas del maléolo posterior están presentes en el 7 al 44% del total de fracturas de tobillo. El objetivo de esta revisión es conocer la evidencia actual sobre las indicaciones de fijación interna y la elección del abordaje quirúrgico para el tratamiento de estas fracturas.
Las indicaciones clásicas de fijación eran el tamaño mayor al 25-30% de la superficie articular y el desplazamiento mayor de 2mm; sin embargo, la evidencia actual sugiere que, en lugar del tamaño, se deben considerar factores tales como la inestabilidad sindesmal, el escalón articular mayor de 1-2mm, la impactación de la superficie articular y la presencia de fragmentos intercalares. Al comparar las vías de abordaje, la bibliografía apoya el uso de los abordajes posteriores, reservando la recomendación de abordaje anterior para casos excepcionales. Para el tratamiento de esta lesión es fundamental conocer la anatomía del tobillo y considerar los factores descritos, además de la presencia de lesiones concomitantes.
Fractures of the ankle are common injuries, accounting for 9% of all fractures, and up to 7–44% are associated with fractures of the posterior malleolus.1–3
Earle first described fracture of the posterior tibial rim in 1828.4 Studies suggest that evaluation with plain ankle radiographs is insufficient, as computed tomography (CT) modifies operative planning in 20–44% of cases.5
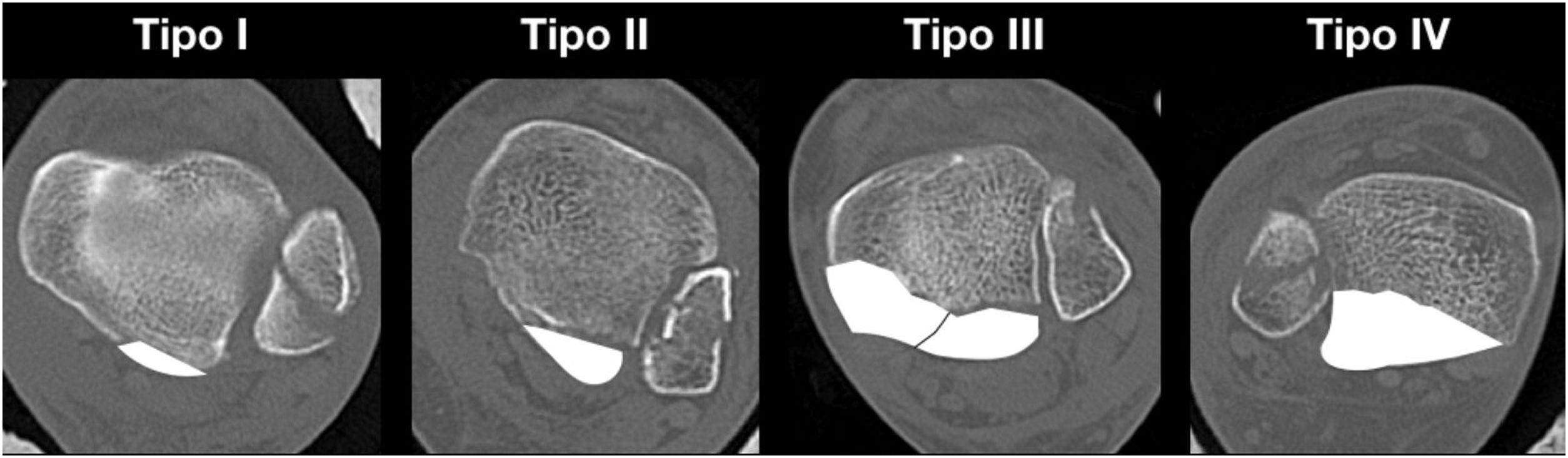
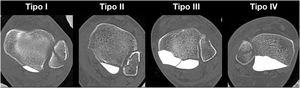
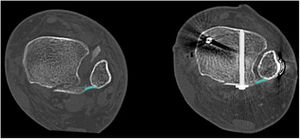
Because CT enables better characterisation of this fracture, it has been used by various authors to describe classifications.6–8 A CT-based classification with three-dimensional reconstruction is currently the most widely used, described in 2015 by Bartoníček and Rammelt, who distinguish five types of fracture of the posterior malleolus (PMF): type I (extraincisural), type II (posterolateral fragment), type III (posteromedial and posterolateral fragments), type IV (large posterolateral triangular fragment), and type V (irregular osteoporotic fracture) (Fig. 1). The importance of this classification lies in its prognostic and therapeutic implications; it allows us to determine the surgical indication and the best surgical approach in each case. The authors recommend conservative treatment in type I, surgery with posterolateral approach in type II and IV, and posteromedial approach or double approach (posterolateral and medial with posteromedial extension) in type III.8,9
This, together with a better understanding of the normal anatomy and biomechanics of the ankle joint, has resulted in a paradigm shift in the indications for internal fixation and also in the approach routes that can be chosen.
