To carry out a review of degenerative subscapularis ruptures (SSC) after their arthroscopic repair and to evaluate whether the results are comparable in terms of pain and function to those of younger patients with traumatic ruptures.
MethodsThe data of 80 SSC tears of the 660 rotator cuff tears operated on by the same team of surgeons from June 2008 to June 2018 were retrospectively reviewed. The clinical data of the surgical indications were collected: age, gender, laterality, intervention delay, associated pathologies, location of pain, value of the Visual Analogue Scale (VAS) and the Constant–Murley test (CMT); surgical data were also collected: type and size of lesion, associated biceps injury and associated surgical procedure, coracoid stenosis and associated surgical procedure, number and type of anchors used. A statistical study was performed with multiple linear regression test, parametric tests (Student's t or ANOVA) and non-parametric tests.
ResultsOf 80 patients, 36 were women (45%) and 44, men (55%); mean age 61 years (range 47–81); mean delay of surgery 3.5 months (range 1–6); right shoulder affected in 46 cases (57.5%), left in 34 (42.5%); 22 (27.5%) were isolated lesions, 58 (72.5%) were associated with supraspinatus rupture (SE). The mean improvement was 5.0 points in terms of the VAS and 39.9 points on average in the CMT. New breakage rate, 1.25%. Adverse factors: size of the tear, delay in intervention, women. Patients with type I-B rupture have a better overall result in the CMT than types I-A and III. The longer the delay, the worse results are observed, both for the VAS and the CMT. Women present worse and statistically significant results both in the VAS (p 0.00) and in the CMT (p 0.01).
ConclusionsExcellent and good results have been obtained in this group of patients, but there are adverse factors such as the size of the tear, the duration of the symptoms and the association of other pathologies, especially in women.
Realizar una revisión de roturas del subescapular (SBE) de origen degenerativo tras su reparación por artroscopia y evaluar si los resultados son equiparables en términos de dolor y función a los de pacientes más jóvenes con roturas traumáticas.
Material y métodoSe han revisado de forma retrospectiva los datos de 80 roturas de SBE de las 660 roturas de manguito rotador intervenidas por el mismo equipo de cirujanos desde junio del 2008 hasta junio del 2018. Se recogieron los datos clínicos de los pacientes intervenidos: edad, género, lateralidad, demora de intervención, patologías asociadas, localización del dolor, valor de la escala visual analógica (EVA) y del test de Constant-Murley (TCM); se han recogido también los datos quirúrgicos: tipo y tamaño de lesión, lesión asociada del bíceps y gesto quirúrgico asociado, estenosis coracoidea y gesto quirúrgico asociado y número y tipo de anclajes empleados. Se realizó estudio estadístico con prueba de regresión lineal múltiple, pruebas paramétricas (t de Student o ANOVA) y pruebas no paramétricas.
ResultadosDe 80 pacientes, 36 fueron mujeres (45%) y 44, hombres (55%); media de edad de 61 años (rango 47 a 81); demora media de la cirugía de 3,5 meses (rango 1 a 6); hombro derecho afectado en 46 casos (57,5%), el izquierdo en 34 (42,5%); 22 (27,5%) fueron lesiones aisladas, 58 (72,5%), asociadas a rotura del supraespinoso (SPE). La mejoría media fue de 5,0 puntos en términos de la EVA y de 39,9 puntos de media en el TCM. Índice de nueva rotura, 1,25%. Factores adversos: tamaño de la rotura, demora de intervención, mujeres. Los pacientes con rotura tipo I-B tienen mejor resultado total en el TCM que los tipos I-A y III. A mayor demora se observan peores resultados, tanto de la EVA como del TCM. Las mujeres presentan resultados peores y estadísticamente significativos tanto en la EVA (p=0,00) como en el TCM (p=0,01).
ConclusionesSe han obtenido excelentes y buenos resultados en este grupo de pacientes con patología degenerativa del SBE, de forma equiparable a las series con casos traumáticos. Existen factores adversos, como el tamaño de la rotura, la demora de la cirugía y la asociación de otras patologías, especialmente en mujeres.
