Hip arthroplasty represents a significant advancement in the treatment of refractory chronic joint pain, improving quality of life and functionality. The objective of this study is to identify the risk factors associated with local and systemic complications in patients treated with total hip arthroplasty.
MethodsObservational, analytical, retrospective cohort study, which included 304 participants treated with total hip replacement. Comparison of variables between two groups was performed; 38 participants in the group with complications and 266 participants in the group without complications.
ResultsThe mean age in the complication group was 66 years (SD 18.7) and in the uncomplicated group it was 67.1 years (SD 15.1) (p 0.686). Female sex was observed in 73.3% of the group with complications and 65% in the group without complications (p 0.292). Risk factors were: hip fracture as an indication for arthroplasty RR 1.33 [95% CI 1.004; 1.775 p 0.047], coronary heart disease RR 1.31 [95% CI 1.067; 1.616 p 0.010] and surgical bleeding equal to or greater than 400 cc RR 1.11 [95% CI 1.012; 1.218 p 0.028].
ConclusionsThe risk factors for complications in total hip arthroplasty were: hip fracture as the indication for arthroplasty, coronary artery disease, and surgical bleeding equal to or greater than 400 cc.
La artroplastia de cadera es un gran avance para el tratamiento del dolor articular crónico refractario, que mejora la calidad de vida y la funcionalidad. El objetivo de este estudio es identificar los factores de riesgo asociados a complicaciones locales y sistémicas en pacientes tratados con artroplastia total de cadera.
MétodosEstudio observacional, analítico, de cohorte retrospectiva, que incluyó a 304 participantes tratados con reemplazo total de cadera. Se realizó la comparación de variables entre dos grupos: 38 participantes en el grupo de complicaciones y 266 participantes en el grupo sin complicaciones.
ResultadosLa media de edad en el grupo de complicación fue de 66 años (DE 18,7) y en el grupo sin complicaciones fue de 67,1 años (DE 15,1) (p=0,686). El sexo femenino se observó en el grupo de complicaciones en el 73,3%, y en el grupo sin complicaciones en el 65% (p=0,292). Los factores de riesgo fueron: fractura de cadera como indicación de la artroplastia RR 1,33 [IC 95% 1,004;1,775 p=0,047], enfermedad coronaria RR 1,31 [IC 95% 1,067;1,616 p=0,010] y sangrado quirúrgico igual o mayor a 400 cc RR 1,11 [IC 95% 1,012;1,218 p=0,028].
ConclusionesLos factores de riesgo para complicaciones en artroplastia total de cadera fueron: fractura de cadera como indicación de la artroplastia, enfermedad coronaria y sangrado quirúrgico igual o mayor a 400 cc.
Osteoarthrosis of the hip joint is a complex chronic disease characterised by degeneration of the articular cartilage and thickening of the subchondral bone. This condition impacts joint function, is painful, and adversely affects the patient's quality of life.1 Primary arthroplasty of the hip is the treatment of choice to address advanced osteoarthrosis of the hip, given that it improves function and provides effective pain relief.2,3 While it is a safe procedure, total hip replacement does not come without its complications and can entail associated infection, instability, and loosening or wear of the prosthesis, which, in some cases, may warrant revision surgery.2,4,5 With nearly 650,000 procedures performed each year in the United States and a projected increase by up to 70% in the number of surgeries by the year 2030, studying the potential complications and various interventions to minimise risk is of paramount importance.6,7 Sociodemographic factors, comorbidities, surgery-specific factors, as well as the use of certain medications have been found to correlate with the incidence of complications in total hip arthroplasty8; nevertheless, definitive conclusions regarding the factors associated with worse surgical outcomes have yet to be reached.9 This study seeks to identify the factors associated with worse surgical outcomes in total hip arthroplasty, in addition to identifying risk factors associated with complications in patients undergoing this type of surgery.
MethodsAfter the approval of the ethics and research committee of the Imbanaco Clinic (referral hospital in the city of Cali, Colombia) registered under CEI-000002-Protocol CEI-660, a retrospective observational cohort study was conducted; the sample size for cohort studies was calculated using the Epidat software programme, version 4.2 (Servicio de Epidemioloxía de la Dirección Xeral de Saúde Pública de la Consellería de Sanidade [Expidemiology Service of the Department of Health], Xunta de Galicia [the Regional Government of Galicia], with the support of the Pan American Health Organization [PAHO-WHO] and the CES University of Colombia). The parameters were: risk in those exposed 7%,10 95% confidence level, 80% power, application of Yates correction for a minimum sample size of 279 patients, non-probabilistic convenience sampling. The inclusion criteria consisted of patients aged 18 years or older, with a minimum follow-up of six months, treated with total hip arthroplasty by the Knee and Hip Joint Surgery Group between the years 2010 and 2022. The exclusion criteria included incomplete medical records and any other surgical treatment during the same operation time.
