Phalangeal fractures are the most common hand fractures. In the last years, intramedullary compression screw (IMHCS) for instable transverse or short oblique proximal P1 fractures have been described. Although both anterograde (intraarticular or trans-articular) and retrograde IMHCS techniques have shown good results, no comparison between anterograde and retrograde screw in P1 fractures has been published. We sought to determine stability with retrograde IMHCS and anterograde IMHCS, both trans-articular and intra-articular technique, in a cadaveric transverse proximal P1 fracture model, at two different levels.
Material and methodsWe performed a biomechanical study in 30 fresh-frozen human cadaveric P1 fracture model. Fracture was performed at 9-mm from the metacarpo-phalangeal (MCP) joint in 15 specimens, whereas it was done at 15mm in the other 15. In turn, in each group, five fractures were stabilised with an anterograde intra-articular IMHCS, five with anterograde trans-articular IMHCS and other five with retrograde IMHCS.
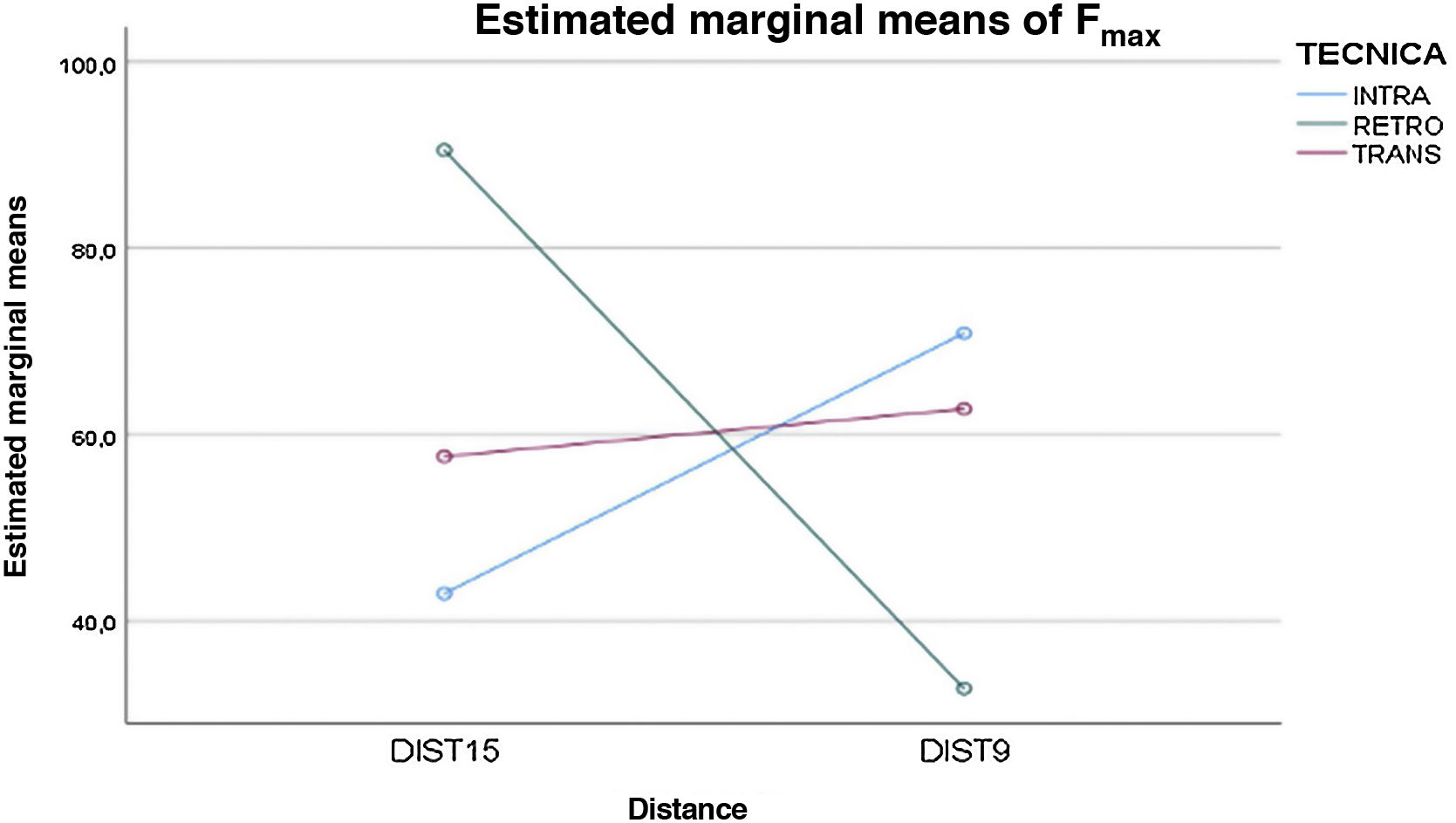
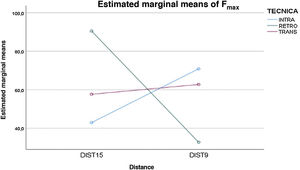
ResultsAnterograde IMHCS fixation in 9-mm P1 fractures (both trans- and intra-articular technique, 62.74N and 70.86N, respectively) was found to be more stable than retrograde IMHCS one (32.72N) (p=0.022). Otherwise, retrograde IMHCS fixation was found to be more stable in more distal P1 fractures (90.52N retrograde vs. 57.64N trans-articular vs. 42.92N intra-articular; p=0.20).