Subscapularis (SSC) rupture results in an alteration of the balance of the pairs of forces acting on the shoulder stabilising it in the transverse plane. This results in a tendency for the humeral head to migrate superiorly during movement, the greater the extent of the injury. Repair of the SSC is therefore essential to restore this balance.1 Injury can occur:2–4 (1) from fall trauma with the arm extended and rotated outwards, or from forces acting in hyperextension; (2) in association with anterior dislocation of the shoulder; or (3) associated with degenerative processes in work or sporting activities with the arm at or above the shoulder.5
Classically, it has been considered difficult to diagnose SSC injuries, especially because of the frequency of partial or incomplete lesions. These incomplete lesions may go unnoticed on nuclear magnetic resonance imaging (NMR) examination. They have therefore been described as “hidden lesions” or difficult to diagnose.6–8 This difficulty in diagnosis, together with the technical complexity of arthroscopic repair, has delayed a reliable approach to these lesions, and although there are previous descriptions, it was not until 1991 that the first results of surgical treatment were reported.2,3 The first arthroscopic results were not published before 2002.1,8–10 The classification of these lesions and their frequent association with bicipital groove injuries were also not described until recently.6,8,11,12 Progress in the diagnosis and treatment of these lesions has been aided by the description of the reliability of the different clinical examination tests,13 the description of specific signs on NMR imaging studies14–16 and the consolidation of surgical techniques for shoulder arthroscopy.1,7,10
Most of the studies dealing with SSC tears indicate that, in terms of aetiology, the percentage of injuries caused by trauma is between 40% and 80% and that the association of tears between the supraspinatus (SPE) and the SSC is 18% of all rotator cuff tears.17,18 It has also been pointed out that isolated subscapularis tears, which most frequently occur in young patients under 40 years of age and are associated with trauma, constitute a different entity from those of older people, associated with a mainly degenerative aetiology.19
The aim of this study is to review the results of cases of SSC rupture after arthroscopic repair and to assess whether they are comparable in terms of pain and function to those of series of younger patients with traumatic ruptures. We hypothesise that excellent and good results can be obtained in these patients, but that adverse factors may influence them.
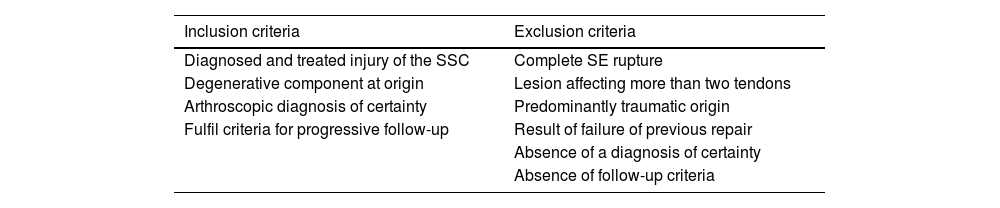
Material and methodsData was collected from 80 SSC ruptures (79 cases) selected from among 660 ruptures of rotator cuff operated on by the same surgical team from June 2008 to June 2018. Out of these cases in 280 (40%) an isolated lesion or SSC-associated lesions was diagnosed but only 80 lesions met with the inclusion criteria (Table 1).
Description of the inclusion-exclusion criteria.
| Inclusion criteria | Exclusion criteria |
|---|---|
| Diagnosed and treated injury of the SSC | Complete SE rupture |
| Degenerative component at origin | Lesion affecting more than two tendons |
| Arthroscopic diagnosis of certainty | Predominantly traumatic origin |
| Fulfil criteria for progressive follow-up | Result of failure of previous repair |
| Absence of a diagnosis of certainty | |
| Absence of follow-up criteria |
Inclusion criteria were: cases where a reconstruction of the SSC tendon lesión was made; they were of a degenerative nature and met with the arthroscopic diagnostic and follow-up care criteria. Exclusion criteria were: all cases where the supraspinatus tear was complete; the lesion affected more than two tendons; was of predominantly traumatic origin; were the result of a previous failure to repair; did not meet with the diagnostic criteria as the lesión was not well described during arthroscopy, or did not meet with the criteria for follow-up care.
In the database created for the study the following variables were included: type of rupture; age; sex; affected side; production mechanism; delay to surgery; the presence of other pathologies and the number of anchors used in repair. The study was approved by the Ethical Research Committee of the Quirón-Salud Hospital Group, with register code 2020/124-COT-PGQ.