The database was recorded in the 2019 version of Excel® (Microsoft Corporation, Redmond, Washington, United States) and subsequently analysed using the SPSS® software package, version 28 (IBM, Armonk, New York, United States). The univariate analysis was carried out by means of descriptive statistics, determining absolute and relative frequencies in the categorical variables; for the numerical variables, measures of central tendency and dispersion were ascertained. The bivariate analysis to determine associations between the different categorical variables was performed using Pearson's χ2 test, which yielded the p value (significant <0.05) and the RR (relative risk) with its 95% confidence interval. Likewise, the multivariate analysis relied on the Poisson generalised linear regression model; the variables that displayed an association in the bivariate analysis and with a theoretical representative value were included in the model.
For the present study, the dependent variable was defined as the overall incidence of complications, defined as any local (superficial or deep infection of the surgical site, dislocation of the prosthesis, periprosthetic fracture, peripheral nerve injury, loosening of the prosthesis, and shortening of the limb) or systemic complication directly related to the postoperative period (severe anaemia requiring transfusion, death, pulmonary embolism, ventricular tachycardia, urinary tract infection, or pneumonia). The independent variables were: age 70 years or older, sex, arterial hypertension, diabetes mellitus, malnutrition, normal weight, overweight (BMI between 25 and 29.9), obesity (BMI ≥30), heart failure, coronary heart disease, cardiac arrhythmia, cerebrovascular disease, chronic kidney disease, chronic obstructive pulmonary disease (COPD), Parkinson's disease, hypothyroidism, rheumatoid arthritis, osteoporosis, Alzheimer's disease/dementia, anaemia, cancer, coxarthrosis, hip dysplasia, hip fracture, avascular necrosis, right lateral, posterolateral approach, anterolateral approach, total prosthesis, bipolar prosthesis, Exactech® prosthesis (Exactech, Inc., Gainesville, Florida, USA) (standard stem, uncemented), Johnson® prosthesis (DePuy Synthes, Warsaw, Indiana. Country: USA) (standard stem, uncemented), Link® prosthesis (Waldemar Link GmbH & Co. KG, Hamburg, Germany) (standard stem, uncemented) (standard stem, uncemented), Johnson® prosthesis (DePuy