Currently, most hospitals systematically request preoperative crossmatching tests for patients undergoing arthroplasty. The aim of this study is to assess whether routine preoperative crossmatch testing (CMT) is necessary for all patients undergoing primary total hip arthroplasty (THA). To this end, we evaluated the transfusion rate, associated clinical risk factors, and the economic impact of routine crossmatch testing.
Material and methodsA retrospective study including patients undergoing primary THA for coxarthrosis from 2021 to 2023. Patients with fractures and their complications, as well as prosthetic revisions, were excluded. Epidemiological, clinical, and analytical variables, as well as the cost of routinely performing preoperative CMT were evaluated.
ResultsA total of 273 patients were included (152 males), with a mean age of 66.9 years [27–89]. Tranexamic acid was administered to 207 patients (75.8%), and surgical drains were used in 133 cases (48.7%). The decision to use tranexamic acid and drains was made by the attending anaesthesiologist and surgeon, respectively. The mean length of hospital stay was 2.5 days [1.2–3.7]. All surgeries were performed using a posterolateral approach, and all prostheses implanted were uncemented Polar R3® (Smith & Nephew) components. The mean preoperative haemoglobin level was 14.3g/dL [10–19.7], and the postoperative level was 11.1g/dL [7.2–14.7]. Blood transfusion was required in 20 patients (7.3%). No urgent or intraoperative transfusions were recorded; all were prescribed postoperatively at the discretion of the attending surgeon. Female sex, the use of surgical drains, and preoperative haemoglobin<13g/dL were identified as statistically significant risk factors for transfusion (p<0.05). The estimated cost of routine PPCC was €21,840.
ConclusionsThe blood transfusion rate following primary THA was less than 10% (7.3%). It seems reasonable to stop routinely performing CMT for every patient undergoing primary THA and to individualise the indication for transfusion based on each specific case.
En la actualidad se concibe necesaria la realización sistemática de pruebas cruzadas preoperatorias en las intervenciones por artroplastia en la mayor parte de hospitales. Nuestro objetivo es analizar si la solicitud de pruebas cruzadas (PPCC) preoperatorias de forma sistemática es necesaria en todo paciente intervenido de prótesis total de cadera (PTC) primaria; para ello determinamos la tasa de transfusión sanguínea en pacientes intervenidos de PTC primaria, factores de riesgo clínicos asociados y el impacto económico derivado de su solicitud.
Material y métodosEstudio retrospectivo incluyendo los pacientes intervenidos de PTC por coxartrosis primaria durante los años 2021 a 2023. Excluimos pacientes con fracturas y sus complicaciones, así como recambios protésicos. Se evalúan variables epidemiológicas, clínicas y analíticas, así como el coste de realizar PPCC preoperatorias de forma rutinaria.
ResultadosSe incluyeron 273 pacientes (152 hombres). Edad media 66,9 años [27-89]. Se administró ácido tranexámico a 207 pacientes (75,8%) y se colocó drenaje en 133 pacientes (48,7%). El uso de ácido tranexámico y de drenaje fueron a criterio del anestesista y cirujano, respectivamente, basados en la evidencia disponible. La media de ingreso fue 2,5 días [1,2-3,7]. Se realizó abordaje posterolateral en todos los casos. Todas las PTC fueron Polar R3 (Smith & Nephew®) no cementadas. La hemoglobina (Hb) preoperatoria media fue de 14,3g/dl [10-19,7], y la postoperatoria fue de 11,1 [7,2-14,7]. Se transfundió a 20 pacientes (7,3%). Ninguna transfusión fue urgente y ninguna se realizó durante el día de la cirugía (siendo bajo criterio del cirujano responsable del paciente teniendo en cuenta una Hb por debajo de 8g/dl). El sexo femenino, el uso de drenaje y la Hb preoperatoria <13g/dl fueron factores de riesgo para transfusión sanguínea (p<0,05). El coste de realizar PPCC de forma rutinaria fue de 21.840 euros en total.
ConclusionesEl porcentaje de transfusión sanguínea tras PTC primaria fue menor del 10% (7,3%). Parece razonable dejar de realizar PPCC sistemáticas a todo paciente intervenido de PTC primaria e individualizar la indicación de transfusión según cada caso concreto.