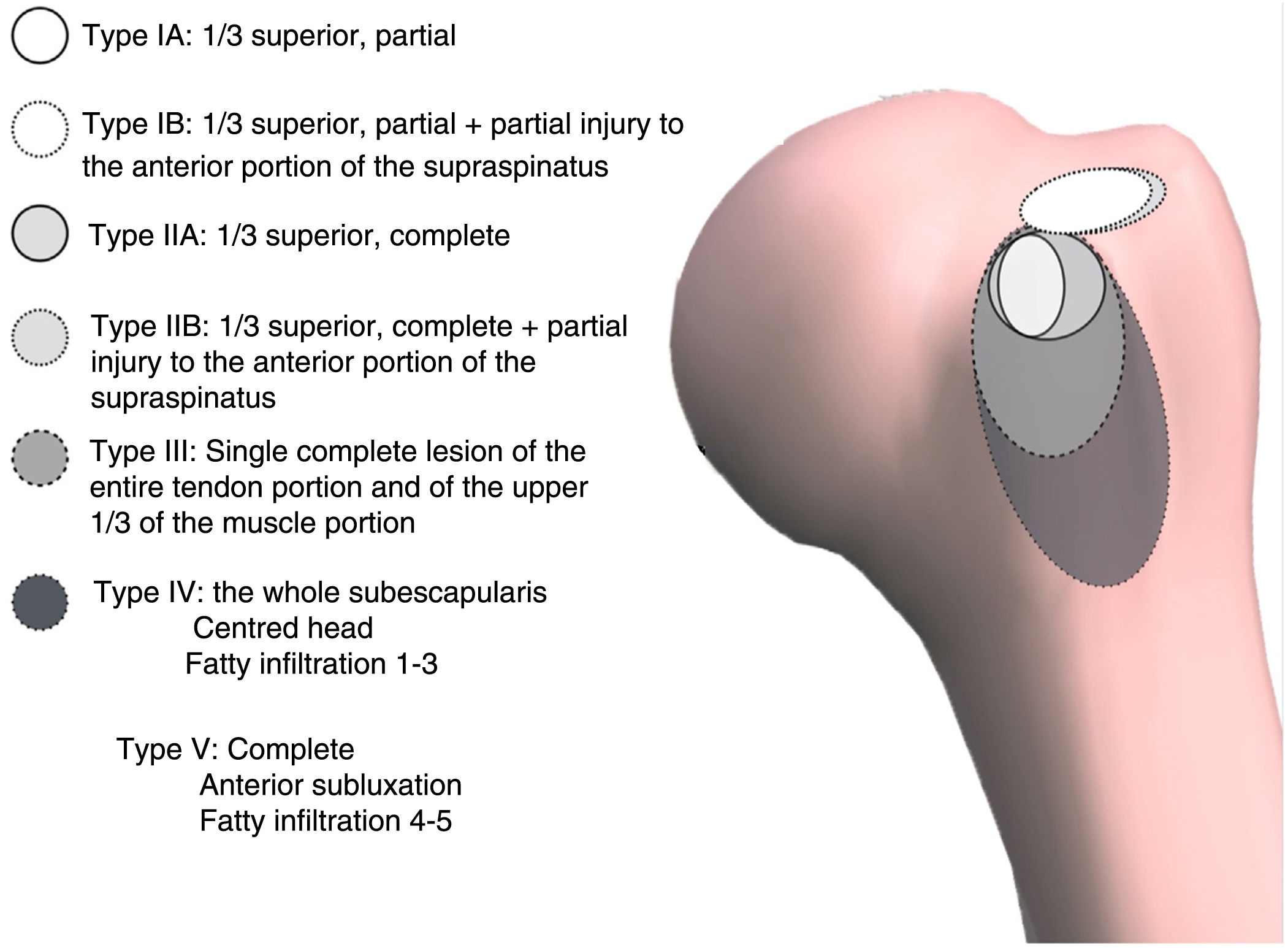
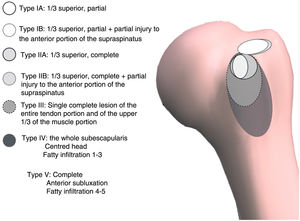
In this study, we have used the classification of the French school which, with its 5 types, takes into account the anatomical aspects related to the repair of lesions.11,12 We subclassify the frequent association of type I and type II lesions with partial full-thickness lesions of the most anterior portion of the SSC as types I-B and II-B (Fig. 1). In these, the long portion of the biceps (LPB) is involved in one way or another in almost all cases.20,21
Medical records contained significant data including: location of pain, presence of nocturnal pain, time of delay to surgery, mechanism of production, presence of other joint pathology, sports and work activity. The lift-off test, Napoleon's test and belly-press test were used together as recommended13 for diagnosis in the consultation room. Provocation tests were also performed to assess possible lesion of the LPB.22,23 To diagnose possible involvement of the coracohumeral space, the described manoeuvre of pain provocation was performed on the anterior aspect of the shoulder by means of a combined movement of antepulsion, internal rotation and adduction.23 Patients were assessed using the visual analogue scale (VAS) and the Constant–Murley test (CMT), validated in a previous study24 and performed preoperatively, 6 months after surgery and at 1 and 2 years.
