Talo-calcaneal coalition (TCC), presents a significant challenge in adult patients, often associated with pes planus and pes cavus. The aim of this study was to assess the effect of Medial Displacement Calcaneal Osteotomy (MDCO) on TTC.
Materials and methodsThis study retrospectively analyzed 11 adult patients diagnosed with rigid flat feet caused by TCC, who underwent MDCO without coalition resection. Clinical and radiographic outcomes were assessed using questionnaires (ADL-FAAM, VAS and Likert scale) and imaging (Talar-first Metatarsal angle, Talo-calcaneal angle, both in AP and lateral views, and Talo-navicular Coverage) preoperatively and at one-year follow-up. Postoperative complications, infections or subsequent surgical procedures were also registered during follow up.
ResultsOne year postoperatively, the mean improvement in ADL-FAAM was −49 (SD 15.73), VAS was −6.7 (SD 1.21) and Likert scale −2.6 (SD 0.46). Radiographic analysis post-surgery revealed minimal changes, emphasizing that the substantial clinical benefits were primarily due to the correction of malalignment. A significant correlation was found between talo-calcaneal angles and talo-navicular coverage with postoperative FAAM scores (p=0.011, p=0.047), and talo-calcaneal angles with Likert scores (p=0.05, p=0.008). Patients with more severe preoperative valgus deformities experienced increased improvement.
ConclusionMDCO without coalition resection offers a treatment alternative for adults with TCC-induced flatfoot.
Level of evidenceLevel IV, retrospective case series.
La coalición talocalcánea (TCC) se asocia a deformidades como el pie plano y el pie cavo y representa un reto terapéutico en el adulto. El objetivo de este estudio fue evaluar el efecto de la Osteotomía Medializadora de Calcáneo (MDCO) en el tratamiento de la TCC.
MétodoSe analizaron retrospectivamente a 11 pacientes adultos diagnosticados de pies plano rígido causado por TCC, que fueron sometidos a MDCO sin resección de la coalición. Se evaluaron los resultados clínicos y radiográficos mediante cuestionarios (ADL-FAAM, VAS y escala Likert) e imágenes (ángulo talo-primer metatarsiano, ángulo talo-calcáneo en anteroposterior y lateral, y cobertura talo-navicular) en el preoperatorio y a un año de seguimiento. Durante el seguimiento se registraron complicaciones postoperatorias, infecciones y necesidad de procedimientos quirúrgicos posteriores.
ResultadosA un año postoperatorio, la mejora media fue de -49 (DE 15.73) en ADL-FAAM, de -6.7 (DE 1.21) en VAS y de -2.6 (DE 0.46) en la escala Likert. El análisis radiográfico postquirúrgico mostró cambios mínimos. Se encontró una correlación significativa entre los ángulos talo-calcáneos y la cobertura talo-navicular preoperatorios con el FAAM postoperatorios (p=0.011, p=0.047), así como entre los ángulos talo-calcáneos preoperatorios y la escala Likert (p=0.05, p=0.008). Los pacientes con deformidades en valgo preoperatorias más severas experimentaron una mayor mejora.
ConclusiónLa MDCO sin resección de la coalición es una alternativa terapéutica para el tratamiento del pie plano del adulto causado por una TCC.
Nivel de evidenciaNivel IV, serie de casos retrospectiva.
Tarsal coalition is a congenital disorder characterized by the fusion of two or more tarsal bones, resulting in a stiff and painful foot, often associated with malalignment deformities including pes planus1 and pes cavus.2 Talo-calcaneal coalition (TCC) is challenging since its optimal treatment is still controversial in the adult population. While the most common treatment approach for symptomatic TCC in children is surgical resection of the bony bridge,3 this approach showed unpredictable results in adults.4 Surgical intervention for this group of patients involves different types of arthrodesis, and due to inconsistent outcomes, the gold standard technique is yet to be defined.5
In recent years, there has been growing interest in realignment procedures, such as Medial Displacement Calcaneal Osteotomy (MDCO), as an alternative treatment option for tarsal coalitions.6–8 These procedures aim to improve foot function and alleviate symptoms by correcting the malalignment and restoring the normal biomechanics of the foot, without removing the coalition itself. Since the publication of Mosca et al. in 2012,6 this line of research has become increasingly widespread. However, there are only isolated case reports and very few publications on this technique in adults.7,8
The purpose of this study is to report a series of 11 adult patients diagnosed with flat feet caused by TCC who underwent realignment procedures through MDCO without coalition resection, and to evaluate the clinical and radiographic outcomes of this approach. We hypothesize that realignment via medializing calcaneal osteotomy will provide effective pain relief and improve functional outcomes for adult patients with symptomatic coalitions, without the need for resection of the coalition nor some kind of arthrodesis.