The aim of this study is a review of the literature on current indications for internal fixation of PMF.
Indications for internal fixation of PMFThe classical indications for PMF fixation were displacement greater than 2mm on lateral radiograph and fragment size greater than 25–30% of the tibial plafond.3,10 The rationale behind this size was the apparent increased risk of posterior talar subluxation and poorer functional outcomes.3,11
A change in thinking in PMF began to take place in 2011, when a survey of 401 surgeons was published and only 29% used the threshold of size greater than 25% as an indication for fixation and 56% responded that the indication for fixation depends on “stability and other factors”.12 These various factors influencing the indication for fixation and their current evidence are discussed in this article.
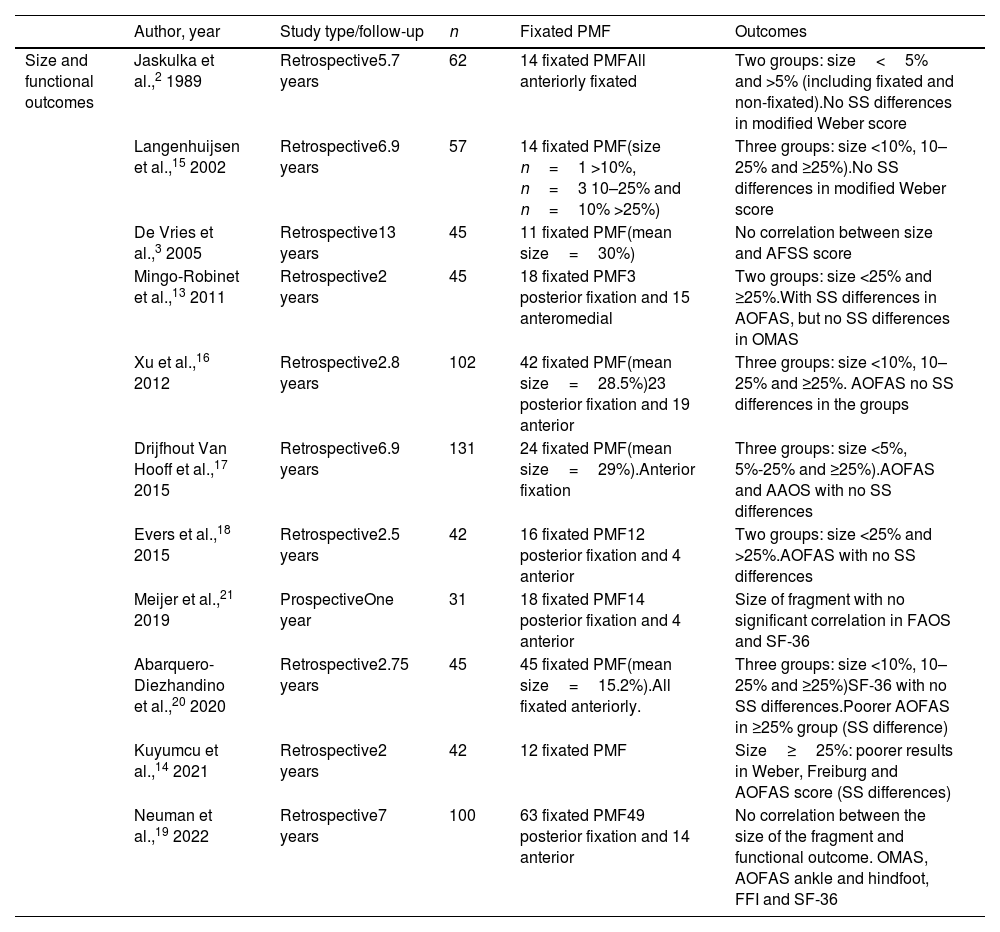
Fragment sizeThe size of the PMF was typically measured in relation to the percentage of the tibial plafond involved, and assessed in a lateral ankle projection (Fig. 2). Several clinical studies have addressed the relationship between fragment size and posterior subluxation of the talus,3 the patient's functional outcome,2,3,13–21 and the development of post-traumatic osteoarthritis3,10,16–18,20,21 (Table 1).
Summary of clinical studies on the relationship between PMF size and functional outcomes.