In addition to undertaking the radiographic study with the three most usual projections (AP, axillary oblique and L scapular Y projection), the diagnosis of the lesion was completed by NMR study and the dimension of the coracohumeral space was assessed in the axial projection of the same NMR study.25 The NMR study was also used to assess signs of muscle atrophy and fatty infiltration.26
The cases that presented a traumatic component as a trigger for the symptomatology, (fall by hikers) were considered to be of low intensity and not decisive. The existence of a history of previous pain, the performance of an overuse activity (work or sport) or, especially, the presence of findings of a degenerative nature and the absence of acute signs in the NMR study also contributed to this.
Surgical procedureAll interventions were arthroscopic, performed by the same surgical team, who were highly experienced in arthroscopic surgery. The patients were operated on in lateral decubitus position under combined general and interscalene block anaesthesia. The posterior lever arm manoeuvre described by Burkhart,1,8 was used to improve the anterior access space to the lesion. The lesion is best explored by initially debriding the rotator interval, as described by Lafosse11; this allows better assessment of the frequent injury to the walls of the LPB groove, the stability of the LPB and the size of the SSC and SE tear.
Small tears are repaired from the glenohumeral space using a posterior view portal and an anterosuperior portal. These tears were repaired using a single anchor. In tears with associated SPE injury, this was completed from the subacromial space using a third anterolateral portal and the use of one to three anchors, depending on size.27 Type III ruptures were sutured from the subacromial space and required a fourth anteroinferior portal to allow better release of the retracted tendon, as described.9–12 These ruptures required the use of two to four anchors in a “double row” arrangement.
Postoperative protocolPostoperative immobilisation was usually maintained for 4–6 weeks, allowing pendulum-type exercises, active elbow flexion–extension, active forearm pronation and active hand and wrist mobility during this time. Active supination was allowed from 4 weeks in patients with biceps tenodesis. Rotations were started at 8 weeks and muscle strengthening at 9–12 weeks after surgery. Sports activities such as racquetball or swimming were not allowed before 6 months or, in general, until a good functional and muscular balance was achieved.
Statistical studySPSS v.22 was used for statistical analysis. Pain intensity and function were considered as primary outcome variables. Pain intensity was measured by 10cm VAS with the extremes marked as “no pain” and “greatest pain imaginable”, with no marks in between. Function was measured using the validated CMT24, both in global score and in each of its four subscales: pain, activities of daily living, mobility and strength. These are considered secondary study variables: the type of rupture (expressed in grades I-A, I-B, II-A, I-B, II-B and III), gender (male, female), the trigger of the pathology (twisting, overuse, occupational, gradual), the delay from surgery to the time of intervention (expressed in months), the number of anchors used in the intervention, the type of action performed on the LPB (no treatment; tendon absent; tenotomy; tenodesis either to support reconstruction, by anchors, or by screw), the presence of aggravating factors (other polyarticular inflammatory pathology) and the percentage of new symptomatic ruptures.
For quantitative type variables data was analysed to see whether they followed a normal distribution using the Kolmogorov–Smirnov test. To analyse the influence of quantitative (pain and delay to surgery) the multiple lineal regression test was used in the outcomes, and in the qualitative type variables parametric tests were used (Student's t-test for independent samples or ANOVA with Bonferroni correction) if values followed a normal distribution and non parametric tests (Mann–Whitney U test or Kuskal–Wallis) otherwise. The significance level was set at p<.05.