IntroductionHip osteoarthritis is one of the most prevalent musculoskeletal conditions globally, which affected an estimated 7.6% of the world's population in 2020, equivalent to approximately 595 million people.1 The progressive ageing of the population and the consequent increase in life expectancy have contributed to a growing demand for primary total hip replacements (THRs) in recent years.2
Blood loss associated with total hip arthroplasty and the resulting need for blood product transfusions have historically been a key aspect of perioperative management. In the early 2000s, transfusion rates in this type of surgery were considerably high, ranging from 30% to 50%.3 Currently, thanks to improved perioperative patient management, these rates have been significantly reduced, reaching figures between 2% and 7% in some studies.4 However, predisposing factors that increase the risk of bleeding persist, including advanced age, low body mass index, untreated preoperative anaemia, and the presence of coagulopathies.5
The systematic request for cross-matching (CM) in patients eligible for primary total hip replacements (THRs) has been controversial in recent years because its indiscriminate use entails a significant consumption of material and human resources, as well as a considerable economic cost for the healthcare system. Furthermore, blood transfusion is not without clinical risks, including volume overload, immunological reactions, immunosuppression, with the consequent increased risk of infection, as well as electrolyte imbalances, all of which can increase the overall morbidity and mortality of the procedure.6,7
Therefore, several centres are advocating for the implementation of patient blood management strategies aimed at minimising transfusions in clinical practice and reducing the risk of bleeding in the surgical setting.4
The aim of this study was to analyse whether the systematic request for preoperative CM is truly necessary for all patients undergoing total hip replacement (THR). To this end, we determined the blood transfusion rate in patients undergoing primary THR, the associated clinical risk factors, and the economic impact of requesting these tests.
Material and methodsWe conducted a retrospective study that included all patients over 18 years of age who underwent primary THR for hip osteoarthritis between 2021 and 2023 at our centre. Patients who underwent surgery for fractures, their complications, or revision prosthetic surgery were excluded. Patients with coagulation disorders were also excluded, as these may have an increased risk of bleeding.
Our variables included sex, anaesthetic risk classification according to the ASA (American Society of Anaesthesiologists) scale; the laterality of the operated hip; the surgical approach; administration of tranexamic acid; use of drainage: postoperative blood transfusion and the timing of the transfusion (distinguishing between urgent transfusions or those performed on the first postoperative day and those performed on the second or third postoperative day). Patient-specific variables such as the use of anticoagulants and antiplatelet agents before the procedure, hypertension, and diabetes mellitus; and quantitative variables such as age; the number of days of hospitalisation from surgery to discharge; preoperative and postoperative haemoglobin (Hb) levels and the difference between them, and preoperative and postoperative haematocrit (Hct) levels and the difference between them.
In addition to previously recorded cardiovascular history, such as hypertension and diabetes mellitus, personal histories of ischaemic heart disease, as well as relevant haematological and oncological conditions, were collected. This data was considered to identify potentially influential comorbidities in clinical decision-making regarding the indication for blood transfusion in the perioperative setting.
Decisions regarding the indication for postoperative blood transfusion (general indications according to the Spanish Society of Haematology are Hb<7g/dL or <8g/dL with anaemia or haematological or oncological pathology)8 the use of drainage, and the type of surgical approach employed (anterolateral or posterolateral) were left to the discretion of the surgeon responsible for each procedure. Similarly, the administration of tranexamic acid was determined by the anaesthesiologist, “generally using it except in cases of cardiovascular pathology.” Consequently, during the study period, there was no standardised protocol for its administration.
As postoperative thromboembolic prophylaxis, all patients received treatment with low molecular weight heparin at prophylactic doses (40mg every 24h), following the established recommendations for major orthopaedic surgery.9
All data were recorded from patient medical records and compiled in a spreadsheet using IBM SPSS version 29.9 (New York, USA) for statistical analysis.
We established two groups based on postoperative transfusion. We used the Kolmogorov–Smirnov test to determine if the variables were normally distributed. We performed a descriptive analysis of the qualitative variables, defining their absolute frequency and percentage, and of the quantitative variables using the mean and standard deviation.