| Author, year | Study type/follow-up | n | Fixated PMF | Outcomes | |
|---|---|---|---|---|---|
| Size and functional outcomes | Jaskulka et al.,2 1989 | Retrospective5.7 years | 62 | 14 fixated PMFAll anteriorly fixated | Two groups: size<5% and >5% (including fixated and non-fixated).No SS differences in modified Weber score |
| Langenhuijsen et al.,15 2002 | Retrospective6.9 years | 57 | 14 fixated PMF(size n=1 >10%, n=3 10–25% and n=10% >25%) | Three groups: size <10%, 10–25% and ≥25%).No SS differences in modified Weber score | |
| De Vries et al.,3 2005 | Retrospective13 years | 45 | 11 fixated PMF(mean size=30%) | No correlation between size and AFSS score | |
| Mingo-Robinet et al.,13 2011 | Retrospective2 years | 45 | 18 fixated PMF3 posterior fixation and 15 anteromedial | Two groups: size <25% and ≥25%.With SS differences in AOFAS, but no SS differences in OMAS | |
| Xu et al.,16 2012 | Retrospective2.8 years | 102 | 42 fixated PMF(mean size=28.5%)23 posterior fixation and 19 anterior | Three groups: size <10%, 10–25% and ≥25%. AOFAS no SS differences in the groups | |
| Drijfhout Van Hooff et al.,17 2015 | Retrospective6.9 years | 131 | 24 fixated PMF(mean size=29%).Anterior fixation | Three groups: size <5%, 5%-25% and ≥25%).AOFAS and AAOS with no SS differences | |
| Evers et al.,18 2015 | Retrospective2.5 years | 42 | 16 fixated PMF12 posterior fixation and 4 anterior | Two groups: size <25% and >25%.AOFAS with no SS differences | |
| Meijer et al.,21 2019 | ProspectiveOne year | 31 | 18 fixated PMF14 posterior fixation and 4 anterior | Size of fragment with no significant correlation in FAOS and SF-36 | |
| Abarquero-Diezhandino et al.,20 2020 | Retrospective2.75 years | 45 | 45 fixated PMF(mean size=15.2%).All fixated anteriorly. | Three groups: size <10%, 10–25% and ≥25%)SF-36 with no SS differences.Poorer AOFAS in ≥25% group (SS difference) | |
| Kuyumcu et al.,14 2021 | Retrospective2 years | 42 | 12 fixated PMF | Size≥25%: poorer results in Weber, Freiburg and AOFAS score (SS differences) | |
| Neuman et al.,19 2022 | Retrospective7 years | 100 | 63 fixated PMF49 posterior fixation and 14 anterior | No correlation between the size of the fragment and functional outcome. OMAS, AOFAS ankle and hindfoot, FFI and SF-36 |
AAOS: American Academy of Orthopaedic Surgeons; AFSS: Ankle Fracture Scoring System; AOFAS: American Orthopaedic Foot & Ankle Society; FAOS: Foot and Ankle Outcome Score; FFI: Foot Function Index; n: number of patients with PMF; OMAS: Olerud Molander Ankle Score; SF-36: SF-36 Health Survey; SS: statistically significant.
In relation to posterior talar subluxation, De Vries et al.3 in a retrospective clinical study concluded that fragment size was larger in patients with subluxation, and this difference was statistically significant. In a cadaveric study, Raasch et al.22 resected 10%, 20%, 30%, and 40% of the articular surface in a group that had no other bone or ligament injuries vs. a group that also underwent a section of the anterioinferior tibiofibular ligament (AITFL) and osteotomy of the fibula. The authors found a posterior translation of less than 1mm, even with resection of 40% of the articular surface in the first group, and in the second group they observed a translation of more than 3mm with resection of 30% of the articular surface, concluding that posterior subluxation of the talus depends mostly on fibular stability and the AITFL, and not on the size of the posterior malleolus fragment. Fitzpatrick et al.23 later confirmed these findings, performing a 50% osteotomy of the articular surface of the tibia to then move the ankle from 25° plantarflexion to 15° dorsiflexion, finding no subluxation.
Fragment size and functional outcomeMingo-Robinet et al.13 reported lower AOFAS score in fragments≥25%. Xu et al.16 evaluated a total of 102 patients divided according to fragment size less than 10%, between 10% and 25%, and greater than 25%, concluding that there were no statistically significant differences in AOFAS and VAS scales. On the other hand, Abarquero-Diezhandino et al.20 in a study that included only patients with indirect reduction through the traditional approach, observed poorer AOFAS scores in fragments larger than 25% of the joint surface; however, they found no statistically significant differences in the SF-36 Health Survey (SF-36) or VAS at rest. Recently, in a retrospective seven-year follow-up study, Neumann and Rammelt found no correlation between fragment size and Olerud Molander Ankle Score (OMAS), AOFAS Ankle and Hindfoot, Foot Function Index (FFI), or SF-36.19 Other studies also reported no differences in functional outcome according to fragment size.2,3,15,18,21
Fragment size and posttraumatic osteoarthritisIt is important to assess the relationship between the size of the posterior malleolus fragment and the development of osteoarthritis, as it is known that malleolar fractures are the leading cause of ankle osteoarthritis (39% of cases).24
Some authors reported a significant decrease in joint contact area with 33% or more joint involvement and suggested that this could predispose to degenerative changes at the joint level.25,26 This was questioned in two other studies that did not find a statistically significant decrease in contact area or maximum stress, in one of which an osteotomy involving 50% of the joint surface was performed.23,27
A retrospective clinical study of 2.8 years of follow-up reports a statistically significant difference in the incidence of osteoarthritis in fractures with fragments larger than 25%.16 Meanwhile, Drijfhout Van Hooff et al.17 in a 6.9-year follow-up study report an increased risk of osteoarthritis in fragments larger than 5% of the articular surface. A prospective cohort reports a moderate correlation between fragment size and the development of osteoarthritis; however, the follow-up was only one year.21
Unlike the aforementioned authors, in a retrospective study with a 13-year follow-up, De Vries et al.3 found no correlation between fragment size and the development of osteoarthritis. However, Abarquero-Diezhandino et al.20 concluded that there is a relationship between the development of osteoarthritis and the size of the posterior malleolus fragment; however, they highlight that they found no statistically significant differences when comparing between their study groups (less than 10%, between 10% and 25%, and greater than 25%).
