The most common tibial plateau fractures are AO 41B3/Schatzker type 2 (external unicondylar lesions with a vertical fracture line). The goal of treatment for these fractures is the satisfactory restoration of mechanical alignment, anatomic reduction of the articular surface, and stable fixation to allow early range of motion. The aim of our study is to determine the factors that most influence long-term functional and quality of life outcomes after surgical treatment by strictly selecting previously healthy patients facing an unexpected external tibial plateau fracture.
Material and methodA retrospective study was conducted in our tertiary hospital after obtaining approval from the ethics committee. Data from patients with external tibial plateau fracture hospitalized between 2013 and 2018 with more than 3 years of evolution were analyzed. All patients who met the strict inclusion criteria completed the KOOS, EQ-5D profile and VAS questionnaires. In addition, they underwent a physical examination and radiological study using telemetry and computed tomography (CT). The clinical data collected from the patients were: age, sex, fracture side, implant use, graft use, days elapsed until surgery, years after surgery, ASA, range of motion in extension and flexion. The radiological data were: in the telemetry, the deviation in mm of the load axis with respect to the contralateral limb was analyzed, the MPTA of both limbs and the difference in degrees between them; in the CT, the maximum joint step was measured and the affected area was calculated in cm2 as well as the largest anteroposterior diameter and maximum width in mm (maximum anteroposterior and transverse diameters).
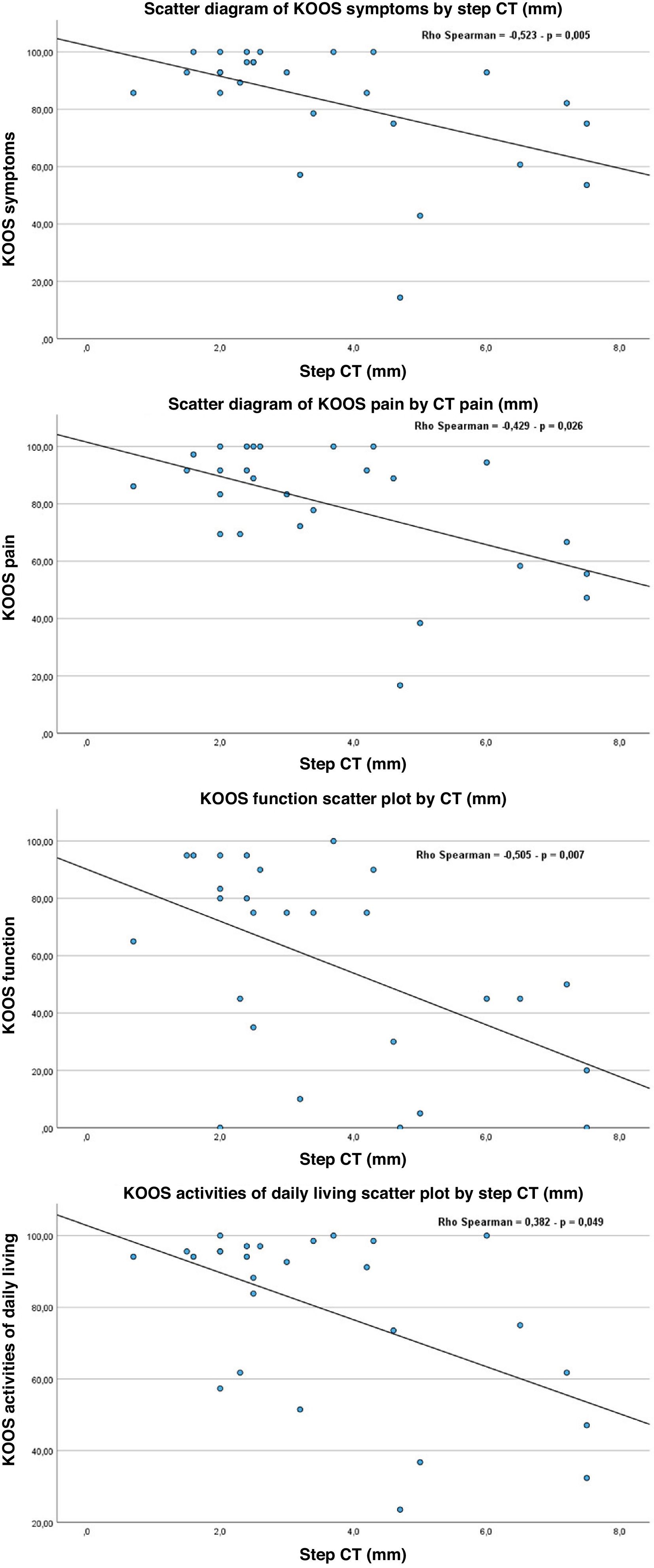
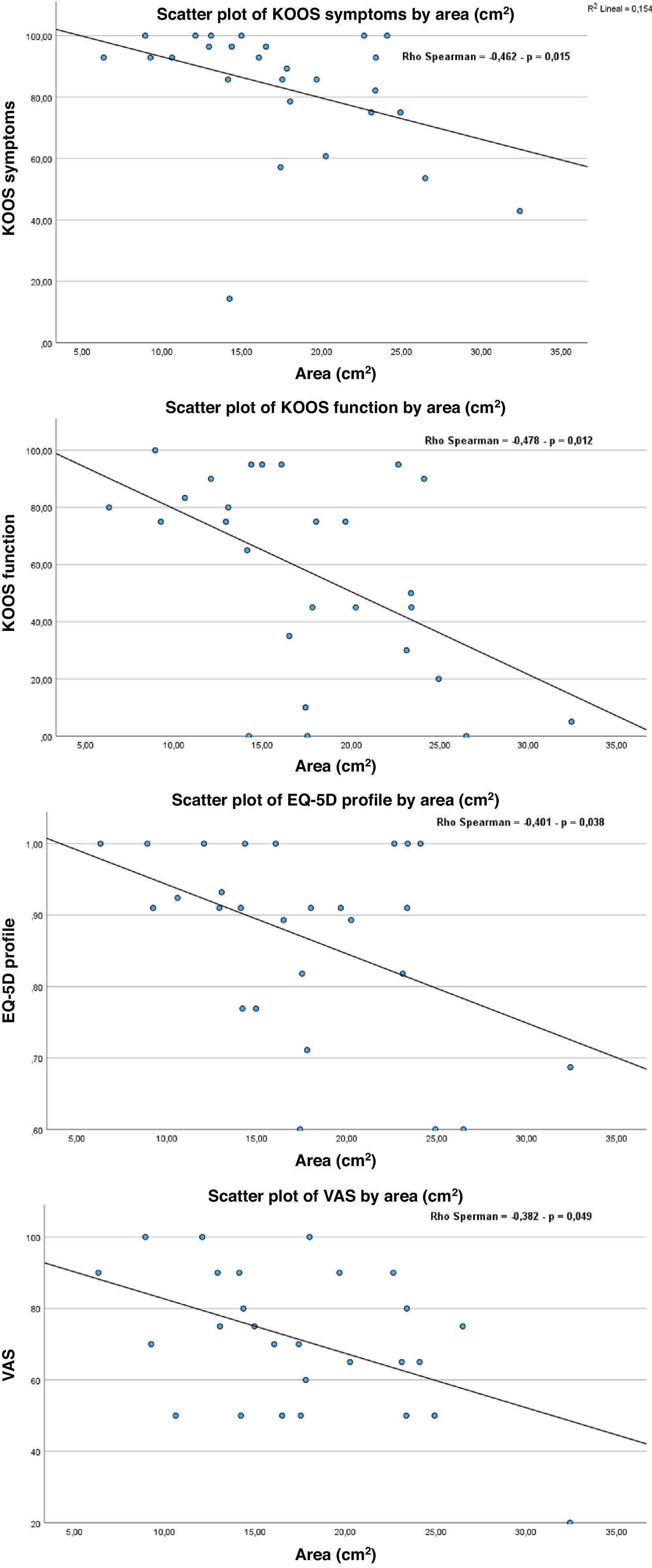
ResultsA total of 27 patients were analysed, with a mean age of 53.3 years and a mean evaluation time since the fracture of 4.8 years. We found statistically significant correlations (p<.05) between: days until surgery and size of the area in cm2 (p=.042) and step in mm (p=.028), that is, the more days of delay, the greater the area and the greater the step; being a man presented a positive correlation with having a greater step (p=.025), greater area (p=.007) and greater slope (p=.039) compared to women. A statistically significant relationship was observed between the area of residual fracture and the values of KOOS symptoms (p=.015), KOOS function (p=.012), EQ-5D profile (p=.038) and VAS (p=.049); the greater the affected area, the worse the patient's condition. We also detected significant correlations between increased joint step and KOOS symptoms (p=.005), KOOS pain (p=.026), KOOS activities of daily living (p=.049) and KOOS function (p=.007); the higher the step, the worse the patient's situation.