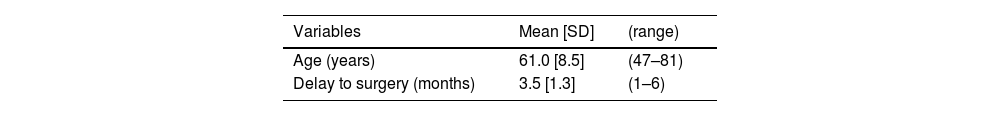
ResultsThe sample comprised 35 women and one of them was operated on in both shoulders during the study period. There were therefore 36 cases in women (45%) and 44 in men (55%), with a mean age at the time of surgery of 61 years (range 47–81) and a mean delay to surgery of 3.5 months, from the moment when surgery was indicated (range 1–6). The right shoulder was affected in 46 cases (57.5%) and the left in 34 (42.5%). The characteristic location of pain was mostly in the anterior side of the shoulder and radiated down the anterior side of the arm following the path of the biceps to the elbow flexor. Only in cases with major ruptures of types II-B and III were subscapularis exploration tests more evident. The clinical-demographic data of the sample are presented in Table 2.
Clinical/demographic sample variables.
| Variables | Mean [SD] | (range) |
|---|---|---|
| Age (years) | 61.0 [8.5] | (47–81) |
| Delay to surgery (months) | 3.5 [1.3] | (1–6) |
| Variables | n | (%) |
|---|---|---|
| Type of rupture | ||
| I-A | 10 | (12.5) |
| II-A | 7 | (8.8) |
| III | 5 | (6.3) |
| I-B | 23 | (28.7) |
| II-B | 35 | (43.8) |
| Gender | ||
| Man | 44 | (55) |
| Woman | 36 | (45) |
| Origin of the pathology | ||
| Sport (hikers’ fall) | 9 | (11.3) |
| Occupational (overuse) | 11 | (13.8) |
| repeated twisting movements | 7 | (8.8) |
| Gradual | 53 | (66.3) |
| Laterality | ||
| Right | 46 | (57.5) |
| Left | 34 | (42.5) |
| Number of anchorages | ||
| 1 | 17 | (21.3) |
| 2 | 27 | (33.8) |
| 3 | 28 | (35.0) |
| 4 | 8 | (10.0) |
| Type of action on PLB | ||
| No treatment | 10 | (12.5) |
| SLAP reinsertion | 2 | (2.5) |
| Absent | 5 | (6.3) |
| Tenotomy | 23 | (28.7) |
| Anchor tenodesis | 8 | (10.0) |
| Screw tenodesis | 5 | (6.3) |
| reconstruction support tenodesis | 27 | (33.8) |
| Other aggravating factors | ||
| Previous DSA | 4 | (5.0) |
| Other poliarticular inflammatory pathology | 15 | (18.8) |
| New rupture | 1 | (1.3) |
The diagnosis of certainty of the type of lesion was established in all cases after arthroscopic examination. Thus, the distribution of cases for each type of lesion was as follows (Table 2):
- 1)
Isolated SSC injury, 22 cases. Of these: 10 were type I, which we called I-A; 7, type II, which we called II-A; 5 more presented a type III rupture; during this period we did not treat any type IV injuries. Seventeen of the 22 presented with LPB injury and/or its groove.
- 2)
Twenty-three presented with a minor anterosuperior injury (type I SSC injury with incomplete anterior lesión of the SE, which we called type I-B. Twenty of the 23 presented with LPB injury.
- 3)
Thirty-five presented with anterosuperior injury, but with type II SSC tear together with incomplete anterior lesion of the SE, which we called type II-B. All of these cases presented with LPB injury.
In 17 of the 22 operated shoulders with partial isolated injury or injury proximal to the SSC (types I and II) repair of the whole lesion was achieved using one or two anchors, whilst in 5 cases with a complete rupture (type III) three or four anchors were required for SSC reconstruction. Type I-B and II-B lesions required two to three anchorages. The complementary surgical procedures (LPB, coracoidoplasty) are detailed in Table 2.