Material and methodsPatientsFrom January 2011 to December 2019 all consecutive patients who had a diagnosis of rigid flat feet (hindfoot valgus) associated to a TCC and underwent an isolated MDCO without coalition resection were identified. The indications for operative intervention were a hindfoot valgus with continued unremitting pain for more than six months and failure of nonoperative treatments. Exclusion criteria included paediatric population, TCC resection or any form of arthrodesis.
Description of therapeutic interventionCases were treated surgically by two experienced foot and ankle surgeons using a technique previously described in the literature.6,7 Under spinal anaesthesia, in prone and with tourniquet, a MDCO was performed through an oblique incision to expose the lateral wall of the calcaneus and correct the malalignment by displacing the tuberosity. Displacement of 10mm was determined intraoperatively using calcaneus long axials views and fixation was achieved through 2 headless compression screws (Fig. 1). Postoperatively, patients were placed in short leg cast without weightbearing for 4 weeks, followed by 4 weeks of rehabilitation with progressive range-of-motion and partial weightbearing to allow full weightbearing at 8 weeks postoperatively.
Baseline dataFor all those patients included, a clinical examination and clinical chart review was performed to obtain data on onset of pain, previous trauma or injury, pain site, laterality, conservative treatments, hindfoot alignment (valgus/neutral/varus) and subtalar range of motion (grades). Moreover, preoperative CT scans were reviewed to confirm the diagnosis and determine the type of coalition (bone or cartilage).
Clinical outcomesAll included patients, performed at baseline and at one-year follow up 3 questionnaires: the Activity Daily Living (ADL) subscale of the Foot and Ankle Ability Measure (FAAM) score,9 the Visual Analogue Scale (VAS) pain, and the Likert scale.10 The main outcome of this study was the ADL subscale of the FAAM score which is a self-report measure that assesses physical function of individuals with lower leg, foot, and ankle musculoskeletal disorders.11 The response to each item on the ADL subscale is scored from 4 – no difficulty – to 0 – unable to do, with a final % representing higher scores higher physical functionality. The VAS pain assesses pain from 0 – no pain–, to 10 – maximal pain.
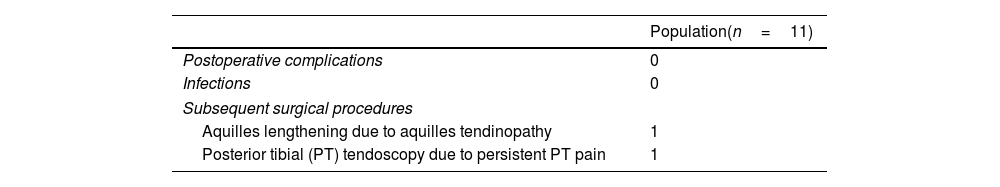
During the rest of follow up, events of interest were also registered including postoperative complications, infection, and subsequent surgical procedures.
Radiographic outcomesAll included patients, performed at baseline and at one-year follow up AP and lateral weight-bearing radiographs. Those were measured to quantify the AP and lateral Talar-first Metatarsal angle (AP T-M1 and LAT T-M1), the AP and Lateral Talo-Calcaneal angle (AP TC and LAT TC) and the AP Talo-Navicular Coverage (TNC)12 (Fig. 2).
Statistical analysisResults were analyzed descriptively from the baseline database. Continuous variables were expressed as means and standard deviations (SD) or medians and interquartile ranges (IQRs), depending on their distribution's normality. Categorical variables were reported as frequencies and percentages. Continuous variables were compared using the independent-samples t-test for data with a normal distribution and the Wilcoxon rank-sum test for data without normal distribution, as determined by the Shapiro–Wilk test. Categorical variables were compared using Chi-squared and Fisher's exact tests. To assess the impact of preoperative and postoperative radiographic deformity on clinical scores, correlations between radiographic measurements (AP T-M1, LAT T-M1, AP TC, LAT TC, and TNC) and clinical scores (ADL/FAAM, VAS, Likert) were evaluated using Pearson's correlation for normally distributed variables and Spearman's rank correlation for variables not normally distributed. Statistical significance was established at a p-value<0.05. Statistical analyses were conducted using R (Version 4.0.5, R Core Team, 2021) within the RStudio IDE (Version 1.4.1106).