ConclusionsAnterograde IMHCS fixation in proximal transverse P1 bone cut in a cadaveric model provides more stability than retrograde IMHCS, while retrograde screw provides more stability when the bone cut is located more distal.
Las fracturas de falange proximal (FP) son las fracturas más frecuentes de la mano. En los últimos años, se ha descrito el uso de tornillos endomedulares sin cabeza (TESC) para las fracturas inestables transversas u oblicuas de la FP. A pesar de que tanto la técnica anterógrada como retrógrada con TESC han mostrado buenos resultados, no se ha publicado ningún estudio comparativo de su uso en fracturas de FP. Nuestro objetivo es determinar la estabilidad que se obtiene con el uso de TESC retrógrados y anterógrados en un modelo en cadáver de fractura transversa proximal de FP, a dos niveles diferentes.
Material y métodosRealizamos un estudio biomecánico en 30 modelos de fractura de FP de cadáver fresco-congelado. La osteotomía se realizó a los 9 mm desde la articulación metacarpofalángica en 15 especímenes, y a una distancia de 15 mm en los otros 15. A su vez, en cada grupo, cinco osteotomías se estabilizaron con un TESC anterógrado intraarticular, cinco mediante un TESC anterógrado transarticular y cinco con un TESC retrógrado.
ResultadosLa fijación con TESC anterógrado en osteotomías realizadas a los 9 mm (tanto con la técnica transarticular como intraarticular, 62,74 N y 70,86 N, respectivamente) fue más estable que la fijación con TESC retrógrado (32,72 N) (p 0,022). Por otra parte, la fijación con TESC retrógrado fue más estable en el modelo de fractura más distal (90,52 N retrógrado vs. 57,64 N transarticular vs. 42,92 N intraarticular (p=0,20).
ConclusionesLa fijación con TESC retrógrado ofrece más estabilidad en fracturas más distales, mientras que las técnicas anterógradas son más estables en fracturas proximales.
Phalangeal fractures are the most common hand fractures, 38% of which are fractures of the proximal phalanx (P1).1 Surgery is reserved for unstable fractures. Of the different techniques described, the most common are K-wire (KW), plate-screw, and intramedullary compression screw (IMHCS). Short oblique and transverse extra-articular P1 fractures have classically been stabilised with two crossed anterograde KWs. Although good results have been reported with this technique,2,3 a complication rate of up to 36% has been described,4 and because it requires a period of postoperative immobilisation, joint stiffness is not uncommon.5 In recent years, the use of both antegrade and retrograde IMHCS has been described as an alternative for this fracture pattern.6,7 Low soft tissue damage is one of its advantages, which allows immediate mobilisation and no need to remove the implant.7
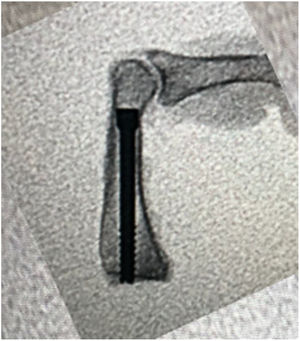
The retrograde IMHCS technique is performed through the head of the phalanx, in maximum flexion of the proximal interphalangeal joint. The anterograde IMHCS technique would theoretically be a better method of osteosynthesis in proximal P1 fractures, as it allows us to better cover the entire segment. Fixation of anterograde IMHCS can be either intra-articular (from the dorsal articular margin of the P1) or trans-articular (through the metacarpal head, which gives an entry point centred on the P1). From a biomechanical point of view, IMHCS have been shown to offer sufficient stability in metacarpal and P1 fractures.8,9 However, we have found no comparative biomechanical study of the use of antegrade and retrograde IMHCS in P1 fractures in the literature.
