Shoulder calcific tendinopathy is a frequent cause of shoulder pain. Diagnosis is usually based on ultrasound (US) and/or X-ray. US is considered an inherently operator-dependent imaging modality and, interobserver variability has previously been described by experts in the musculoskeletal US. The main objective of this study is to assess the interobserver agreement for shoulder calcific tendinopathy attending to the size, type, and location of calcium analyzed in plain film and ultrasound among trained musculoskeletal radiologists.
Material and methodsFrom June 2018 to May 2019, we conducted a prospective study. Patients diagnosed with shoulder pain related to calcific tendinopathy were included. Two different experienced musculoskeletal radiologists evaluated independently the plain film and the US.
ResultsForty patients, with a mean age of 54.6 years, were included. Cohen's kappa coefficient of 0.721 and 0.761 was obtained for the type of calcium encountered in plain film and the US, respectively. The location of calcification obtained a coefficient of 0.927 and 0.760 in plain film and US, respectively. The size of the calcification presented an intraclass correlation coefficient (ICC) of 0.891 and 0.86 in plain film and US respectively. No statistically significant differences were found in either measurement.
ConclusionThis study shows very good interobserver reliability of type and size measurement (plain film and US) of shoulder calcifying tendinopathy in experienced musculoskeletal radiologists.
La tendinopatía calcificante de hombro es una causa frecuente de dolor de hombro. El diagnóstico suele basarse en la ecografía (US) y/o la radiografía. La ecografía se considera una modalidad de imagen inherentemente operador dependiente, y la discrepancia interobservador ha sido descrita previamente por expertos en ecografía musculoesquelética. El objetivo principal de este estudio es evaluar la concordancia interobservador para la tendinopatía calcificante del hombro atendiendo al tamaño, al tipo y a la localización del calcio analizado en la radiografía simple y la ecografía entre radiólogos musculoesqueléticos experimentados.
MetodologíaEntre junio de 2018 y mayo de 2019 se realizó un estudio prospectivo. Se incluyeron pacientes diagnosticados de tendinopatía calcificante de hombro sintomática. Dos radiólogos musculoesqueléticos experimentados evaluaron de forma independiente la radiografía simple y la ecografía.
ResultadosSe incluyeron 40 pacientes, con una edad media de 54,6 años. Se obtuvo un coeficiente kappa de Cohen de 0,721 y 0,761 para el tipo de calcificación encontrada en la radiografía simple y la ecografía, respectivamente. La localización de la calcificación obtuvo un coeficiente de 0,927 y 0,760 en la radiografía simple y la ecografía, respectivamente. El tamaño de la calcificación presentó un coeficiente de correlación intraclase (CCI) de 0,891 y 0,86 en la película simple y la ecografía, respectivamente. No se encontraron diferencias estadísticamente significativas.
ConclusionesLa concordancia interobservador en la medición del tipo y del tamaño de la calcificación en la tendinopatía calcificante de hombro entre radiólogos musculoesqueléticos experimentados es muy buena, tanto en la radiografía simple como en la ecografía.
Shoulder calcific tendinopathy is a frequent cause of shoulder pain. It is characterized by the deposit of hydroxyapatite crystals in one or more shoulder tendons.1 Louwerens et al. reported a prevalence of 7.8% in asymptomatic patients and 42.8% in symptomatic patients. If analyzed by age groups, individuals between 31 and 40 years old had an incidence of 19.5%.2 Women are more often affected in the 4th or 5th decade. About 10% have calcium deposits on both shoulders.3
Shoulder calcific tendinopathy can be treated percutaneously with ultrasound-guided needling or ESWT (extracorporeal shock wave therapy) if needed. The indication for these treatments is based on the type and size of calcium.4 But there are also others possible treatments such as arthroscopy surgery or open surgery.8
The cause of shoulder calcific tendinopathy is unknown, but it is well known the natural history of the disease is self-limiting. Regarding Uhthoff et al. there are 4 phases in shoulder calcific tendinopathy: precalcification, formation, rest, and reabsorption.1 In the reabsorption phase, the calcium deposition can migrate into the subacromial bursa, intratendinous, into the humeral head (osseous migration), or exceptionally into the myotendinous junction.5 These stages are characterized by differences in size, shape, and appearance in imaging techniques.6
Diagnosis is usually based on the clinical history and imaging studies (ultrasound [US] and/or X-ray).3 Conservative management usually involves rest, physical therapy, and oral non-steroid anti-inflammatory drugs (NSAIDs) administration. Surgical management is gradually being superseded by new minimally invasive options such as extracorporeal shock wave therapy and ultrasound-guided percutaneous lavage.7,8
It is very important to differentiate types of calcifications with the US since this will determine the type of treatment and evolution of the patient.9 However, ultrasonography is considered an inherently operator-dependent imaging modality,10 and, interobserver variability has previously been described by experts in the musculoskeletal US.11
The main objective of this study is to assess the interobserver agreement for shoulder calcific tendinopathy attending to the size, type, and location of calcium analyzed in plain film and ultrasound among trained musculoskeletal radiologists.