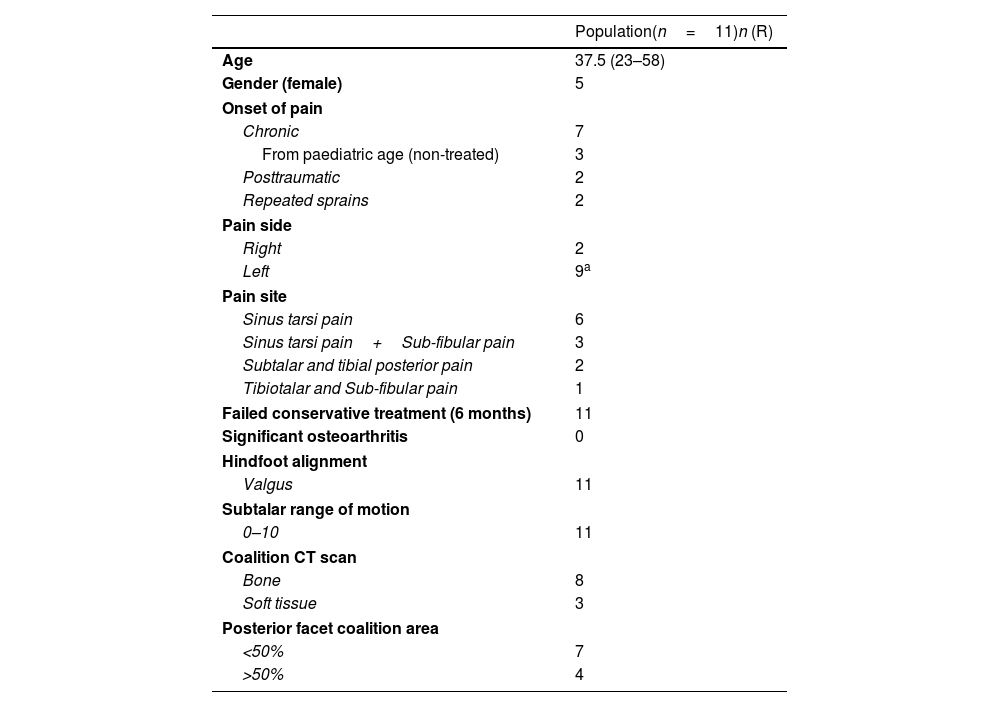
ResultsThe study included 11 patients diagnosed by CT scan with rigid flat feet caused by TCC who underwent an isolated MDCO without coalition resection between 2011 and 2019, with an average follow up of 8 years (4–12). Population and baseline characteristics are summarized in Table 1.
Population and baseline characteristics.
| Population(n=11)n (R) | |
|---|---|
| Age | 37.5 (23–58) |
| Gender (female) | 5 |
| Onset of pain | |
| Chronic | 7 |
| From paediatric age (non-treated) | 3 |
| Posttraumatic | 2 |
| Repeated sprains | 2 |
| Pain side | |
| Right | 2 |
| Left | 9a |
| Pain site | |
| Sinus tarsi pain | 6 |
| Sinus tarsi pain+Sub-fibular pain | 3 |
| Subtalar and tibial posterior pain | 2 |
| Tibiotalar and Sub-fibular pain | 1 |
| Failed conservative treatment (6 months) | 11 |
| Significant osteoarthritis | 0 |
| Hindfoot alignment | |
| Valgus | 11 |
| Subtalar range of motion | |
| 0–10 | 11 |
| Coalition CT scan | |
| Bone | 8 |
| Soft tissue | 3 |
| Posterior facet coalition area | |
| <50% | 7 |
| >50% | 4 |
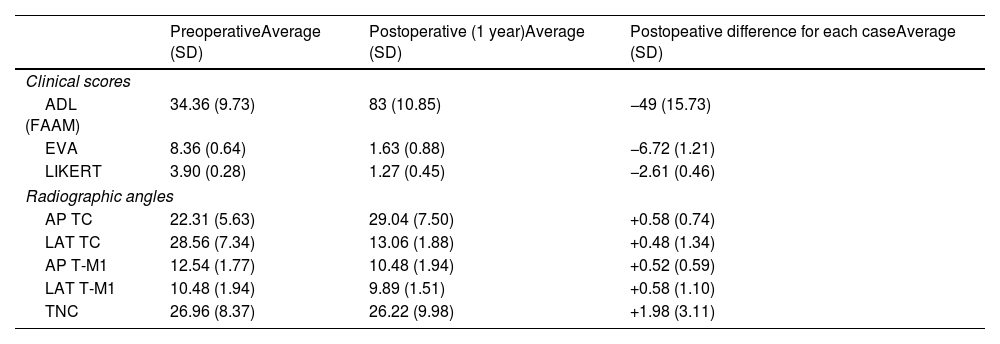
Baseline and 1-year postoperative ADL (FAAM), VAS and Likert tests and weight bearing radiographical measurements are presented in Table 2. All the clinical scores improved postoperatively, while radiographic parameters presented minimum variations (Fig. 3). During follow up, there were no postoperative complications or infection, but 2 patients required a subsequent surgical procedure (Table 3).