While some authors have recommended fixation in fragments greater than 25% and, more recently, 5–10% of the articular surface, three systematic reviews conclude that there is insufficient evidence to justify considering size as a factor in PMF fixation, and that it should be determined by other factors.28–30
Syndesmotic instabilityWhen analysing syndesmotic stability as a factor in defining PMF fixation, it is essential to highlight that the posterior tibial tuberosity is the insertion of the posteroinferior tibiofibular ligament (PITFL), which then runs obliquely and distally to its insertion in the posterior fibula. As described by Ogilvie-Harris in a cadaver study, this ligament provides 41.4% of the stability of the syndesmosis, and is the most important of the three that make up the syndesmotic complex.31 Although some authors suggest that the PITFL has a wider insertion at the level of the posterior region of the distal tibia, this important contribution to syndesmotic stability is interrupted, at least partially, when the posterior malleolus fracture involves the fibular incisura.32
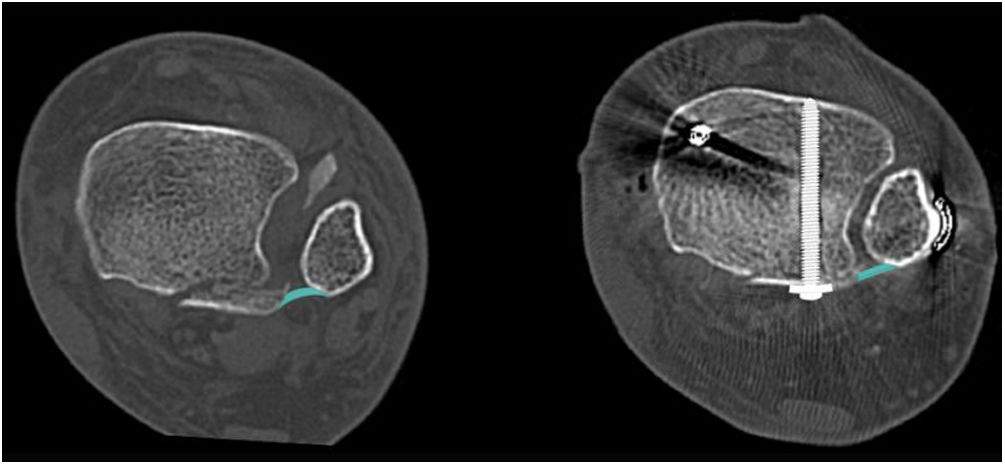
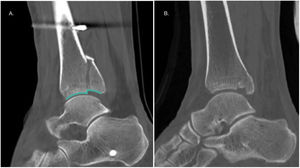
Gardner et al.33 conducted a study in 10 cadaveric specimens where a stage 4 external pronation-rotation fracture pattern was created and randomly performed posterior malleolus fragment fixation vs. isolated syndesmotic screw fixation, concluding that syndesmotic stability was restored in 70% in the first group and only 40% in the isolated syndesmotic fixation group. Along the same lines, a study of 198 patients evaluating posterior malleolus fixation through an anterior approach (indirect reduction) vs. a posterior approach (direct reduction) concluded that 97.9% of syndesmotic stability was restored in the second group, which was 13 times greater than in the indirect fixation group.34 Consistent with the above, Neumann and Rammelt,19 in a retrospective series of 100 patients with an average follow-up of seven years, conclude that internal fixation significantly reduces the need for syndesmotic fixation (p=.010). Therefore, Bartoníček recommends fixation of all fragments involving the fibular incisura8,9 (Fig. 3).