MethodsAfter approval by the local ethics committee (EC123-19_FJD) and giving informed consent to every patient, an observational prospective study was conducted. Patients were collected between June 2018 and May 2019.
Inclusion criteria were: patients diagnosed with calcifying tendonitis of the shoulder. Exclusion criteria were: previous ipsilateral shoulder surgery, patients<18 years, and, patients who refused to participate in the study. All included patients met the inclusion and exclusion criteria.
Two experienced musculoskeletal radiologists (at least 8 years of experience) performed a shoulder US on each patient and reported the X-ray (standardized anteroposterior and trans-scapular X-ray). They determined the location, size, and type of calcium in both diagnostic tests. Each plain radiography was independently reviewed by the two radiologists. The following features were rated: location, calcium size, and type according to Gartner and Heyer's classification (Fig. 1A–C).6
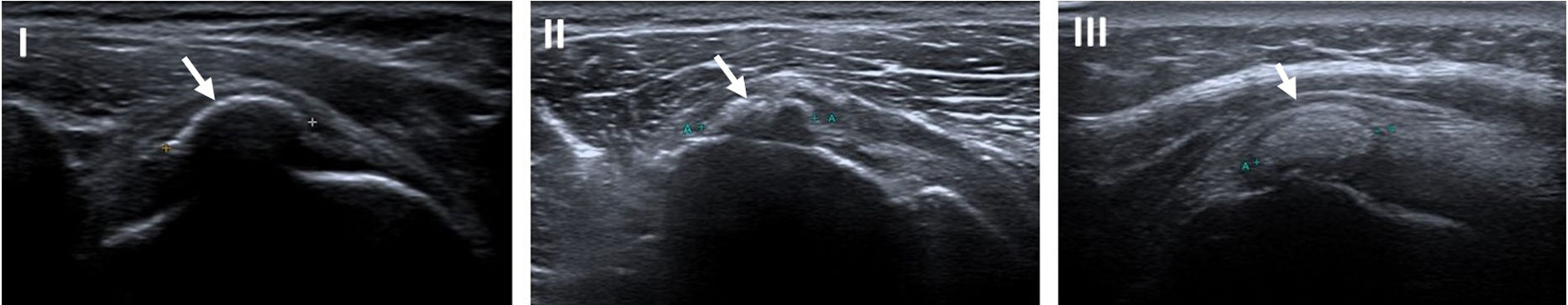
Gartner and Heyer classification.6 (A) Type I: well-circumscribed, dense calcification, formative phase. (B) Type II: soft contour/dense or sharp/transparent. (C) Type III: translucent and cloudy appearance without clear circumscription, resorptive phase.
Shoulder US was also performed by the two radiologists independently using a Toshiba ultrasound. Sonography was performed the same day using a 9–15MHz linear-array transducer and included a complete examination of the shoulder. While the first observer performed the examination, the second waited in a different room. Each observer independently scanned the calcium and rated the following US features: side (right/left), tendon (subscapular, supraspinatus or infraspinatus), size (each observer selected the image that presumably showed the largest diameter) and, calcification type according to a Bianchi and Martinoli classification (Types I, II and III) (Fig. 2).12 If a patient showed more than one calcification, an evaluation was made for each one of them. Data were collected and analyzed on Microsoft Excel, both observers wrote down their results in two independent Excel worksheets.
Bianchi and Martinoli classification. Type I: calcifications appear as hyperechoic foci with a well-defined acoustic shadowing due to their substantial quantitative of calcium; Type II: calcification appears as hyperechoic foci with a mild acoustic shadow due to the reduced amount of calcium; Type III: calcification appears almost isoechoic with the tendon, without an acoustic shadow and often they are difficult to diagnose.
Interobserver agreement on nominal categorical ratings (location and calcium type) was evaluated using Cohen's kappa statistic. Values smaller than 0.20 are considered indicative of slight agreement; 0.21–0.40, fair agreement; 0.41–0.60, moderate agreement; 0.61–0.80, substantial agreement; and 0.81–1.00, near-perfect agreement.