Synthes, Warsaw, Indiana. Country: USA) (standard stem, uncemented), Link® prosthesis (Waldemar Link GmbH & Co. KG, Hamburg, Germany) (standard stem, uncemented), Corin® prosthesis (Corin Group, Cirencester, Gloucestershire, United Kingdom) (standard stem, uncemented), Smith and Nephew® prosthesis (Smith & Nephew plc, London, United Kingdom) (standard stem, uncemented), Stryker® prosthesis (Stryker Corporation, Kalamazoo, Michigan, United States) (standard stem, uncemented), surgical time equal to or greater than 130min, intraoperative bleeding equal to or exceeding 130min, and thromboprophylaxis. All outcomes were assessed up to 12 months from the date of the surgical procedure.
Inclusion and exclusion criteria were used to control for selection bias; variables were collected from medical records without prior knowledge of which patients did or did not develop any complication, and a Poisson regression model was used to control for confounding bias.
ResultsThe institution's database included 310 patients; six were ruled out because they were miscoded and corresponded to knee joint replacements.
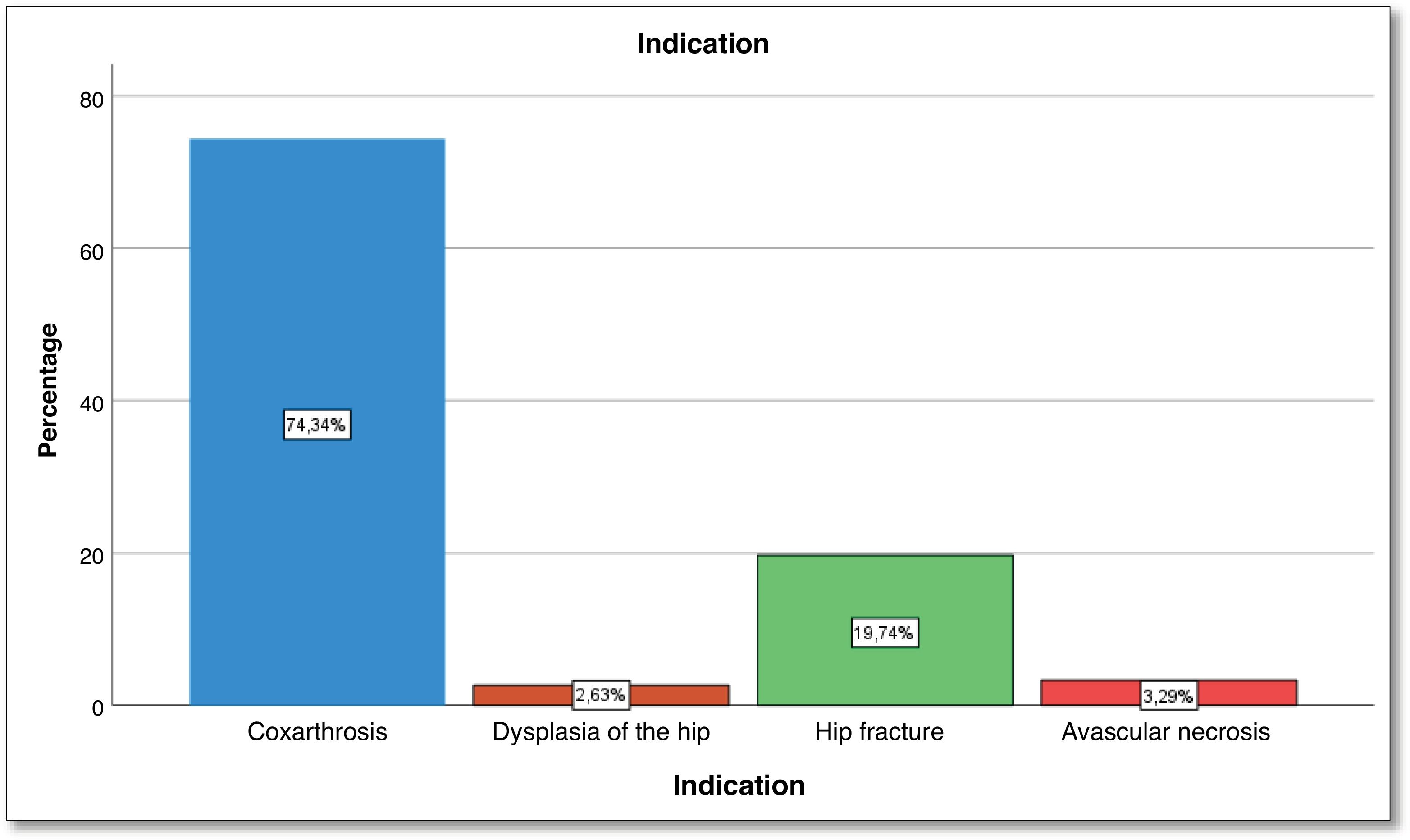
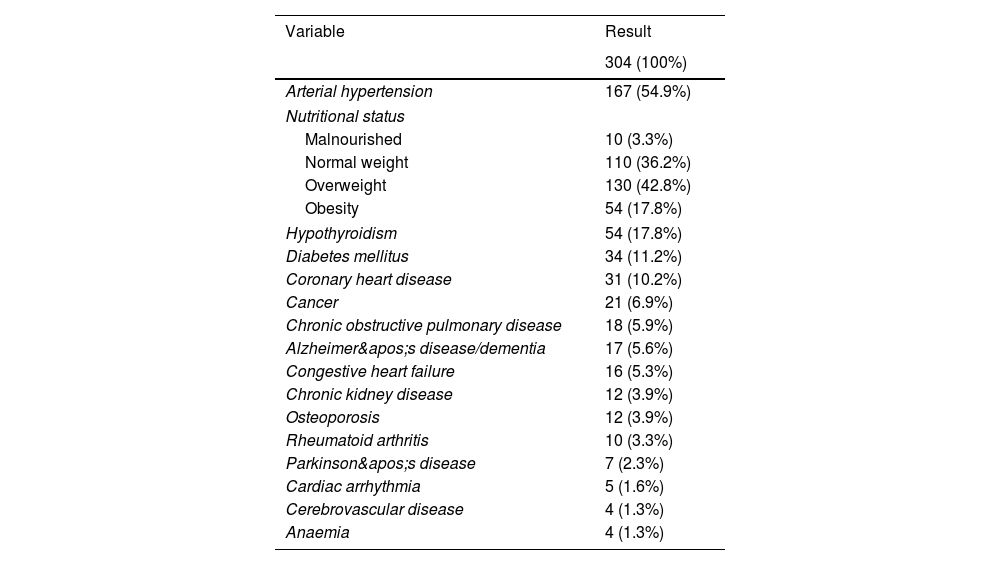
Univariate analysisThe total sample comprised 304 subjects, most of whom were female (66.1%). The youngest participant was 18 years old and the oldest one was 96 years old; the mean age was 67 years (SD 15.7 years). More than half (54.9%) had a history of arterial hypertension; 42.8% were overweight; 17.8% were obese; 17.8% had hypothyroidism; 11.2% had diabetes mellitus, and 10.2% had coronary heart disease (Table 1). The number one indication for total hip arthroplasty was coxarthrosis (74.3%), followed by hip fracture (19.7%), and avascular necrosis (3.2%) (Fig. 1). As for the characteristics of the surgery itself, the side most often treated was the right hip (54.9%); the most widely used approach was posterolateral (96.4%), followed by anterolateral (2.3%). The most extensively implanted prostheses were complete, accounting for 88.8%, and bipolar in 11.2% of the cases. The brands of implants were Exactech® 74.7%, Link® 14.5%, Johnson® 6.3%, Stryker® 2.3%, Corin® 1.6%, and others 0.7%. Of the people who underwent total hip arthroplasty, 97.7% received antithrombotic prophylaxis; the mean operative time was 137min (SD 64.4); the mean intraoperative bleeding was 375 cc (SD 193), and the mean number days of hospital stay was four (SD 4.7).