Our aim is to determine the stability obtained using retrograde and antegrade IMHCS in a cadaveric model of proximal transverse P1 fracture, at two different levels. Our hypothesis is that antegrade IMHCS confers greater stability in proximal P1 fractures, whereas it is equal to retrograde IMHCS if the fracture is more distal.
Material and methodsWe conducted a biomechanical study on 30 fresh-frozen cadaveric P1 fracture models. The age of the specimens was between 86 and 90 years, one male and three females. All fingers except the thumb were included. All fractures were stabilised with a 2.4mm IMHCS (DePuy Synthes, Raynham, MA). The fracture was recreated at 9mm from the metacarpophalangeal (MCP) joint in 15 specimens, and at 15mm in the other 15. In turn, in each group, five osteotomies were stabilised with an intra-articular anterograde IMHCS, five with a transarticular anterograde IMHCS, and the final five with a retrograde IMHCS.
Preparation of the fracture model and fixation techniqueFresh-frozen hands disarticulated at the level of the radiocarpal joint were used. A central longitudinal incision was made to expose the P1 of the triphalangeal fingers. A transverse osteotomy was then performed with a sagittal saw at 9mm from the base of the phalanx on fifteen fingers and at 15mm on the other fifteen. By manual displacement of the osteotomy, we verified the recreation of an unstable bicortical fracture, and it was verified by fluoroscopy. Once the osteotomy had stabilised, all surrounding soft tissues were debrided and the phalanges were collected for further biomechanical study.
Intra-articular antegrade IMHCS techniqueA 1cm transverse dorsal incision was made in the skin at the level of the MCP joint. The extensor tendon was incised longitudinally, and by gentle dorsal subluxation and flexion of the MCP joint, the dorsal proximal articular surface of the P1 was exposed. Once the fracture had been reduced, the guide wire was placed up to the head of the P1. We reamed through the guide wire and placed the cannulated 2.4mm intramedullary compression screw. Using this technique, the entry point of the screw was eccentric and joint damage to the proximal cartilage of the P1 was reduced.
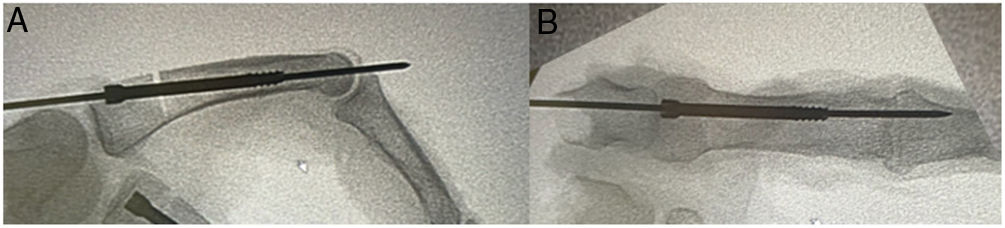
Trans-articular antegrade IMHCS techniqueA 1cm transverse dorsal skin incision was made 1cm proximal to the MCP joint. The longitudinal division of the extensor tendon then allowed access to the dorsum of the metacarpal head. Through the metacarpal head and with maximum flexion of the MCP joint, the guide wire was placed in the centre of the base of the P1. Once the guide wire was placed with the fracture reduced, we reamed through the guide wire and the 2.4mm intramedullary compression screw was placed (Figs. 1 and 2).