Descriptive preoperative and 1 year postoperative results of ADL (FAAM), EVA, Likert scores and radiographic measurements.
| PreoperativeAverage (SD) | Postoperative (1 year)Average (SD) | Postopeative difference for each caseAverage (SD) | |
|---|---|---|---|
| Clinical scores | |||
| ADL (FAAM) | 34.36 (9.73) | 83 (10.85) | −49 (15.73) |
| EVA | 8.36 (0.64) | 1.63 (0.88) | −6.72 (1.21) |
| LIKERT | 3.90 (0.28) | 1.27 (0.45) | −2.61 (0.46) |
| Radiographic angles | |||
| AP TC | 22.31 (5.63) | 29.04 (7.50) | +0.58 (0.74) |
| LAT TC | 28.56 (7.34) | 13.06 (1.88) | +0.48 (1.34) |
| AP T-M1 | 12.54 (1.77) | 10.48 (1.94) | +0.52 (0.59) |
| LAT T-M1 | 10.48 (1.94) | 9.89 (1.51) | +0.58 (1.10) |
| TNC | 26.96 (8.37) | 26.22 (9.98) | +1.98 (3.11) |
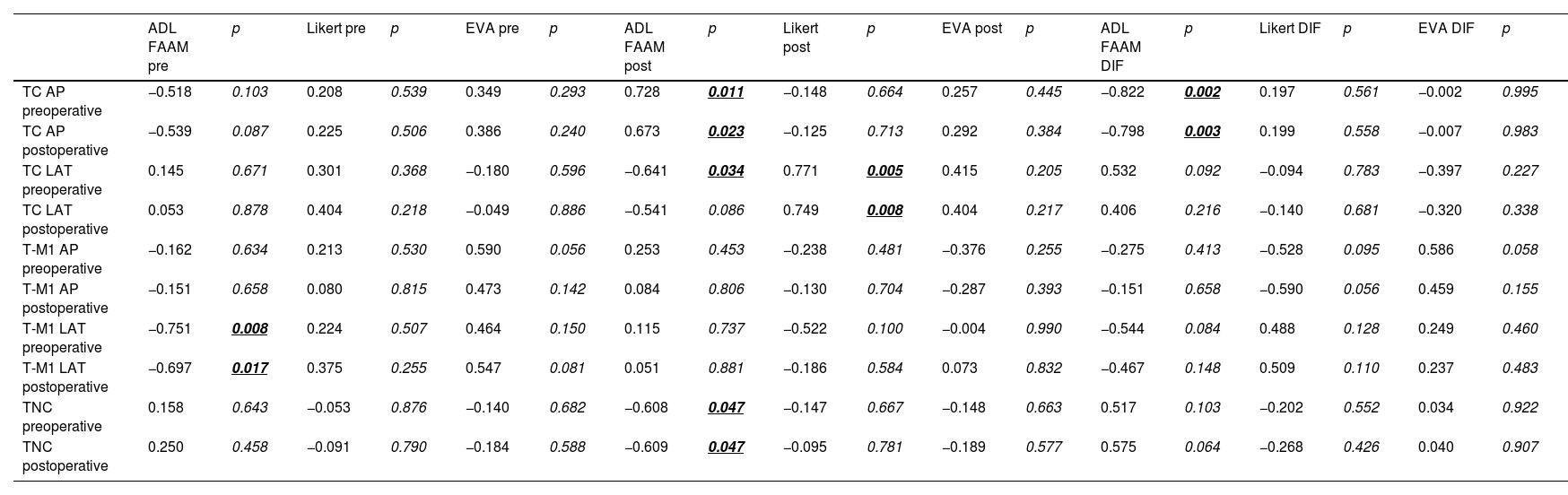
The statistical analysis presented that there is significative correlation between preoperative and postoperative TC-AP angles and TNC and postoperative FAAM scores (p=0.011, p=0.023 and p=0.047, p=0.047 respectively). There is also correlation between pre and postoperative TC-LAT angles and postoperative Likert scores (p=0.05, p=0.008). Globally, patients presenting with greater TC-AP and TNC angles, both pre or postoperative, had a higher correlation of improved results according to FAAM, while those with higher preoperative T-M1 angles to Likert score. This reflects, the more severe valgus deformities obtained the better clinical improvement through this procedure (Table 4).