Clinical history of the study population.
| Variable | Result |
|---|---|
| 304 (100%) | |
| Arterial hypertension | 167 (54.9%) |
| Nutritional status | |
| Malnourished | 10 (3.3%) |
| Normal weight | 110 (36.2%) |
| Overweight | 130 (42.8%) |
| Obesity | 54 (17.8%) |
| Hypothyroidism | 54 (17.8%) |
| Diabetes mellitus | 34 (11.2%) |
| Coronary heart disease | 31 (10.2%) |
| Cancer | 21 (6.9%) |
| Chronic obstructive pulmonary disease | 18 (5.9%) |
| Alzheimer's disease/dementia | 17 (5.6%) |
| Congestive heart failure | 16 (5.3%) |
| Chronic kidney disease | 12 (3.9%) |
| Osteoporosis | 12 (3.9%) |
| Rheumatoid arthritis | 10 (3.3%) |
| Parkinson's disease | 7 (2.3%) |
| Cardiac arrhythmia | 5 (1.6%) |
| Cerebrovascular disease | 4 (1.3%) |
| Anaemia | 4 (1.3%) |
Source: Drafted by the authors.
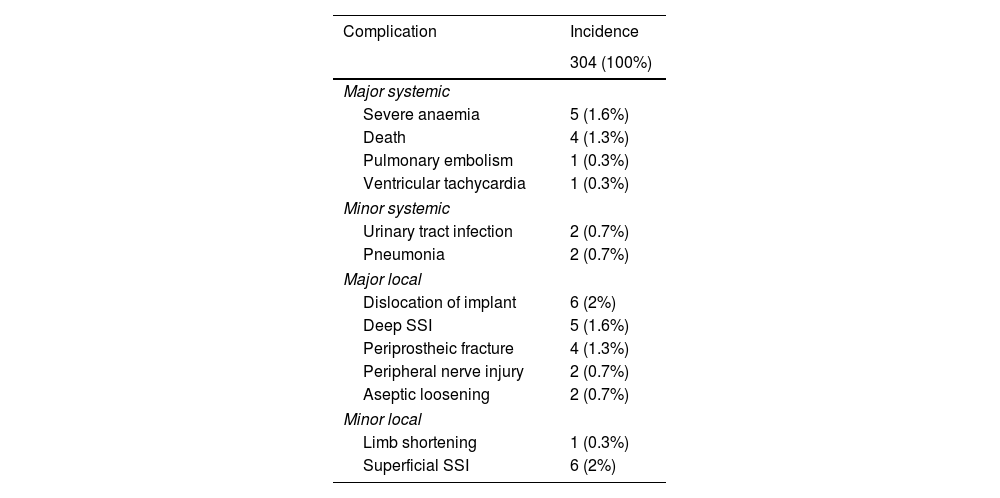
The overall incidence of complications was 12.5% (including all types of complications, regardless of the degree of severity). Each complication was categorised considering the four groups as put forth by Belmont et al.11 and on the basis of the grade of severity; i.e., major systemic (death, anaemia requiring transfusion, pulmonary thromboembolism [PTE], and ventricular tachycardia), minor systemic (pneumonia and urinary tract infection [UTI]), major local (periprosthetic fracture, prosthesis dislocation, deep surgical site infection, and peripheral nerve injury), and minor local (superficial surgical site infection and limb shortening). This yielded an incidence of major systemic complications of 3%, minor systemic complications of 1.3%, major local complications of 7.2%, and minor local complications of 2.3%.
Table 2 outlines the incidence rate of complications in detail. Both prosthesis dislocation and operative site infection were present with an incidence of 2%, followed by severe anaemia and deep operative site infection, each displaying an incidence of 1.6%.
Incidence of complications in total hip replacement surgery.
| Complication | Incidence |
|---|---|
| 304 (100%) | |
| Major systemic | |
| Severe anaemia | 5 (1.6%) |
| Death | 4 (1.3%) |
| Pulmonary embolism | 1 (0.3%) |
| Ventricular tachycardia | 1 (0.3%) |
| Minor systemic | |
| Urinary tract infection | 2 (0.7%) |
| Pneumonia | 2 (0.7%) |
| Major local | |
| Dislocation of implant | 6 (2%) |
| Deep SSI | 5 (1.6%) |
| Periprostheic fracture | 4 (1.3%) |
| Peripheral nerve injury | 2 (0.7%) |
| Aseptic loosening | 2 (0.7%) |
| Minor local | |
| Limb shortening | 1 (0.3%) |
| Superficial SSI | 6 (2%) |
SSI: surgical site infection.