Interobserver agreement on calcium size was evaluated using the intraclass correlation coefficient (ICC). The following criteria were used to determine interobserver reliability: very low (<0.20), low (0.21–0.40), moderate (0.41–0.60), good (0.61–0.80), and excellent (0.81–1.00).
For all statistics, 95% confidence intervals (CI) were also calculated. Data analyses were performed using the SPSS statistical package (IBM Corp. Released 2017. IBM SPSS Statistics for Windows, Version 25.0, Armonk, NY, USA).
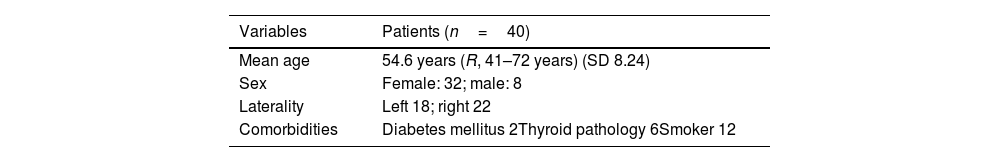
ResultsForty patients (8 women/32 men), with a mean age of 54.6 years (R, 41–72 years), were included. The side affected most frequently was the right (22 patients). Regarding comorbidities, 6 patients suffered from thyroid diseases, 2 patients had diabetes mellitus and, 12 patients were smokers (Table 1). Cohen's kappa coefficient of 0.721 and 0.761 was obtained for the type of calcium encountered in plain film and the US, respectively. Location of calcification obtained a coefficient of 0.927 and 0.760 in plain film and US respectively. The size of the calcification ranged from 4.5mm to 18mm and, presented an ICC of 0.891 and 0.86 in plain film and US respectively. No statistically significant differences were found in either measurement.
DiscussionThe most important finding of this work is that we have found very good interobserver reliability of type and size measurement of shoulder calcifying tendinopathy (plain film and US) in experienced musculoskeletal radiologists.
In the available literature, some articles analyzed interobserver reliability on shoulder bursitis,10 subacromial structures,13 and, rotator cuff.14 However, at the time of publication, interobserver variability of shoulder calcific tendinopathy based on X-ray and US assessment of calcium type, location, and size has not previously measured.
Shoulder calcific tendinopathy can be treated percutaneously with ultrasound-guided needling or shock wave treatment if conservative treatment fails. For some authors, percutaneous treatment is based on the type and size of calcium and is not indicated when patients are asymptomatic, have small calcification less than 5mm or it has migrated into the bursal space.3 However, it is not clear if the location and initial type and size of the calcium would affect clinical results.15
Lowerens et al. concluded that interobserver radiographic classifications for calcific tendinitis of the rotator cuff are not reliable enough and would need more precise and simplified criteria to improve reliability.16 Ultrasound is a very useful technique in shoulder calcific tendinopathy evaluation, especially in those cases where calcium has started the reabsorption process and shows fragmentation at the plain film, which difficulties its identification.3 However, operator dependency is a well-known disadvantage of this technique.17 The resgistering measurements is widely spread in musculoskeletal radiology, but several publications question their reliability,1 especially when they determine different treatments.
Cohen's kappa is a useful measure of interobserver reliability. Where 0 represents the amount of agreement that can be expected from chance and 1 represents a perfect agreement between two tests. The results of the present study suggest that both techniques (X-ray and US) are reliable and the radiologist interobserver reliability ranged from moderate to almost perfect.
The results showed very good reliability on calcium's size measurement in both techniques in X-ray and US being somewhat minor in localization and type, although we also found a very good correlation. This is probably because calcium shows very well-defined margins with both techniques (high density at plain film and hyperechogenicity in the US, independent of their state of reabsorption). Although the location of calcium in the shoulder does not participate in therapeutic decisions, this study also shows that the degree of agreement on the affected tendon is very high in both techniques for experienced observers.
A limitation of this study is that there were no inexperienced observers. We nonetheless consider that experience is essential in ultrasound examination. Therefore we assume that the treatment's indication based on calcium's size, location, and type could be performed with a high grade of reliability between different observers.
ConclusionThis study shows very good interobserver reliability of type and size measurement (plain film and US) of shoulder calcifying tendinopathy in experienced musculoskeletal radiologists.
Level of evidenceLevel of evidence iii.
Institutional review board statementThe study was conducted according to the guidelines of the Declaration of Helsinki and approved by the local Ethics Committee (EC123-19_FJD).
Informed consent statementInformed consent was obtained from all subjects involved in the study.
FundingThis research received no external funding.
Conflicts of interestThe authors declare no conflict of interest.