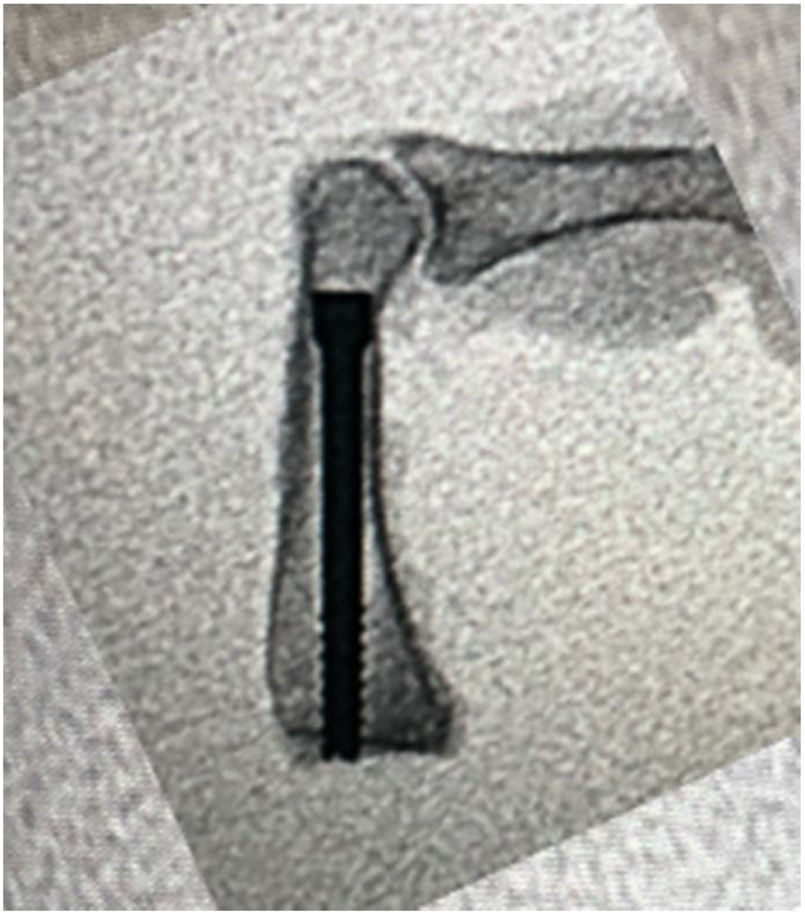
A 1cm transverse dorsal incision was made in the skin at the level of the proximal interphalangeal joint. The extensor apparatus was incised longitudinally and the distal articular surface of the P1 exposed. Once the fracture had been reduced, an intramedullary guide wire was placed down to the subchondral bone at the base of the PF. After reaming through the guide wire, a 2.4mm intramedullary headless screw was inserted (Fig. 3).
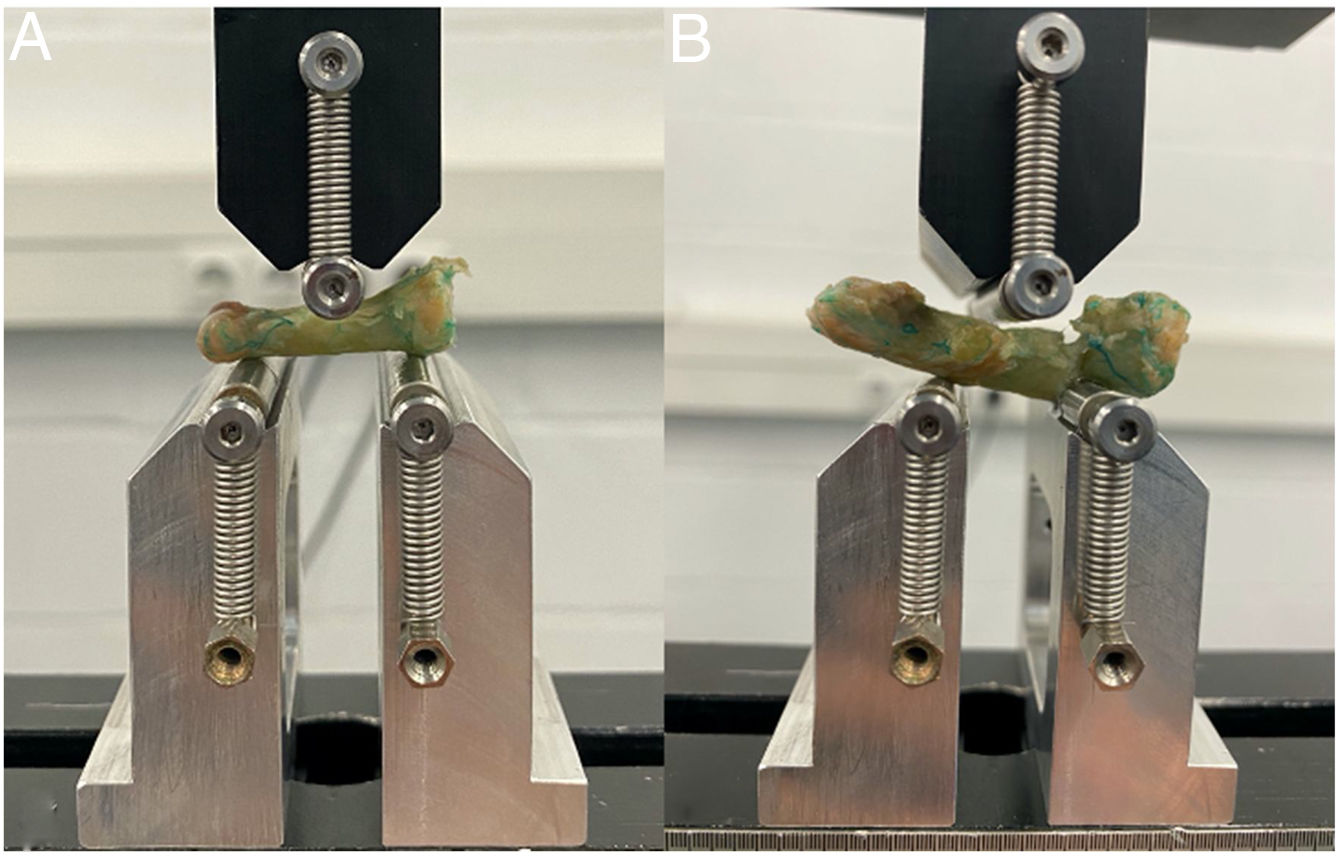
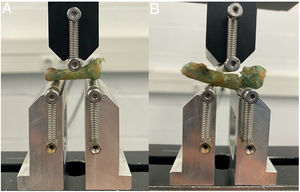
Biomechanical studyThe forces to which transverse or short oblique fractures of the proximal third of the P1 are subjected often involve extension of the fragment due to tendon insertions.10 To reproduce this clinical scenario, a biomechanical 3-point bending test (3 P) was designed. The phalanges obtained were placed horizontally in the test device (Bionix 358®; MTS Systems, Eden Prairie, MN, USA). The distance between the lower supports was constant at 20mm, and the upper support was placed at the midpoint between them (Fig. 4). In all cases, it was ensured that the osteotomy was between the two supports. A load cell of 2.5kN was applied, maintaining a constant displacement rate of 10mm/min until fracture of the construct.11,12
Statistical analysisThe primary outcome was the difference in the mean resistance to the 3 P bending forces between the three IMHCS techniques described. As no applicable data had been published previously, the sample size was calculated based on previous studies with similar designs and test methods,8 assuming potentially underpowered study, which could eventually be expanded. Categorical variables were presented as absolute numbers and percentages, while continuous variables were summarised as medians with interquartile ranges, or means and standard deviations (SD), as appropriate. Comparative analyses were performed using the ANOVA test for continuous variables between groups. All statistical tests were two-tailed, and the criterion for statistical significance was set at p<.05.