Source: Drafted by the authors.
As for the need for revision surgery, 4.6% of the participants (14 of 304 patients) required revision. The reasons cited for revision were: dislocation of the prosthesis that could not be corrected by closed reduction in 35.7% of cases (5 of 14 subjects), deep infection of the operative site in 35.7% of patients (5 of 14 participants), aseptic loosening in 14.3% of cases (2 of 14 patients), and periprosthetic fracture in 14.3% of subjects (2 of 14 individuals).
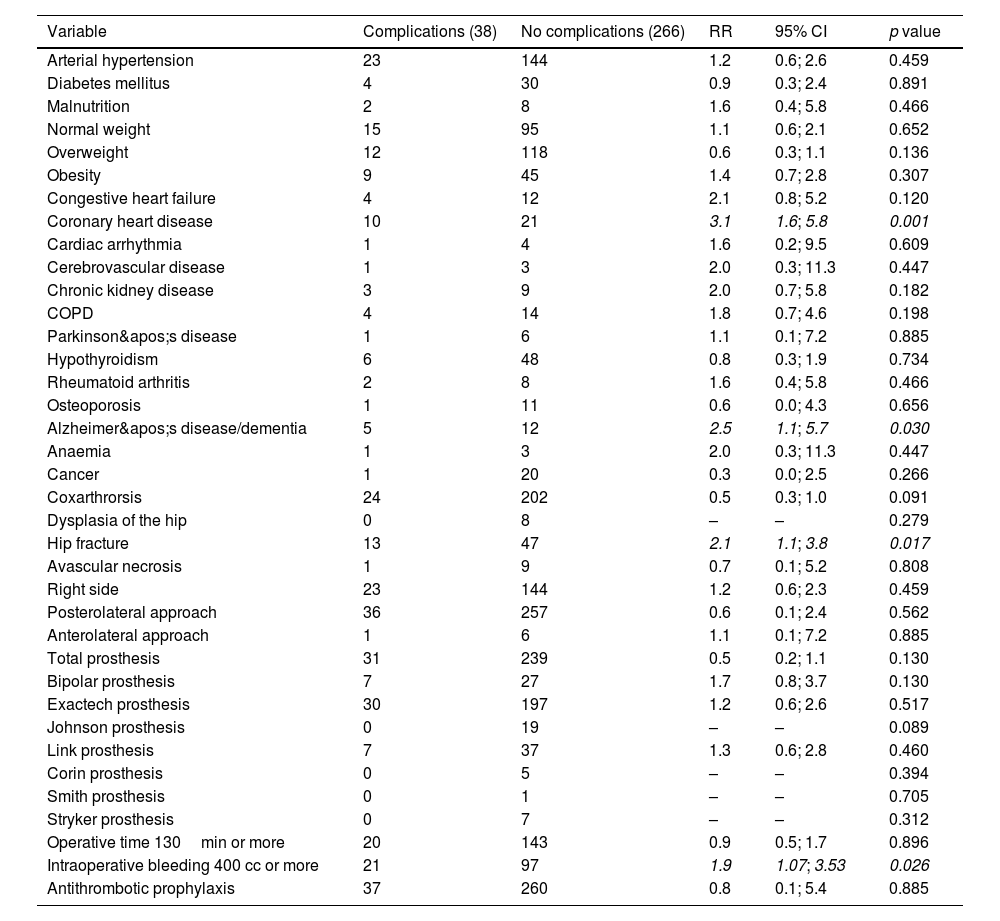
Bivariate analysisVariables were compared between two groups: 38 participants in the complication group and 266 individuals in the uncomplicated group. The mean age in the group of total hip arthroplasty patients with complications was 66 years (SD 18.7) and in the group without complications was 67.1 years (SD 15.1), with no significant statistical difference (p=0.686) in this regard. In the group with complications, 73.3% were female, while in the group without complications, 65% were female, again displaying no statistically significant difference (p=0.292). Thus, it was concluded that the groups were homogeneous when it came to the variables of both sex and age. The risk factors for complications in total hip arthroplasty in order of strength of association (highest to lowest) were: coronary heart disease RR 3.1 (95% CI 1.6; 5.8 p=0.001), Alzheimer's disease/dementia RR 2.5 (95% CI 1.1; 5.7 p=0.030), hip fracture as an indication for arthroplasty RR 2.1 (95% CI 1.1; 3.8 p=0.017), and surgical bleeding equal to or greater than 400 cc RR 1.9 (95% CI 1.07; 3.53 p=0.026) (Table 3).