Relation of postoperative FAAM, EVA and LIKERT scores with preoperative and postoperative radiographic measurements.
| ADL FAAM pre | p | Likert pre | p | EVA pre | p | ADL FAAM post | p | Likert post | p | EVA post | p | ADL FAAM DIF | p | Likert DIF | p | EVA DIF | p | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| TC AP preoperative | −0.518 | 0.103 | 0.208 | 0.539 | 0.349 | 0.293 | 0.728 | 0.011 | −0.148 | 0.664 | 0.257 | 0.445 | −0.822 | 0.002 | 0.197 | 0.561 | −0.002 | 0.995 |
| TC AP postoperative | −0.539 | 0.087 | 0.225 | 0.506 | 0.386 | 0.240 | 0.673 | 0.023 | −0.125 | 0.713 | 0.292 | 0.384 | −0.798 | 0.003 | 0.199 | 0.558 | −0.007 | 0.983 |
| TC LAT preoperative | 0.145 | 0.671 | 0.301 | 0.368 | −0.180 | 0.596 | −0.641 | 0.034 | 0.771 | 0.005 | 0.415 | 0.205 | 0.532 | 0.092 | −0.094 | 0.783 | −0.397 | 0.227 |
| TC LAT postoperative | 0.053 | 0.878 | 0.404 | 0.218 | −0.049 | 0.886 | −0.541 | 0.086 | 0.749 | 0.008 | 0.404 | 0.217 | 0.406 | 0.216 | −0.140 | 0.681 | −0.320 | 0.338 |
| T-M1 AP preoperative | −0.162 | 0.634 | 0.213 | 0.530 | 0.590 | 0.056 | 0.253 | 0.453 | −0.238 | 0.481 | −0.376 | 0.255 | −0.275 | 0.413 | −0.528 | 0.095 | 0.586 | 0.058 |
| T-M1 AP postoperative | −0.151 | 0.658 | 0.080 | 0.815 | 0.473 | 0.142 | 0.084 | 0.806 | −0.130 | 0.704 | −0.287 | 0.393 | −0.151 | 0.658 | −0.590 | 0.056 | 0.459 | 0.155 |
| T-M1 LAT preoperative | −0.751 | 0.008 | 0.224 | 0.507 | 0.464 | 0.150 | 0.115 | 0.737 | −0.522 | 0.100 | −0.004 | 0.990 | −0.544 | 0.084 | 0.488 | 0.128 | 0.249 | 0.460 |
| T-M1 LAT postoperative | −0.697 | 0.017 | 0.375 | 0.255 | 0.547 | 0.081 | 0.051 | 0.881 | −0.186 | 0.584 | 0.073 | 0.832 | −0.467 | 0.148 | 0.509 | 0.110 | 0.237 | 0.483 |
| TNC preoperative | 0.158 | 0.643 | −0.053 | 0.876 | −0.140 | 0.682 | −0.608 | 0.047 | −0.147 | 0.667 | −0.148 | 0.663 | 0.517 | 0.103 | −0.202 | 0.552 | 0.034 | 0.922 |
| TNC postoperative | 0.250 | 0.458 | −0.091 | 0.790 | −0.184 | 0.588 | −0.609 | 0.047 | −0.095 | 0.781 | −0.189 | 0.577 | 0.575 | 0.064 | −0.268 | 0.426 | 0.040 | 0.907 |
In this study, we assessed 11 adult patients with flatfeet caused by a TCC treated with a MDCO without coalition resection. The outcomes obtained from this case series demonstrate the potential effect of the MDCO realigning procedure in achieving satisfactory outcomes in this group of patients.