The comparative analysis of the qualitative variables was performed using the Chi-square test and its (Phi) measure of association to assess their independence and correlation. The odds ratio was used to estimate risk for each variable. Quantitative variables were analysed using the Student's t-test for independent samples.
A significance level (α) of .05 was used for all hypothesis tests.
ResultsOf the total number of primary total hip replacements (THRs) performed at our centre between 2021 and 2023, 273 patients met the inclusion criteria (152 men, 121 women). The mean age was 66.9 years [27; 89]. 157 patients (69.2%) underwent right-sided surgery and 116 (38.8%) underwent left-sided surgery. ASA risk was categorised as I (20), II (161), III (89), and IV (3). Of the total included, 135 patients were hypertensive (49.5%) and 56 were diabetic (20.5%). Additionally, 40 patients were taking antiplatelet agents (14.6%) and 15 were taking anticoagulants (5.4%).
Tranexamic acid was administered intravenously at a rate of 2mg/kg/h in the operating room to 207 patients (75.8%), and a drain was placed in 133 patients (48.7%). The mean length of hospital stay was 2.5 days (1; 16). The approach was posterolateral in all 273 patients included in our study. All total hip replacements (THRs) were Polar R3 (Smith & Nephew®) and all were uncemented in both their acetabular and femoral components.
The mean preoperative haemoglobin (Hb) was 14.3g/dL [10; 19.7], the mean postoperative Hb was 11.1g/dL [7.2; 14.7], and the mean difference between preoperative and postoperative Hb was 3.27g/dL (0; 6.9). The preoperative haematocrit (Hct) was 43.3% (30.3; 55.9), the postoperative Hct was 33% (20.8; 44.9), and the difference between preoperative and postoperative Hct was 10.3% (0; 19.9).
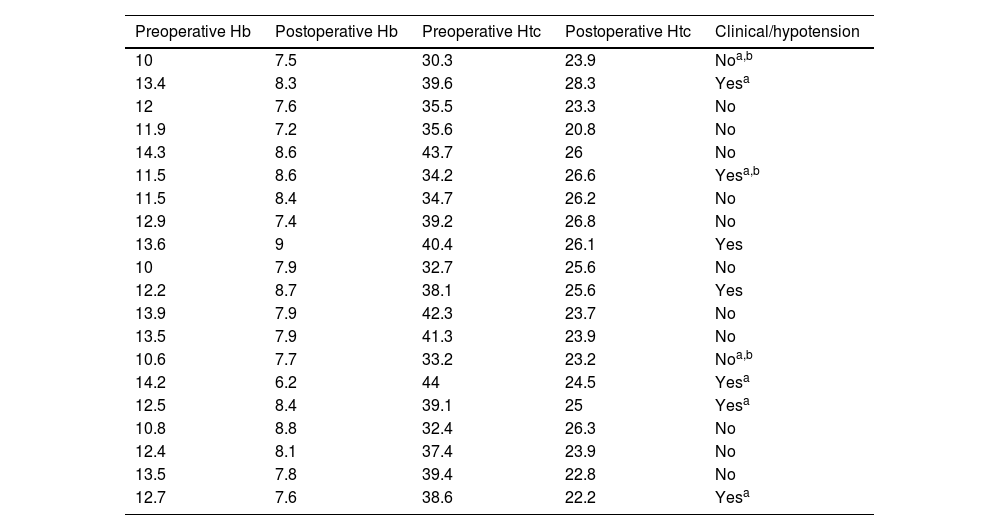
Postoperative blood transfusion was performed in 20 patients (7.3%), 11 of whom (55%) received it on the first postoperative day and 9 (45%) on the second postoperative day, always administering a single unit of packed red blood cells. The mean postoperative haemoglobin (Hb) of the patients who received blood transfusion was 8.1g/dL (7.2; 8.8g/dL), and only 7 of them presented with anaemia, hypotension, haematological or oncological pathology. The indication for transfusion in the remaining 13 patients was questionable, considering the transfusion criteria of the Spanish Society of Haematology (Table 1).