Bivariate analysis of risk factors for complications in total hip replacement surgery.
| Variable | Complications (38) | No complications (266) | RR | 95% CI | p value |
|---|---|---|---|---|---|
| Arterial hypertension | 23 | 144 | 1.2 | 0.6; 2.6 | 0.459 |
| Diabetes mellitus | 4 | 30 | 0.9 | 0.3; 2.4 | 0.891 |
| Malnutrition | 2 | 8 | 1.6 | 0.4; 5.8 | 0.466 |
| Normal weight | 15 | 95 | 1.1 | 0.6; 2.1 | 0.652 |
| Overweight | 12 | 118 | 0.6 | 0.3; 1.1 | 0.136 |
| Obesity | 9 | 45 | 1.4 | 0.7; 2.8 | 0.307 |
| Congestive heart failure | 4 | 12 | 2.1 | 0.8; 5.2 | 0.120 |
| Coronary heart disease | 10 | 21 | 3.1 | 1.6; 5.8 | 0.001 |
| Cardiac arrhythmia | 1 | 4 | 1.6 | 0.2; 9.5 | 0.609 |
| Cerebrovascular disease | 1 | 3 | 2.0 | 0.3; 11.3 | 0.447 |
| Chronic kidney disease | 3 | 9 | 2.0 | 0.7; 5.8 | 0.182 |
| COPD | 4 | 14 | 1.8 | 0.7; 4.6 | 0.198 |
| Parkinson's disease | 1 | 6 | 1.1 | 0.1; 7.2 | 0.885 |
| Hypothyroidism | 6 | 48 | 0.8 | 0.3; 1.9 | 0.734 |
| Rheumatoid arthritis | 2 | 8 | 1.6 | 0.4; 5.8 | 0.466 |
| Osteoporosis | 1 | 11 | 0.6 | 0.0; 4.3 | 0.656 |
| Alzheimer's disease/dementia | 5 | 12 | 2.5 | 1.1; 5.7 | 0.030 |
| Anaemia | 1 | 3 | 2.0 | 0.3; 11.3 | 0.447 |
| Cancer | 1 | 20 | 0.3 | 0.0; 2.5 | 0.266 |
| Coxarthrorsis | 24 | 202 | 0.5 | 0.3; 1.0 | 0.091 |
| Dysplasia of the hip | 0 | 8 | – | – | 0.279 |
| Hip fracture | 13 | 47 | 2.1 | 1.1; 3.8 | 0.017 |
| Avascular necrosis | 1 | 9 | 0.7 | 0.1; 5.2 | 0.808 |
| Right side | 23 | 144 | 1.2 | 0.6; 2.3 | 0.459 |
| Posterolateral approach | 36 | 257 | 0.6 | 0.1; 2.4 | 0.562 |
| Anterolateral approach | 1 | 6 | 1.1 | 0.1; 7.2 | 0.885 |
| Total prosthesis | 31 | 239 | 0.5 | 0.2; 1.1 | 0.130 |
| Bipolar prosthesis | 7 | 27 | 1.7 | 0.8; 3.7 | 0.130 |
| Exactech prosthesis | 30 | 197 | 1.2 | 0.6; 2.6 | 0.517 |
| Johnson prosthesis | 0 | 19 | – | – | 0.089 |
| Link prosthesis | 7 | 37 | 1.3 | 0.6; 2.8 | 0.460 |
| Corin prosthesis | 0 | 5 | – | – | 0.394 |
| Smith prosthesis | 0 | 1 | – | – | 0.705 |
| Stryker prosthesis | 0 | 7 | – | – | 0.312 |
| Operative time 130min or more | 20 | 143 | 0.9 | 0.5; 1.7 | 0.896 |
| Intraoperative bleeding 400 cc or more | 21 | 97 | 1.9 | 1.07; 3.53 | 0.026 |
| Antithrombotic prophylaxis | 37 | 260 | 0.8 | 0.1; 5.4 | 0.885 |
COPD: chronic obstructive pulmonary disease.
In italics, factors that exhibited a statistically significant association.
Source: Drafted by the authors.