Presence of intra-articular step-offThe presence of intra-articular step-off is also a widely studied factor in the literature (Fig. 4A). Xu et al. in 2012 reported that a step-off greater than 1mm was associated with poorer American Orthopaedic Foot & Ankle Society (AOFAS) score, less patient satisfaction, and greater post-traumatic osteoarthritis.16 Another 2018 retrospective study in which 169 patients were evaluated found that a step-off greater than 1mm was a risk factor for the development of osteoarthritis regardless of fragment size, which secondarily led to poorer functional outcome.35 Drijfhout Van Hooff et al.17 published in their series a higher frequency of osteoarthritis in the presence of intra-articular step-off ≥1mm. Kang et al.36 published poorer American Academy of Orthopaedic Surgeons (AAOS) and AOFAS scores at six and 12 months in the presence of a step-off greater than 2mm. In the same vein, Meijer et al.,21 in a prospective series, reported a statistically significant relationship between residual intra-articular step-off and a worse score on the Foot and Ankle Outcome Score (FAOS) subscales of pain and symptoms. While there is no consensus on the 1- or 2-mm limit, a recent review by Rammelt et al. recommends internal fixation in the presence of a step-off greater than or equal to 2mm.4,28
Presence of plafond depression/impactionThe presence of plafond depression, also called “die-punch fragment”, may contribute to subluxation of the talus and the development of post-traumatic osteoarthritis.37,38 The latter would be due to a redistribution of loading towards the anteromedial region of the articular surface, which would put stress on areas of chondrocytes that are not normally subjected to such loads23 (Fig. 4B).
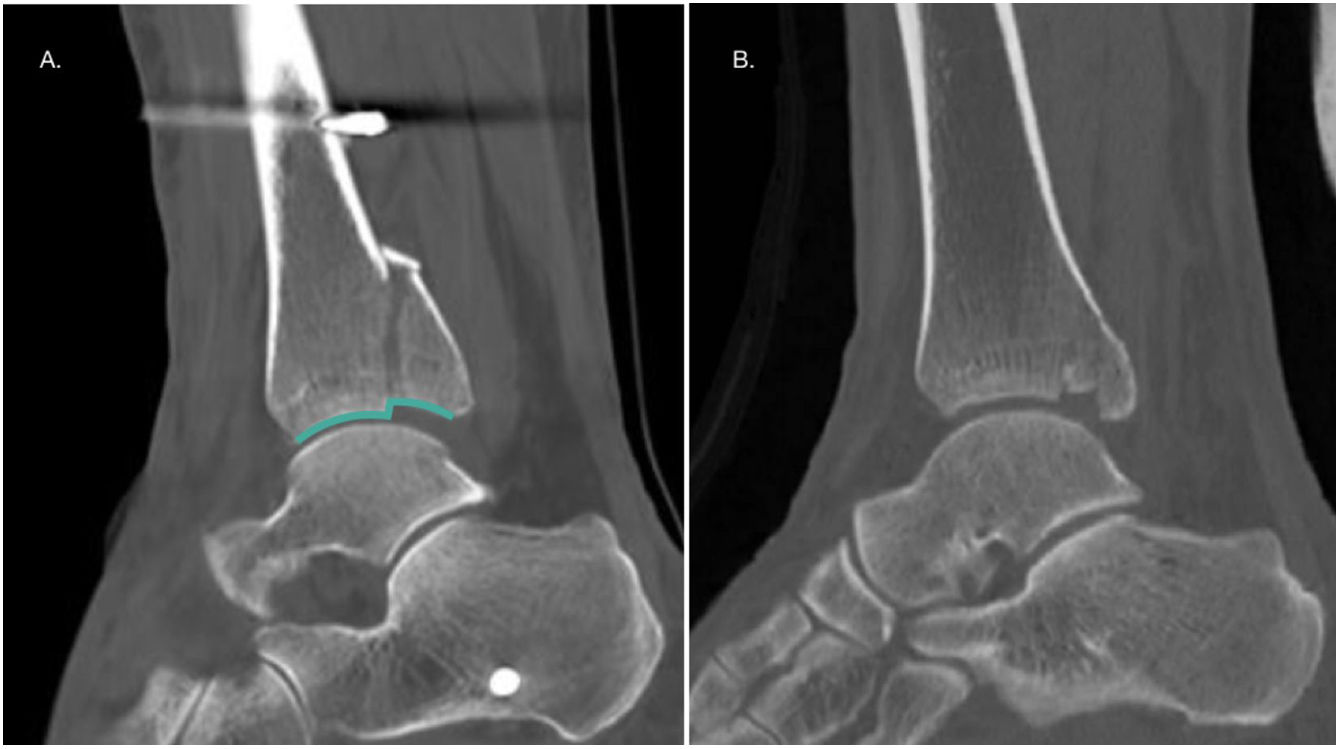
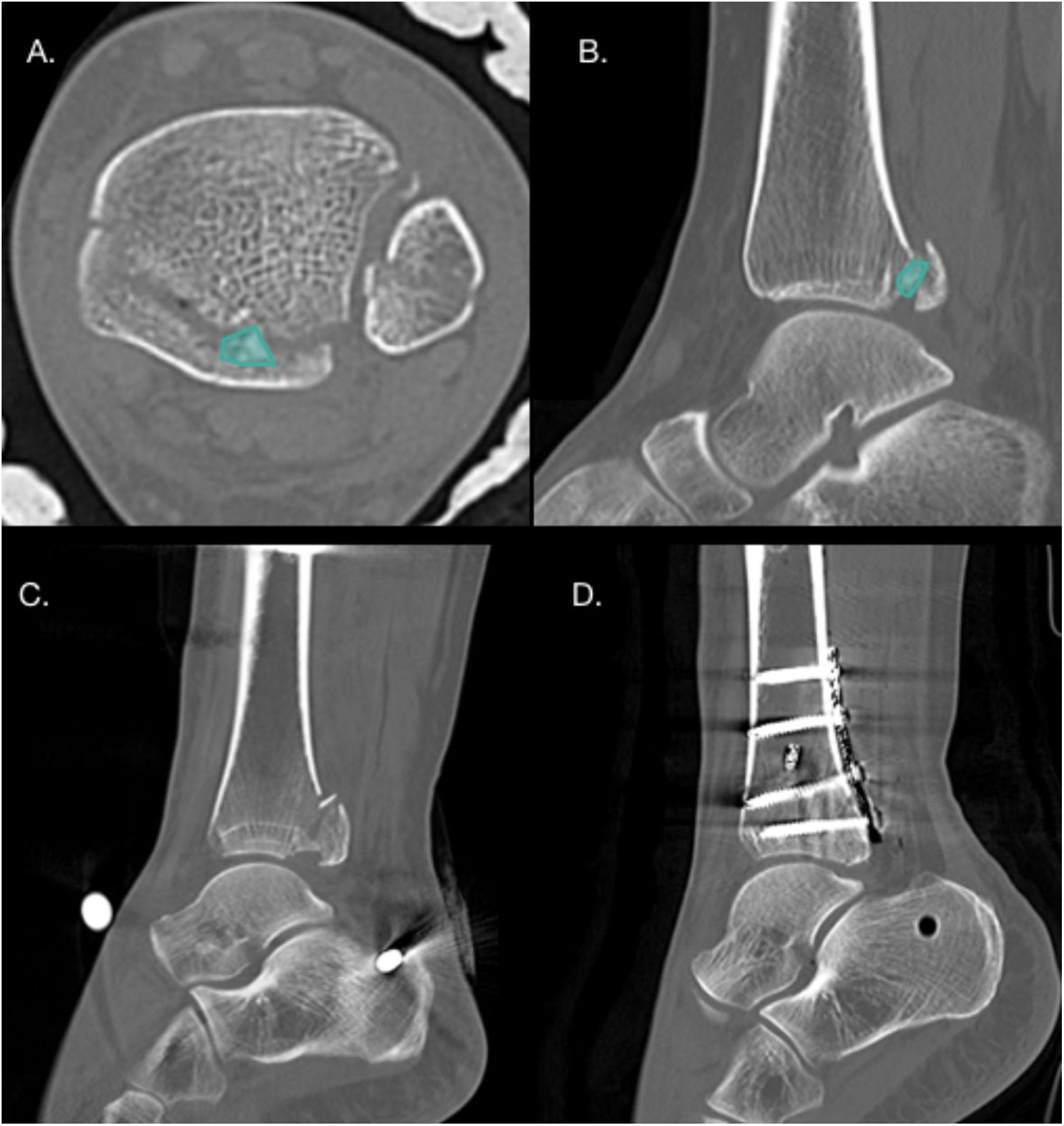
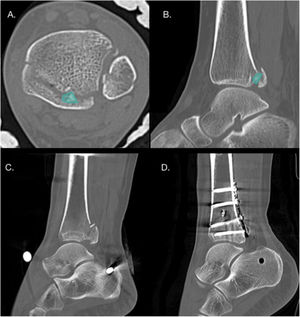
Presence of intercalary fragmentsIntercalary fragments are considered a separate factor, as they may or may not be in the context of a joint collapse, and may be fragments of the posterior tibial cortex, not just articular fragments. These fragments have an incidence of 43% in PMF, up to 70% in Bartoníček type III fractures19,37 (Fig. 5). The most frequent location of these fragments is posterolateral in 64% of cases.37 Normally these fragments prevent anatomical reduction of the fracture, and therefore it is recommended that small fragments be removed to prevent them from acting as intra-articular free bodies, and it is recommended that larger fragments be synthesised.1
(A and B) Axial and sagittal CT slices showing the presence of an intercalary fragment in a patient with Bartoníček and Rammelt type III PMF. (C and D) Pre- and postoperative CT sagittal slices in a patient with Bartoníček PMF and Rammelt type II with an intercalary fragment that was fixated via a posterolateral approach.
Once the indication for fixation of the PMF has been established, we must define whether to use a traditional anterior approach or a posterior approach.