Analytical and clinical data of transfused patients.
| Preoperative Hb | Postoperative Hb | Preoperative Htc | Postoperative Htc | Clinical/hypotension |
|---|---|---|---|---|
| 10 | 7.5 | 30.3 | 23.9 | Noa,b |
| 13.4 | 8.3 | 39.6 | 28.3 | Yesa |
| 12 | 7.6 | 35.5 | 23.3 | No |
| 11.9 | 7.2 | 35.6 | 20.8 | No |
| 14.3 | 8.6 | 43.7 | 26 | No |
| 11.5 | 8.6 | 34.2 | 26.6 | Yesa,b |
| 11.5 | 8.4 | 34.7 | 26.2 | No |
| 12.9 | 7.4 | 39.2 | 26.8 | No |
| 13.6 | 9 | 40.4 | 26.1 | Yes |
| 10 | 7.9 | 32.7 | 25.6 | No |
| 12.2 | 8.7 | 38.1 | 25.6 | Yes |
| 13.9 | 7.9 | 42.3 | 23.7 | No |
| 13.5 | 7.9 | 41.3 | 23.9 | No |
| 10.6 | 7.7 | 33.2 | 23.2 | Noa,b |
| 14.2 | 6.2 | 44 | 24.5 | Yesa |
| 12.5 | 8.4 | 39.1 | 25 | Yesa |
| 10.8 | 8.8 | 32.4 | 26.3 | No |
| 12.4 | 8.1 | 37.4 | 23.9 | No |
| 13.5 | 7.8 | 39.4 | 22.8 | No |
| 12.7 | 7.6 | 38.6 | 22.2 | Yesa |
Hb: haemoglobin; Hct: haematocrit.
Of all the variables evaluated in the study, female sex, the presence of drainage, and preoperative haemoglobin levels below 13g/dL were statistically significantly associated with the risk of blood transfusion (p<.05). Patients requiring blood transfusion were hospitalised longer than those who did not (2.53 vs. 4 days) (p<0.05).
The cost of performing preoperative cross-matching on all patients undergoing prosthetic surgery was €21,840 (273 tests×€80), without being able to economically assess the other indirect costs involved, such as the inconvenience to the patient who had to arrive at the hospital a day early (cost of the patient's lost workday or lost profitability for the company), nursing costs, and patient transport costs, among others.
DiscussionPreoperative anaemia is a significant risk factor for blood transfusion after orthopaedic surgery, which increases the costs of the healthcare intervention, both direct and indirect, due to the comorbidity associated with the transfusion itself. Therefore, early treatment is recommended after its detection in the preoperative evaluation of elective orthopaedic surgeries with a high risk of bleeding, such as primary hip arthroplasty.10 In our study, we observed that, with the exception of two, all patients requiring blood transfusion had a haemoglobin (Hb) level<13g/dL.
Currently, preoperative Hb concentration is considered the most reliable predictor of postoperative transfusion in these patients, so the evidence indicates that the main objective is to optimise this concentration prior to surgery.11
Furthermore, an increase in infection and morbidity/mortality rates has been observed in patients requiring postoperative blood transfusion, highlighting the need for careful patient selection, as this technique is not without risks.12
In recent years, strategies have been sought to manage blood bank resources more efficiently and minimise unnecessary costs. Recently, there has been a growing advocacy for the implementation of patient blood management strategies in healthcare centres, aimed at minimising unnecessary transfusions in clinical practice, as Pinilla et al. have attempted to demonstrate. In a retrospective observational study of patients undergoing primary total portosystemic shunt (TPS) between 2017 and 2019 following the implementation of the blood-saving PBM programme at their hospital, transfusion rates of 2.34% were obtained in a total of 384 patients.4
These data differ from those obtained in our study, in which the transfusion rate was 7.3%. While it is true that 13 of the 20 transfusions performed had a questionable indication according to the transfusion criteria of the Spanish Society of Haematology (Hb<8g/dL associated with anaemia, hypotension, significant cardiovascular disease, ST-segment elevation myocardial infarction, severe thrombocytopenia, haematological or oncological disorders; or Hb<7g/dL),8 there are studies that associate a dramatic increase in mortality when Hb falls below 7g/dL. Likewise, our average stay was shorter, at 2.5 days.
Therefore, there is increasing advocacy for the creation of blood-saving programmes that optimise the patient's condition prior to surgery. In addition, mechanisms exist to reduce intraoperative blood loss, such as the use of intravenous tranexamic acid.13 At our centre, the haematology department is developing the PBM4 for orthopaedic surgery to reduce surgical risk in patients with preoperative anaemia.