ConclusionIn conclusion, it can be observed that the most important aspect when it comes to obtaining good results in terms of patient satisfaction in the long term is the restoration of the joint line, avoiding large depressions and minimizing the area of residual joint involvement.
Las fracturas de meseta tibial más frecuentes son las tipo AO 41B3/Schatzker tipo 2 (lesiones unicondilares externas con línea de fractura vertical). El objetivo del tratamiento de estas fracturas es la restauración satisfactoria de la alineación mecánica, la reducción anatómica de la superficie articular y la fijación estable para permitir un rango de movimiento temprano. El objetivo de nuestro estudio es conocer los factores que más influyen en los resultados funcionales y de calidad de vida a largo plazo tras el tratamiento quirúrgico mediante la selección estricta de pacientes previamente sanos que afrontan una fractura inesperada de meseta tibial externa.
Material y métodoSe realizó un estudio retrospectivo en nuestro hospital de tercer nivel tras obtener la aprobación por parte del comité de ética. Se analizaron datos de pacientes con fractura de meseta tibial externa hospitalizados entre los años 2013 y 2018 con más de 3años de evolución. Todos los pacientes que cumplieron los estrictos criterios de inclusión completaron los cuestionarios KOOS, EQ-5-D Profile y VAS. Además, se les realizó un examen físico y un estudio radiológico mediante telemetría y tomografía computarizada (TC). Los datos clínicos recogidos de los pacientes fueron: edad, sexo, lado de la fractura, uso de implante, uso de injerto, días transcurridos hasta la cirugía, años tras la cirugía, ASA, rango de movilidad en extensión y flexión. Los datos radiológicos fueron: en la telemetría se analizó la desviación en mm del eje de carga respecto al miembro contralateral, el MPTA de ambos miembros y la diferencia en grados entre ellos; en la TC se midió el escalón articular máximo y se calculó el área afecta en cm2 así como el diámetro mayor anteroposterior y la anchura máxima en mm (diámetros máximos anteroposterior y transversal).
ResultadosSe analizaron un total de 27 pacientes, con edad media de 53,3años y tiempo de evaluación medio desde la fractura de 4,8años. Encontramos correlaciones estadísticamente significativas (p<0,05) entre: días hasta cirugía y tamaño del área en cm2 (p=0,042) y del escalón en mm (p=0,028), es decir, a más días de demora mayor área y mayor escalón; ser hombre presentó una correlación positiva con tener mayor escalón (p=0,025), mayor área (p=0,007) y mayor slope (p=0,039) frente a las mujeres. Se observó relación estadísticamente significativa entre el área de fractura residual y los valores de KOOS síntomas (p=0,015), KOOS función (p=0,012), EQ-5D profile (p=0,038) y VAS (p=0,049), siendo a mayor área afectada peor estado del paciente. También detectamos correlaciones significativas entre el escalón articular aumentado y KOOS síntomas (p=0,005), KOOS dolor (p=0,026), KOOS actividades cotidianas de la vida diaria (p=0,049) y KOOS función (p=0,007), siendo a mayor escalón peor situación del paciente.
ConclusiónEn conclusión, se puede observar que el aspecto más importante a la hora de obtener buenos resultados en cuanto a la satisfacción del paciente a largo plazo es la restauración de la línea articular evitando grandes depresiones y disminuyendo al máximo el área de afectación articular residual.