Traditional (anterior) approach in PMF fixation requires indirect reduction by ligamentotaxis through dorsiflexion of the ankle and fixation with an anteroposterior screw.4 The advantages of this approach are the possibility of fixation of the fracture in the supine position and a minimally invasive approach. However, its disadvantages are the difficulty of obtaining an anatomical reduction, the impossibility of removing intercalary fragments or reducing plafond depression, the difficulty of fixation when small posterolateral fragments are present, and the risk of injury to anterior anatomical structures such as the anterior tibial tendon, the extensor hallucis longus tendon, and the branches of the superficial fibular nerve. To reduce this risk, it is recommended that the anteroposterior screw insertion site be medial to the anterior tibial tendon, with meticulous dissection.39
As studies on this fracture have increased and the importance of anatomical reduction has been understood, numerous posterior approaches have been described. These have the advantage of allowing direct, and therefore anatomical, reduction, stable plate/screw fixation, and intercalary fragment removal. The disadvantages of these approaches are the risk of injury to neurovascular structures and the difficulty in reducing quadrimalleolar fractures and fractures of the anterior colliculus of the medial malleolus in the prone position.9
Traditional vs. posterior approachesWhen analysing the quality of reduction, Drijfhout Van Hooff et al. reported 42% malreduction with the traditional approach, defining malreduction as an intra-articular step-off greater than 1mm.17 Vidović et al. reported 23% malreduction with the anterior approach and only 4% with posterior approaches, in this study the presence of an intra-articular step-off greater than 2mm was considered malreduction.40
In terms of functional outcomes, Pilskog et al. obtained similar results between both types of approach in the SEFAS, RAND-36, and VAS questionnaires; however, they described less need for syndesmotic fixation (14% vs. 49%) in posterior approaches.41 In turn, Erinç et al. published statistically significant differences in the SF-36 and FAOS questionnaires in favour of posterior approaches.42
Finally, in relation to the risk of complications, a systematic review and meta-analysis reports no significant differences in the relative risk of complications, but when analysing each complication in isolation, it concludes a higher risk of infection in posterior approaches (p=.01) and a higher risk of postoperative and osteosynthesis-related pain in surgeries that did not use a posterior approach. On this last point, it is important to note that it was not possible to isolate the complications of the anterior approach, as in most cases lateral and/or medial approaches were required in addition to the anterior approach.43
Posterior approaches to the ankle are classically performed in the prone position and can be posterolateral or posteromedial. The posterolateral approach uses the gap between the peroneal tendons and flexor hallucis longus; and the posteromedial approach uses the space between the flexor digitorum longus and flexor hallucis longus, displacing the neurovascular structures laterally.
Multiple modifications of these approaches have been described. For the posteromedial approach, a modification has been proposed maintaining the prone position, but with displacement of the neurovascular structures medially (mpPM) and a modification with the patient in the supine position, abduction of the hip and flexion of the knee (in a “4” position), retracting the posterior tibial tendon anteriorly (msPM)44 (Fig. 6).
Assal et al. described that the mpPM approach, with displacement of the neurovascular structures medially, allows 91% visualisation of the posterior surface of the tibia.45 In addition, Mitsuzawa et al. demonstrated that this approach generates less soft tissue retraction force medially with a lower risk of neurovascular injury when visualisation of the posteromedial region of the tibia is required.46
DiscussionFor many years, the recommendation was that posterior malleolus size greater than 25–30% was an indication for fixation. Some studies then postulated that the limit for fixation would be fragments greater than 10% of the articular surface.15 There is currently no evidence to recommend a size limit for fixation of this fracture.
The PITFL originates from the posterior malleolus and runs obliquely to the posterior border of the fibula. Its importance in the stability of the syndesmotic complex has already been demonstrated, and it becomes even more relevant when in PMF involving the incisura, partially or totally losing the stability that the ligament provides.31 This is the basis for recommending fixation in type II, III, and IV fractures, since in all of them there is involvement of the incisura and, therefore, the stability provided to the ankle by the LTFPI is compromised to a degree. Depression of the tibial plafond, the presence of intercalary fragments, and intra-articular step-off are also indications supported by the literature; however, in the latter, there is still no consensus as to whether the limit should be 1 or 2mm4,16,37,38 (Table 2). It should be noted that although rare, isolated, non-displaced PMFs without syndesmotic instability can be treated orthopaedically.47