To et al.11 designed a cohort study that identified statistically significant risk factors in a total of 1390 patients (737 in the derivation group and 653 in the validation group) undergoing hip and knee arthroplasty. These factors included preoperative haemoglobin concentration, type of surgical procedure, and age over 65 years in combination with female sex. Postoperative transfusion rates were 25% and 15%, respectively, in each group. Our data showed that female gender was a risk factor, while age was not statistically significant.
Regarding the use of complementary strategies to reduce the risk of bleeding, the benefit of administering tranexamic acid intravenously is becoming increasingly well-established. In a 2018 meta-analysis based on level 1 evidence studies by Borsinger et al.,14 which evaluated the efficacy of tranexamic acid in primary hip arthroplasty surgery, they concluded that the safety and efficacy of this drug, as well as the reduction in blood loss, allergenic transfusions, and hospital stay, support its routine use in this type of procedure, provided that contraindications for which a patient should not receive it are taken into account. In our study, tranexamic acid reduced the risk of blood transfusion. However, this reduction was not statistically significant, likely due to the small sample size.
Finally, the excessive use of routine cross-matching in elective orthopaedic surgery has been investigated. The combined results of a meta-analysis by Núñez et al.,15 which analysed this variable, concluded that 96.3% of patients undergoing primary total knee replacement (TKR) and primary knee arthroplasty (KNA) were subject to excessive cross-matching. Considering the calculated cost of €21,840 in our study, we believe that discontinuing routine cross-matching would represent significant savings for the healthcare system, always bearing in mind that each case must be individualised.
ConclusionsThe transfusion rate after primary TKR was 7.3%, with female sex, use of surgical drainage, and a preoperative haemoglobin level below 13g/dL identified as risk factors. These results support the need to abandon the routine use of preoperative cross-matching, favouring an individualised approach, which would imply significant cost savings for the healthcare system. Future strategies should focus on preoperative patient optimisation and the development of transfusion protocols agreed upon with the haematology service.
Level of evidenceLevel of evidence iv.
Ethical considerationsNo patient data appear in this article. No experiments on humans or animals were performed in this research.
FundingNo funding of any type exists.
Conflict of interestsNone.
1. Bierbaum BE, Callaghan JJ, Galante JO, Rubash HE, Tooms RE, Welch RB. An analysis of blood management in patients having a total hip or knee arthroplasty. J Bone Joint Surg Am. 1999;81:2–10, https://doi.org/10.2106/00004623-199901000-00002. PMID: 9973048.
2. Cai L, Chen L, Zhao C, Han G, Wang Q, Kang P. Do patients with borderline anemia need treatment before total hip arthroplasty? A propensity score-matched cohort study. Orthop Surg. 2024;16:123–31, https://doi.org/10.1111/os.13955.
3. García-Dobarganes-Barlow FE, Romo-Aguilera IJ, Negrete-Corona J, Guevara Álvarez A, Garcini-Munguía FA, Téllez-Hoyos S. Effectiveness of tranexamic acid for decreased allogenic blood transfusion in total hip arthroplasty. Acta Ortop Mex. 2020;34. PMID: 33230992.
4. Liu KC, Bagrodia N, Richardson MK, Piple AS, Kusnezov N, Wang JC, et al. Risk factors associated with thromboembolic complications after total hip arthroplasty: an analysis of 1129 pulmonary emboli. J Am Acad Orthop Surg. 2024;32:e706–15, https://doi.org/10.5435/JAAOS-D-23-01213.
5. Molko S, Dasí-Sola M, Marco F, Combalía A. El proceso de atención de las artroplastias primarias totales de rodilla y cadera en Spain: un estudio a nivel nacional. Rev Esp Cir Ortop Traumatol. 2019;63:408–15, https://doi.org/10.1016/j.recot.2019.06.005.
6. Núñez JH, Colomina J, Anglès F, Pallisó F, Acosta HF, Mateu D, et al. Routine pretransfusion testing before primary total hip or knee arthroplasty are an expensive and wasteful routine. Systematic review and metaanalysis. Arch Orthop Trauma Surg. 2024;144:1585–95, https://doi.org/10.1007/s00402-024-05243-3.