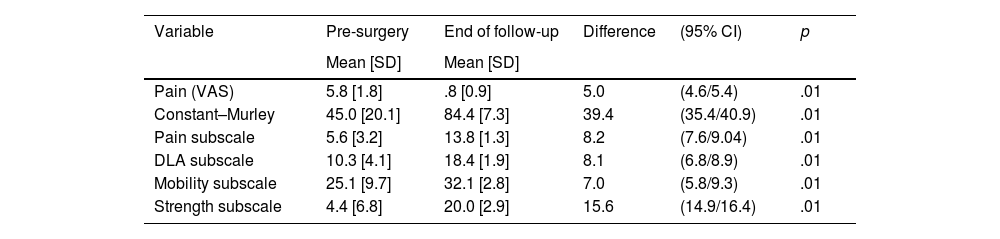
The mean preoperative VAS value in terms of pain was 5.8±1.8, and 45.0±20.1 in relation to the CMT, with mean subscale values of 5.6±3.2, 10.3±4.1, 25.1±9.7 and 4.4±6.8, respectively, for pain, activities of daily living (ADL), mobility and strength. At the end of the follow-up period all cases show a statistically significant improvement, with the mean pain expressed by the patients at the end of the follow-up period being 0.8±0.9 (range 0–4, mode 0, Mean 1). Mean functionality according to the CMT was 84.4 points, the subscale values being 13.8±1.3, 18.4±1.9, 32.1±2.8 and 20.0±2.9, respectively. The mean improvement was 5.0 points in terms of VAS and 39.9 points on average on the GCT. All these values are shown in Table 3.
Values of outcome variables.
| Variable | Pre-surgery | End of follow-up | Difference | (95% CI) | p |
|---|---|---|---|---|---|
| Mean [SD] | Mean [SD] | ||||
| Pain (VAS) | 5.8 [1.8] | .8 [0.9] | 5.0 | (4.6/5.4) | .01 |
| Constant–Murley | 45.0 [20.1] | 84.4 [7.3] | 39.4 | (35.4/40.9) | .01 |
| Pain subscale | 5.6 [3.2] | 13.8 [1.3] | 8.2 | (7.6/9.04) | .01 |
| DLA subscale | 10.3 [4.1] | 18.4 [1.9] | 8.1 | (6.8/8.9) | .01 |
| Mobility subscale | 25.1 [9.7] | 32.1 [2.8] | 7.0 | (5.8/9.3) | .01 |
| Strength subscale | 4.4 [6.8] | 20.0 [2.9] | 15.6 | (14.9/16.4) | .01 |
CI: confidence interval; DLA: daily life activities; SD: standard deviation.
The results of the multiple linear regression analysis are shown in Table 4. In relation to patient age, there is no statistical relationship with VAS (p=.99) and CMT (p=.60) results, while the time of delay in surgery does show a linear statistical relationship with VAS (p=.03) and CMT (p=.04) results. Worse results are observed in cases with longer waiting time. VAS ranged from .56 points on average for people who waited 1 month to 1.33 for people who waited 6 months. The CMT ranges from 88.9 points for people who waited 1 month to 80.7 for those who waited 6 months.
results in pain and function, according to initial sample characteristics.
| EVA | Constant–Murley | Mobility subscale | Strength subscale | |
|---|---|---|---|---|
| Mean | Mean | Mean | Mean | |
| Type of rupture | ||||
| I-A | 1.3 | 79.9 | 32.0 | 18.9 |
| II-A | .3 | 87.9 | 32.4 | 22.0 |
| III | .8 | 77.8 | 31.2 | 15.0 |
| I-B | .6 | 87.3 | 32.8 | 21.1 |
| II-B | .9 | 83.9 | 31.8 | 19.8 |
| Sig. | .10 | .01 | .73 | .00 |
| Gender | ||||
| Man | .5 | 86.2 | 32.7 | 20.5 |
| Woman | 1.2 | 82.1 | 31.4 | 19.4 |
| Sig. | .00 | .01 | .14 | .11 |
| Origin of pathology | ||||
| Sport | .6 | 88.9 | 33.8 | 22.2 |
| Occupational | .4 | 84.7 | 31.7 | 19.8 |
| Twisting | .9 | 83.9 | 31.7 | 20.4 |
| Gradual | .9 | 83.9 | 31.9 | 19.7 |
| Sig. | .26 | .19 | .32 | .22 |
| Laterality | ||||
| Right | .7 | 85.5 | 32.4 | 20.5 |
| Left | .9 | 82.9 | 31.7 | 19.3 |
| Sig. | .46 | .11 | .45 | .09 |
| Action on LPB tendon | ||||
| No treatment | 1.1 | 82.9 | 32.5 | 19.7 |
| SLAP reinsertion | 1.0 | 82.0 | 30.0 | 20.0 |
| Absent | .4 | 86.2 | 32.4 | 19.8 |
| Tenotomy | .7 | 85.2 | 32.8 | 19.9 |
| Anchor tenodesis | 1.1 | 83.0 | 31.4 | 19.8 |
| Screw tenodesis | .8 | 84.2 | 30.8 | 21.2 |
| reconstruction support tenodesis | .8 | 84.4 | 32.0 | 20.0 |
| Sig. | .72 | .96 | .36 | .90 |
| Other factors | ||||
| Previous DSA | 1.8 | 75.8 | 31.5 | 16.3 |
| Other polyarticular inflammatory pathology | 1.3 | 80.6 | 30.9 | 19.6 |
| Re-rupture | 4.0 | 50.0 | 20.0 | 10.0 |
| Sig. | .10 | .10 | .79 | .32 |
The type of rupture (Table 4) shows no statistically significant relationship with the VAS result (p=.10) but does show a statistically significant relationship with the total CMT result (p=.01). Post hoc ANOVA analysis applying Bonferroni correction shows statistically significant improvement of patients with type I-B rupture over patients with type I-A rupture (p=.05). With regard to gender, women presented worse and statistically significant results in both VAS (p=.00) and CMT (p=.01). The variables: origin of the pathology, laterality, action on the tendon of the long portion of the biceps and other factors recorded do not show a statistically significant relationship with either the VAS result (p from .10 to .87) or the CMT result (p from .10 to .96).