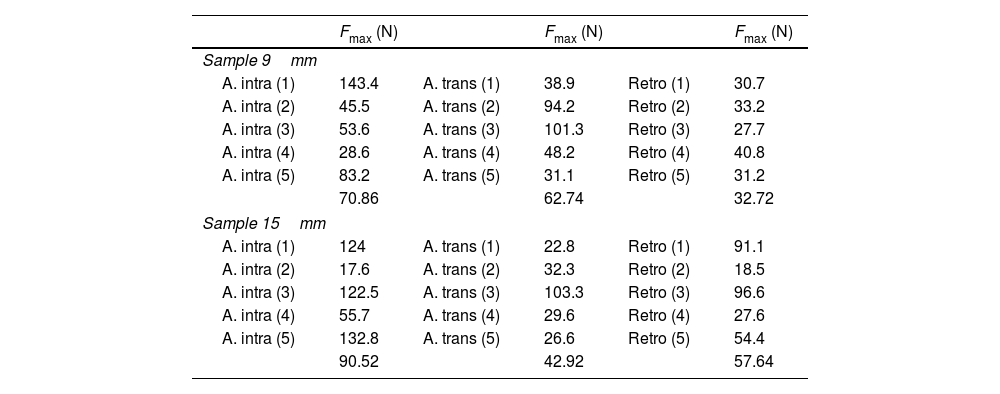
ResultsThis biomechanical study evaluated the resistance of the PF fracture model to 3 P bending strain (Table 1). For osteotomies at 9mm from the MCP joint, the anterograde IMHCS technique (both intra-articular and trans-articular technique, 70.86N and 62.74N, respectively) showed greater resistance than the retrograde technique (32.72N) (p=.002). Between the two antegrade techniques, the intra-articular technique (70.86N) withstood higher 3 P bending strain than the trans-articular technique (62.74N), in the 9mm group (p>.05). In contrast, the retrograde IMHCS technique was more stable than the antegrade in fractures at 15mm from the MCP joint (90.52N retrograde vs. 57.64N trans-articular vs. 42.92N intra-articular (p=.20) (Fig. 5).
Results obtained after application of deforming force at 3 points.
| Fmax (N) | Fmax (N) | Fmax (N) | |||
|---|---|---|---|---|---|
| Sample 9mm | |||||
| A. intra (1) | 143.4 | A. trans (1) | 38.9 | Retro (1) | 30.7 |
| A. intra (2) | 45.5 | A. trans (2) | 94.2 | Retro (2) | 33.2 |
| A. intra (3) | 53.6 | A. trans (3) | 101.3 | Retro (3) | 27.7 |
| A. intra (4) | 28.6 | A. trans (4) | 48.2 | Retro (4) | 40.8 |
| A. intra (5) | 83.2 | A. trans (5) | 31.1 | Retro (5) | 31.2 |
| 70.86 | 62.74 | 32.72 | |||
| Sample 15mm | |||||
| A. intra (1) | 124 | A. trans (1) | 22.8 | Retro (1) | 91.1 |
| A. intra (2) | 17.6 | A. trans (2) | 32.3 | Retro (2) | 18.5 |
| A. intra (3) | 122.5 | A. trans (3) | 103.3 | Retro (3) | 96.6 |
| A. intra (4) | 55.7 | A. trans (4) | 29.6 | Retro (4) | 27.6 |
| A. intra (5) | 132.8 | A. trans (5) | 26.6 | Retro (5) | 54.4 |
| 90.52 | 42.92 | 57.64 | |||
Fmax: maximum force; N: Newtons.
In the biomechanical study presented, fixation with an anterograde IMHCS in proximal P1 fractures proved more stable than with a retrograde IMHCS. In contrast, retrograde IMHCS fixation has been shown to be stronger in more distal P1 fractures.