Rigid flatfeet resulting from a TCC is a challenging condition to manage, and there is ongoing debate regarding the optimal treatment approach. In recent years, there has been growing interest in realignment procedures as an alternative treatment option for tarsal coalitions.13 The rationale behind our approach lies in the understanding that the primary cause of symptoms in this group of patients is the abnormal foot alignment. By performing a MDCO, we were able to correct the valgus deformity and restore a more anatomically aligned foot. Although this philosophy has increased its popularity,6–8 consistent publications are sparse. Mosca et al.6 in 2012 reported 13 valgus deformity associated TCC, mean age 13.5 years, treated through calcaneal lengthening osteotomy with gastrocnemius or Achilles tendon lengthening and reporting successful results at 5–11y follow up. Cho et al.,7 in 2018 reported a case of a 15yo female with a TCC and varus deformity treated through sliding calcaneal osteotomy for hindfoot realignment. Shang et al.,8 in 2020 presented 13 cases of TCC with hindfoot valgus deformities that underwent Evans lateral lengthening calcaneal osteotomy, mean 15yo with reporting improvement on AOFAS, VAS and TMT, TCA angles.
We align with Mosca6 on the ability of the MDCO to reorientate the Chopart joint and allow them to function as a pseudo-subtalar joint, decreasing transfer forces to ankle. The results of our study support the potential effectiveness of this realignment technique. All 11 patients in our cohort experienced improvements in pain and functional ability following the MDCO. Importantly, none of the patients required a reintervention via subtalar arthrodesis. It is worthy to note that “lateral side pain”, which can include sinus tarsi, subtalar and sub-fibular impingement, are interpreted as a pathological overload due to malalignment and may be aligned with this use of this realigning procedures. However, it is important to highlight that complete clinical improvement is seldom achieved in these patients due to the inherent mechanical limitations they experience. In this series, no significant arthritic changes were observed in the described cases, which could have potentially influenced the obtained outcomes. Despite the favourable outcomes, residual pain or discomfort may persist because of the underlying mechanical constraints imposed by the coalition, as described in our series, with 2/11 cases who required aquilles lengthening and posterior tibial tendoscopy. In addition, is important to highlight that our results showed that radiographic flat feet parameters did not improve postoperatively. This is not surprising since we did not alter the relationship between the talus and the calcaneus. We can assume that we were not able to identify changes in the radiographic assessment because we did not include a hind foot view (e.g. Saltzman view) or a weightbearing CT scan. Although it might seem obvious that by not resecting the coalition, the hindfoot radiographic angles should not change, there may be more distal changes as a consequence of compensatory dynamic forefoot supination of the Chopart join, which could be modified by realigning the hindfoot. Interestingly, the patients who showed greater TC AP and worst TNC (most severe valgus deformities) experienced the best clinical results, reflecting the clinical benefit of realignment. These results differ from those presented by Shang, who describes improvement of radiological parameters, but in a paediatric population.
As a strength of this study, is important to highlight that this study represents the largest series published to date of MDCO to treat TCC in the adult population. This mid-term (8 years) follow-up provides valuable insights into the outcomes and management of this challenging condition in this group of patients.
However, it is important to note that this study has certain limitations. The sample size was relatively small, and the retrospective nature of the study introduces inherent biases. Preoperative SPECT were not available and the lack of X-ray at latest follow up, the lack of available Saltzman views and weight bearing CT scan weakened a more in-depth analysis of these patients.
ConclusionIn conclusion, our study proposes that a MDCO without coalition resection is an effective treatment option for valgus flatfoot caused by TCC. This technique addresses the underlying alignment issues, providing satisfactory outcomes and avoiding the potential complications associated with coalition resection or arthrodesis. Further research with larger patient cohorts and prospective study designs is needed to validate these findings and establish the long-term durability of this treatment approach for this challenging condition.
Level of evidenceLevel of evidence IV.
Ethics approvalInstitutional review board approval was obtained for this study IRB 2023/129.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interestNone.
None.