The mobility subscale of the CMT (Table 4) does not show statistically significant differences for any of the variables studied (p from .14 to .79), but the strength subscale does show statistically significant differences according to laterality (p=.09), with strength being lower on the left side, and according to type of rupture (p=.00), with strength being statistically lower in patients with type III rupture compared to patients with I-A (p=.04), II-A (p=.00), I-B (p=.00) and II-B (p=.00) ruptures. The influence of the treatment given to the tendon of the long portion of the biceps on the pain subscale of the CMT was also analysed, finding values ranging from 13.3 points (no treatment) to 14.4 points (absent), but with no statistically significant difference between these values (p=.67).
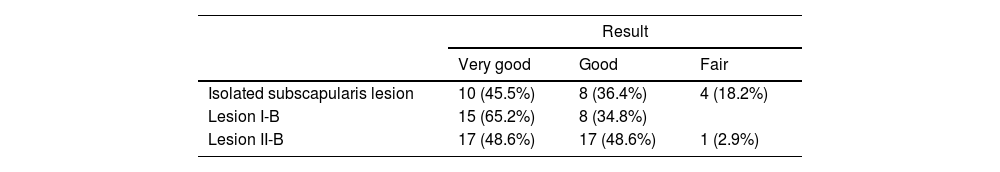
The results are considered overall as very good or excellent with an CMT score of 85 points or more; these patients were able to resume their work and leisure sports activity without significant impairment and without pain. The outcome was considered good with an CMT score of 75–85 points for loss of internal rotation behind the body or some residual pain; fair (70–75 points) for further loss of mobility or strength restricting daily function, and poor (below 70 points) leading to re-rupture with persistent painful symptoms and impairment of function. A very good or excellent result was obtained in 42 (52.5%), good in 33 patients (41.25%), fair in 4 (5.0%) and poor in one (1.25%) with 50 points for new rupture (due to clinical suspicion, confirmed by MRI) within the first 6 months of follow-up. The distribution of results by type of lesion is detailed in Table 5.
DiscussionThis study helps to show that good results can also be obtained with arthroscopic repair of subscapularis tears in patients with degenerative pathology, similar to the results obtained in young patients with trauma tears.4,17–19,28,29 We have also found that the results in this group are influenced by adverse factors, such as tear size, delay to surgery and association with other joint pathologies.
Regarding the group characteristics, this was a homogeneous series not only in terms of its degenerative nature but also in terms of size and the characteristics of the rupture, with no signs of fatty degeneration and/or significant muscle atrophy, which would also explain the low rate of new rupture. Thus, in this group in this group there is also an equal proportion of men and women, much higher for men in case series of traumatic origin.17–19 This has allowed certain valid conclusions to be drawn, such as the adverse influence of certain factors such as the size of the rupture, the delay to surgery in relation to the onset of symptoms and gender, with women obtaining worse results. Although the first two are predictable and coincide with those of other series4,17,18 we speculate that the poorer results obtained in the group of women could be due to the greater frequency of coexistence of other pathologies, such as polyarthritis.
It is also evident that despite good clinical outcomes, recovery of strength in these cases is lower than in trauma cases, as has been described.29 And that is particularly significant is the relationship between laterality (left arm) and lesion size, as shown in the results of the CMT strength subscale.