When comparing the approaches for this fracture, there are no differences between the traditional approach and the posterior approaches in terms of relative risk of complications and there is no consensus in the literature regarding possible differences in functional outcomes.41,42 However, a lower rate of malreduction and consequently less need for syndesmotic fixation in posterior approaches has been reported. This is because an anatomical reduction of the posterior malleolus facilitates reduction of the fibula in the incisura.17,40–42 Therefore, in the presence of a PMF where fixation is indicated, posterior approaches are recommended.5,48
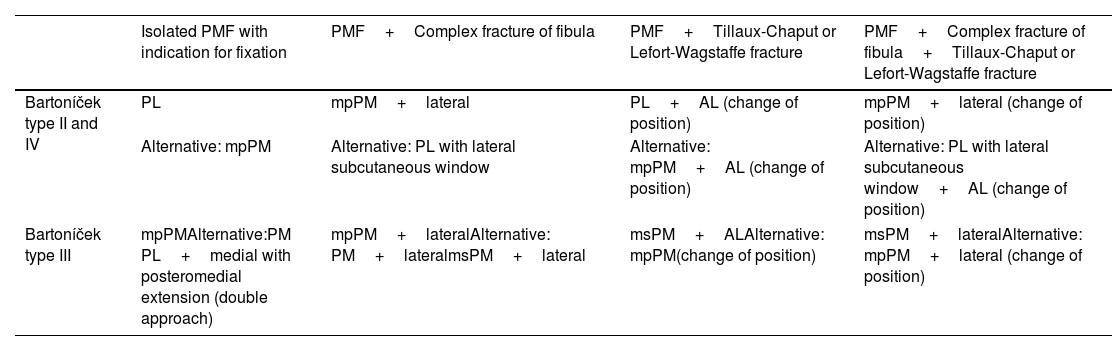
For the choice between a posterolateral and posteromedial approach, the recommendations of Bartoníček and Rammelt have already been described, based on the morphology of the PMF, suggesting a posterolateral approach for type II and IV fractures and a posteromedial approach or double approach (posterolateral and medial with posteromedial extension) for type III fractures.4 As an option, they propose a transfibular approach in selected cases with Weber B fractures of the lateral malleolus initiating at the level of the joint, or a traditional (anterior) approach in Bartoníček and Rammelt type IV fractures without intra-articular step-off or intercalary fragments.4,8
Other authors add to the morphology of the PMF the importance of concomitant injuries that may modify operative planning. In this regard, in the presence of a Bartoníček type II or IV fracture associated with a complex fracture of the fibula, the posterolateral approach with a subcutaneous window for lateral fixation of the fibula, or otherwise a modified prone posteromedial approach associated with a lateral approach, has been recommended. On the other hand, in the presence of a Bartoníček type III fracture associated with Tillaux-Chaput or Lefort-Wagstaffe fractures, a modified supine posteromedial approach combined with a lateral approach or a prone posteromedial approach and subsequent change to supine for an anterolateral approach48,49 (Table 3) has been recommended. In all cases it is recommended to maintain a skin bridge of at least 6cm between approaches and ideally respect the angiosomes of the ankle.48
Summary of surgical approach options according to PMF morphology and concomitant lesions.
| Isolated PMF with indication for fixation | PMF+Complex fracture of fibula | PMF+Tillaux-Chaput or Lefort-Wagstaffe fracture | PMF+Complex fracture of fibula+Tillaux-Chaput or Lefort-Wagstaffe fracture | |
|---|---|---|---|---|
| Bartoníček type II and IV | PL | mpPM+lateral | PL+AL (change of position) | mpPM+lateral (change of position) |
| Alternative: mpPM | Alternative: PL with lateral subcutaneous window | Alternative: mpPM+AL (change of position) | Alternative: PL with lateral subcutaneous window+AL (change of position) | |
| Bartoníček type III | mpPMAlternative:PM PL+medial with posteromedial extension (double approach) | mpPM+lateralAlternative: PM+lateralmsPM+lateral | msPM+ALAlternative: mpPM(change of position) | msPM+lateralAlternative: mpPM+lateral (change of position) |
AL: anterolateral approach; PL: posterolateral approach; PM: classical posteromedial approach; mpPM: modified prone posteromedial approach; msPM: modified supine posteromedial approach.
In summary, the authors recommend CT in all PMF, whether isolated or in the context of bimalleolar, trimalleolar, or quadrimalleolar fractures. In addition, we recommend direct internal fixation of the posterior malleolus through a posterior approach (posterolateral, posteromedial, or their modifications). Fixation of this fragment should be the first stage of the surgery, as it facilitates fibular reduction and also enables assessment of the quality of the reduction of the articular surface on lateral fluoroscopic projections, which is difficult when the lateral malleolus has been previously synthesised. After fixation of all the malleoli involved, we recommend assessing the stability of the syndesmosis and, if in doubt, performing an arthroscopic examination with an anterior approach for evaluation and possible treatment.50
Finally, it is extremely important to know the anatomy of the ankle when planning treatment of a fracture, and also to understand that this treatment must be “à lacarte”, i.e., it must cover all the factors associated with the posterior malleolus as described above, in addition to concomitant injuries, whether fractures of the lateral or medial malleolus, Tillaux-Chaput and Lefort-Wagstaffe fragments, ligament injuries, osteochondral injuries, inter alia.
ConclusionsThe treatment of PMF requires optimal surgical planning that will depend on the type of fracture according to the preoperative ankle CT scan, but will also depend on the patient's comorbidities and the state of the soft tissues.
Internal fixation of this fracture is suggested in the presence of syndesmotic instability, intra-articular step-off greater than 1–2mm, impaction of the tibial plafond and intercalary fragment.
We recommend the posterior approach as the route of choice to achieve anatomical reduction of the fracture and reduce the need for trans-syndesmotic fixation. The use of a traditional anterior approach may be considered in the presence of large fragments without intercalary fragment, step-off or tibial plafond depression.
Level of evidenceLevel of evidence ii.
FundingNo funding was received for this paper.
Conflict of interestsThe authors have no conflict of interests to declare.