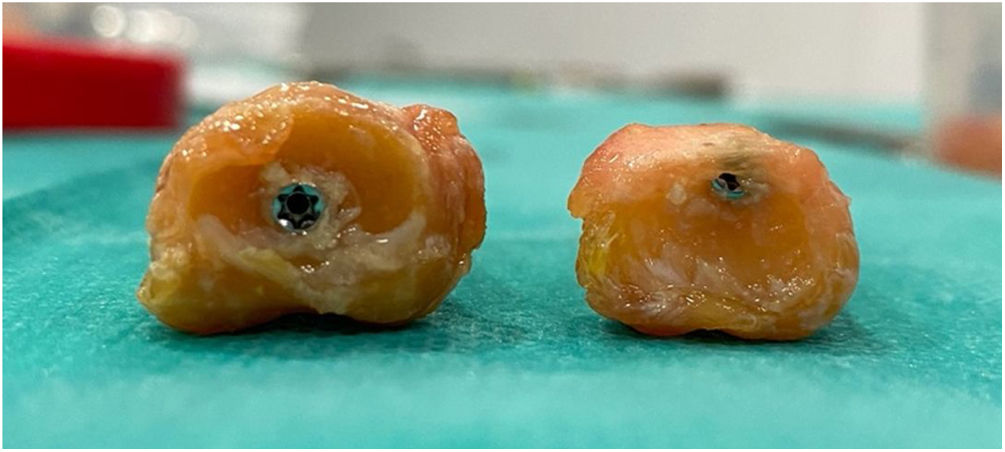
Various fixation methods have been described for transverse or short oblique P1 fractures.13–15 Optimal treatment should provide sufficient stability to enable early rehabilitation, with minimal soft tissue damage and a low rate of osteosynthesis material removal. Techniques using IMHCS have been shown to offer plate-like stability while avoiding soft tissue damage, and therefore potential postoperative stiffness is also reduced.7,8 Three IMHCS techniques have been described: antegrade intra-articular, antegrade trans-articular, and retrograde. With the retrograde IMHCS technique, despite damage to the cartilage of the phalangeal head (13%–18% for 2.5mm screws, 19%–25% for 3.0mm screws15) and the extensor apparatus during screw implantation, it has been reported that the percentage of joint surface affected is low, and would have little clinical impact.15 Anterograde fixation has the advantage that it avoids damage to the central band of the extensor apparatus and causes less damage to the articular surface during implantation6; 4.6% damage has been reported with the use of 2.2mm screws and 8.5% with 3.0mm screws.6 Of the anterograde techniques, the intra-articular technique avoids injury to the metacarpal head and halves the damage to the cartilage at the base of the P1 compared to the transarticular technique,6 but this is not always possible as limited subluxation of the MCP joint may not allow screw implantation. In these cases, especially in the index and middle fingers, the transarticular technique would be the alternative.
Aware of the advantages and disadvantages of the three methods of fixation with IMHCS, we wanted to investigate whether the stability of the construct changed depending on the technique chosen and the level of the fracture. Some authors have performed biomechanical studies finding statistical equivalence between intra-articular IMHCS techniques and plate-screw fixation in short oblique fractures of the P1.8 However, to our knowledge, there are no biomechanical studies that evaluate and compare the stability of fixation with the different IMHCS techniques in this type of fracture. We found that when the fracture was located closer to the MCP joint, the antegrade technique offered greater stability than the retrograde technique (66.74±38.86N vs. 32.72±4.92N, respectively), with no differences between the two antegrade techniques (70.86±45.11 vs. 62.74±32.62). On the other hand, when the fracture was located more distally, the construct with retrograde IMHCS was stronger (90.52±51.13N vs. 50.28±34.79N, respectively). Of note about these findings is that, although some methods offered less stability than others, in all groups the resistance was greater than 25N, which has been defined as the force experienced by the P1 in daily activities.16
Some caution is required in interpreting our results, given the inherent limitations of cadaveric studies. We only reproduced transverse fractures, which may not adequately represent a clinical scenario, as these types of fractures normally have some degree of obliquity. Nevertheless, the level at which we performed the osteotomy was at a constant distance to avoid the variability that this could produce in our results. We used the same screw size in all cases, unlike in clinical practice, where the screw size is individualised according to the phalanx and fracture. In our study we only assessed the resistance to extension forces, which, despite being the most common deforming forces in transverse and short oblique fractures of the P1, does not include other deforming forces such as rotational forces, to which this type of fracture may be exposed in the postoperative period.
Our findings have shown that anterograde IMHCS fixation of a transverse proximal P1 fracture in a cadaveric model offers greater stability than retrograde IMHCS, while this technique offers greater stability when the osteotomy is placed more distally. However, combining our results with previous biomechanical studies, both antegrade and retrograde IMHCS techniques offer sufficient postoperative stability for activities of daily living.
Level of evidenceLevel of evidence IV.
FundingThe present paper was funded by the Sociedad Española de Cirugía Ortopédica y Traumatología: Proyectos de Iniciación a la Investigación Fundación SECOT (Spanish Society of Orthopaedic Surgery and Traumatology: SECOT Foundation Research Initiation Projects).
Conflict of interestsThe authors have no conflict of interests to declare.