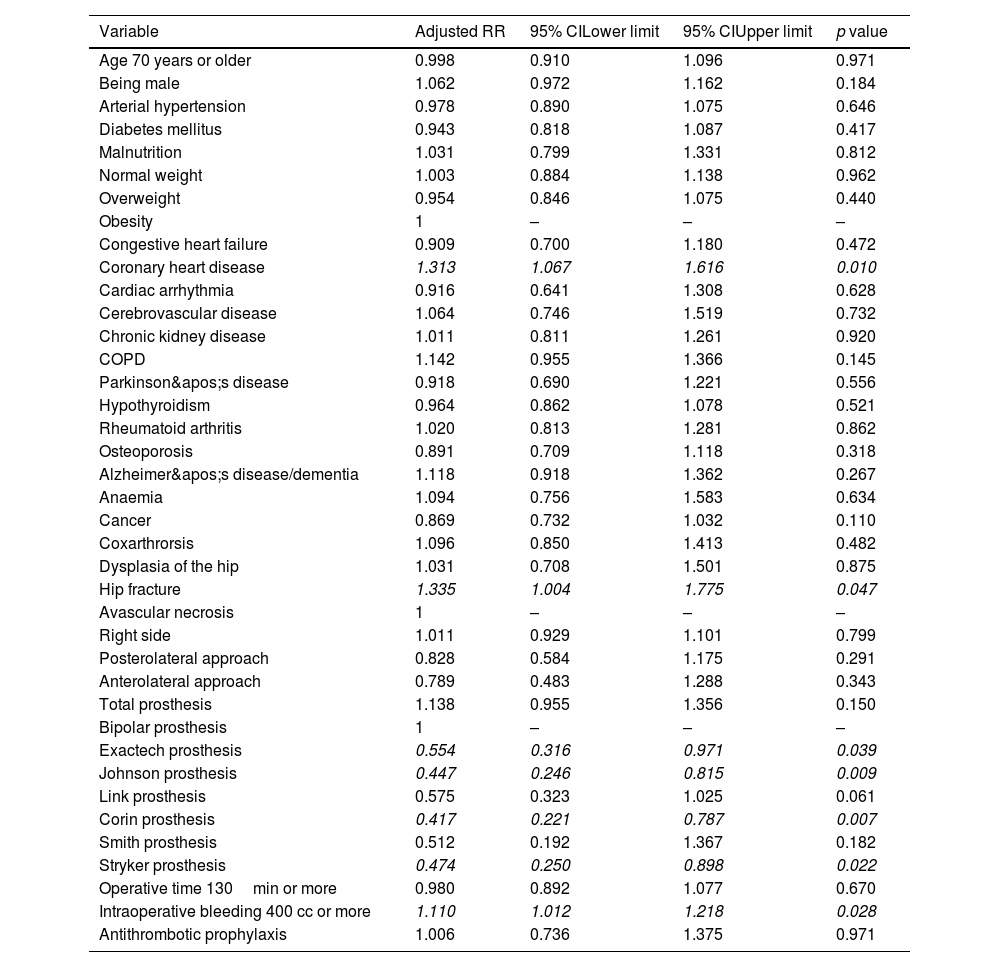
Given that the study sample consisted of a cohort with determination of cumulative incidence and calculation of relative risk, the Poisson regression model was used (categorical dependent variable, corresponding to the overall incidence of complications), all the variables that were analysed in the bivariate analysis were included (both those that were statistically significant as well as the variables with a theoretical representative value), and the model was accepted because the incidence deviation/degrees of freedom is 0.066 (<1). The factors that were associated as risk factors for complications in total hip arthroplasty were: hip fracture as an indication for total arthroplasty, coronary artery disease, and surgical bleeding equivalent to or in excess of 400 cc. The use of Exactech®, Johnson®, Corin®, and Stryker® prostheses was a protective factor. All of these implants were standard uncemented stems (Table 4).
Multivariate analysis and factors associated with complications in total hip replacement surgery.
| Variable | Adjusted RR | 95% CILower limit | 95% CIUpper limit | p value |
|---|---|---|---|---|
| Age 70 years or older | 0.998 | 0.910 | 1.096 | 0.971 |
| Being male | 1.062 | 0.972 | 1.162 | 0.184 |
| Arterial hypertension | 0.978 | 0.890 | 1.075 | 0.646 |
| Diabetes mellitus | 0.943 | 0.818 | 1.087 | 0.417 |
| Malnutrition | 1.031 | 0.799 | 1.331 | 0.812 |
| Normal weight | 1.003 | 0.884 | 1.138 | 0.962 |
| Overweight | 0.954 | 0.846 | 1.075 | 0.440 |
| Obesity | 1 | – | – | – |
| Congestive heart failure | 0.909 | 0.700 | 1.180 | 0.472 |
| Coronary heart disease | 1.313 | 1.067 | 1.616 | 0.010 |
| Cardiac arrhythmia | 0.916 | 0.641 | 1.308 | 0.628 |
| Cerebrovascular disease | 1.064 | 0.746 | 1.519 | 0.732 |
| Chronic kidney disease | 1.011 | 0.811 | 1.261 | 0.920 |
| COPD | 1.142 | 0.955 | 1.366 | 0.145 |
| Parkinson's disease | 0.918 | 0.690 | 1.221 | 0.556 |
| Hypothyroidism | 0.964 | 0.862 | 1.078 | 0.521 |
| Rheumatoid arthritis | 1.020 | 0.813 | 1.281 | 0.862 |
| Osteoporosis | 0.891 | 0.709 | 1.118 | 0.318 |
| Alzheimer's disease/dementia | 1.118 | 0.918 | 1.362 | 0.267 |
| Anaemia | 1.094 | 0.756 | 1.583 | 0.634 |
| Cancer | 0.869 | 0.732 | 1.032 | 0.110 |
| Coxarthrorsis | 1.096 | 0.850 | 1.413 | 0.482 |
| Dysplasia of the hip | 1.031 | 0.708 | 1.501 | 0.875 |
| Hip fracture | 1.335 | 1.004 | 1.775 | 0.047 |
| Avascular necrosis | 1 | – | – | – |
| Right side | 1.011 | 0.929 | 1.101 | 0.799 |
| Posterolateral approach | 0.828 | 0.584 | 1.175 | 0.291 |
| Anterolateral approach | 0.789 | 0.483 | 1.288 | 0.343 |
| Total prosthesis | 1.138 | 0.955 | 1.356 | 0.150 |
| Bipolar prosthesis | 1 | – | – | – |
| Exactech prosthesis | 0.554 | 0.316 | 0.971 | 0.039 |
| Johnson prosthesis | 0.447 | 0.246 | 0.815 | 0.009 |
| Link prosthesis | 0.575 | 0.323 | 1.025 | 0.061 |
| Corin prosthesis | 0.417 | 0.221 | 0.787 | 0.007 |
| Smith prosthesis | 0.512 | 0.192 | 1.367 | 0.182 |
| Stryker prosthesis | 0.474 | 0.250 | 0.898 | 0.022 |
| Operative time 130min or more | 0.980 | 0.892 | 1.077 | 0.670 |
| Intraoperative bleeding 400 cc or more | 1.110 | 1.012 | 1.218 | 0.028 |
| Antithrombotic prophylaxis | 1.006 | 0.736 | 1.375 | 0.971 |
COPD: chronic obstructive pulmonary disease.