Based on the type of lesions found, we subclassify type I and II lesions as (Fig. 1): types I-A and II-A with single lesion of the SSC and types I-B and II-B incomplete lesions of the SSC associated with incomplete rupture of the most anterior portion of the SE, instead of basing it solely on the subscapularis rupture.30 These injuries also very frequently involve the long portion of the biceps (LPB) or its groove.20,21
Once again, the importance of detection of these incomplete SSC lesions is evident. Although their diagnosis has improved thanks to the higher reliability of the different clinical examination tests,13 description of specific NMR signs14–16 and arthroscopy,7,10 SSC lesions should continue being suspected in many cases, particularly those of a partial nature (longitudinal and transverse).31 We should therefore be meticulous in searching for them so that they stop being difficult to diagnose or being “hidden lesions”,32 as defined by Bennett6 and Lyons and Green.7
The findings reached in our series are in keeping with others which have been published. Thus, Gerber, in an already classical study from 1996,4 analysed the results from a series of 13 patients operated arthroscopically for an isolated SSC lesion. The mean age of these patients was 50, with a CMT result of 82. Two review articles were also of note: Mall17 reviewed 9 studies out of a total of 511 patients with a mean age of 54 years and the associated presence of the SE tear in 84% of them, obtaining a CMT value of 76.6. Lazarides19 also reviewed 12 studies with a total of 336 patients, all of whom were under 40 years of age, in which, above all, the return to sport in throwers was analysed, finding a loss of level or abandonment between 25% and 97%. Meshram18 analysed a series of 140 patients subdivided into a young group with an injury of traumatic origin with an average age of 59.3 and an older group with an injury of gradual origin and an average age of 62.5; they reached a result in the CMT of 69.9 (±5.2) and 68.2 (±5.4), respectively. In a study more similar to ours, but with a lower mean age (55.7), Gerhardt analyses a group of 68 patients with 69.1% of associated lesions of the SSC and SE and an CMT result of 79.9 (±9.1).28 Similar values are found in Jeong's series of 68 patients,29 with a SE lesion association of 86.8% and a CMT score of 75.7 (±16.6).
We only evaluated clinical data and we did not consider it necessary to undertake systematic imaging studies to assess the percentage of new ruptures, since these indices are known and are usually more significant when there are major type III and IV lesions with fatty infiltration above grade 2.18
The earlier detection of the pathology meant that, just as we did not have to treat grade IV ruptures during the study period, we did not treat cases with significant amyotrophy or fatty degeneration greater than grade 1 of the Goutalier classification.26 This means that the results are better and the rate of new rupture is lower (1.25%) than in other series that have treated larger ruptures and with a greater degree of muscle atrophy and/or fatty degeneration, such as 8.8% in the Jeong series18 or 33% in the Nove-Josserand.33 In this case, too, factors that worsen the prognosis are: the larger size of the rupture; the longer time elapsed between injury and repair, as well as female gender. However, age does not seem to be a determining factor in our series, as it is in Rhee's.34 Neither does the fact of repairing combined lesions as opposed to isolated lesions appear to be a determining factor in relation to the results of other series.35 The fact of performing surgery as soon as possible does seem to be a determining factor, as Gerber4 pointed out at the time and as Sppel36 points out in his review.
This study has some limitations. Thus, although it is based on prospective data collection, the study is really a retrospective review, so that the different consideration of some aspects could be a source of bias. However, as it is a descriptive study, it provides us with information to describe the type of patients with the best outcomes and to assess the incidence of certain prognostic factors. Although there are studies like this one, most of the works reviewed provide a more general overview without establishing a homogeneous group, as in this degenerative study.
ConclusionsExcellent and good results have been obtained in this group of patients with degenerative SSC pathology, comparable to series with trauma cases. There are adverse factors such as the size of the rupture, the delay to surgery and the association of other pathologies, especially in women.
Level of evidenceLevel of evidence IV, case series.
Ethical responsibilitiesProtection of humans and animalsThe authors declare that no experiments on humans or animals have been carried out for this research.
Confidentiality of dataThe authors declare that they have followed their centre's protocols on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the informed consent of the patients and/or subjects referred to in the article. This document is held by the corresponding author.
FundingThe authors declare that this article has not been partially or totally funded by any entity. Authors Ad.C., R.S. and R.C. are consultants who occasionally receive fees from Smith&Nephew.
Conflict of interestsThe authors have no conflict of interests to declare.