In italics, factors that exhibited a statistically significant association (p value of less than 0.05).
Source: Drafted by the authors.
Revision hip replacement entails an increased risk of complications, risk of bleeding, longer hospital stays, and higher financial costs for health care systems.12 In the United States, revision rates for arthroplasties of the hip have been reported to be as high as 17.5% of cases, while in Europe these rates are as low as 6.4% after five years of follow-up.13 In the current study, the revision rate was found to be 4.6%. Paez et al. reported a lower revision rate following total hip replacement, with an incidence of 2.7%.14 Dislocation of the hip prosthesis is the number one cause leading to revision in the United States, raising economic costs by 300%.15 The dislocation rate in this research work was 2%, which is compatible with data reported in the literature, where an incidence between 0.2% and 5% has been documented.16
Periprosthetic infection is a major complication of total hip arthroplasty,17 which results in multiple revision surgeries and long-term antibiotic treatment, adversely affecting the patient; increasing periods of immobility, the number of readmissions to the emergency department, and compromising quality of life.18 According to Franceschini et al., deep infection is associated with increased morbidity and has an incidence rate of approximately 2%19; a similar incidence of 1.6% was identified in the present study. Meanwhile, Papagrigorakis et al. reported that periprosthetic fracture was noted in 14% of the people treated with total hip arthroplasty and osteoporosis, which translates into loss of function, as well as increased pain and morbidity and mortality.20 Contrary to their results, our study identified an incidence of periprosthetic fracture of 1.3%; however, participants were not stratified on the basis of the presence or absence of osteoporosis, which may explain the discrepancies. Peripheral nerve damage is a rare complication of hip replacement surgery. In their study, Hasija et al. reported an incidence of 0.6% to 3.7%,21 which is in line with the incidence of peripheral nerve damage found in the present study, which was 0.7%. If we look at the study by Zeng et al., which included 210,450 participants treated with total hip replacement, a mortality rate of between 2.6 and 2.9% was observed in the first 30 days following surgery22; their registry displays a higher mortality rate compared to the results of this research, in which the mortality rate was found to be 1.3%.
Coronary heart disease is known to be a risk factor that is conducive to worse operative outcomes in orthopaedic surgery23; specifically in the case of hip arthroplasty, cardiac disease is associated with longer hospital stays, increased readmission rates, and higher mortality.24,25 In this study, coronary heart disease was identified as a risk factor for complications in total hip arthroplasty; similar results were reported by Edwards et al. who also found heart disease to be a risk factor for complications following hip arthroplasty.23 A systematic review of the literature published by Stibolt et al. documented an increased risk of complications among patients with hip fracture who had undergone hip arthroplasty.26 This corroborates the results of the present research, in which hip fracture as an indication for total arthroplasty was demonstrated to be a risk factor for complications. Significant blood loss during total hip replacement can increase the rate of blood transfusion,27 which negatively impacts surgical outcomes and increases the incidence of complications.28 Surgical bleeding equal to or greater than 400 cc was documented in this work to be another risk factor for complications in replacement surgery.
ConclusionThe risk factors for complications in total hip replacement surgery were as follows: hip fracture as the indication for the total arthroplasty, coronary heart disease, and intraoperative bleeding with a loss of 400 cc or more.
Level of evidenceLevel of evidence II.
Ethical considerationsThis study was conducted in accordance with the ethical standards recognised by the Declaration of Helsinki and Resolution 008430 dated 1993 and has received the approval of the Institution's Ethics Committee. Informed consent was not required given that the research was retrospective in nature and data were obtained from clinical records.
FundingThis research has not received any specific grants from any public or commercial sector or from any non-profit organisations.
Conflicts of interestThe authors have no conflict of interests to declare.