Tibial plateau fractures account for 1%–2% of all fractures. Seventy percent affect the lateral plateau, 10%–30% are bicondylar and fewer than 10% affect only the medial condyle.1–6
These fractures have a bimodal distribution: in young patients, they are usually the result of a high-energy trauma mechanism (e.g. falls from height or traffic accidents), whereas in elderly patients with osteoporosis, they typically result from a low-energy trauma mechanism. These fractures are caused by axial loading with varus or valgus deviation.1–3 In recent decades, there has been an increase in osteoporotic fractures in women resulting from low-energy trauma.4
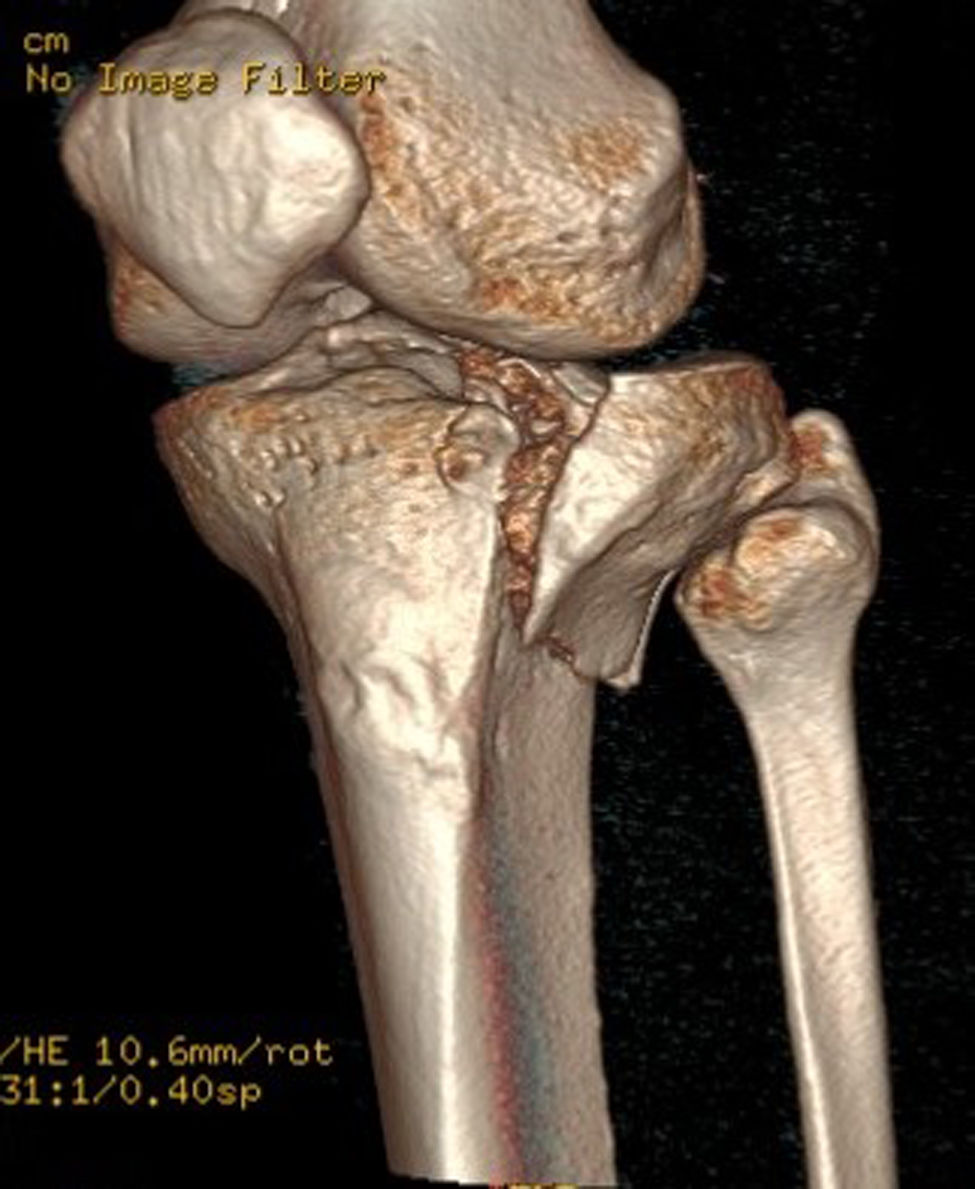
Several classifications of tibial plateau fractures exist, based on their location and displacement. The most widely used is the Schatzker classification, which divides fractures into 6 types, ranging from the least to the most severe. The AO classification is the most extensive, corresponding to 41 A-B-C. Luo's three-column classification is the simplest for surgical planning purposes. In all epidemiological studies, the most frequent fractures are Schatzker type 2 or AO 41B3. These correspond to an external unicondylar fracture pattern caused by a valgus mechanism involving depression and a vertical fracture line.1–7 The advent of CT and 3D models has greatly contributed to the description of different fracture patterns for adequate surgical planning,1–6 with the posterolateral area being described as having the highest incidence of fracture lines and poor reduction2,6 (Fig. 1).
As with other tibial plateau fractures, the objective of treating these fractures is to restore mechanical alignment and achieve anatomical reduction of the joint surface satisfactorily, while providing stable fixation to allow an early range of motion. Treatment for external unicondylar injuries with a vertical fracture line often requires open reduction and internal fixation. This involves raising the depressed articular surface and sometimes grafting the bone defect, as well as osteosynthesis.7,8
Several studies have determined the importance of restoring the anatomy of the articular surface in the surgical treatment of tibial plateau fractures, with better results and less development of secondary osteoarthritis being observed the less the residual joint depression.9–15 Other factors related to the prognosis of these fractures include alteration of the mechanical axis of the affected limb and the area of joint involvement.10–12
While most studies on tibial plateau fractures investigate functional and quality of life outcomes in the short and medium term, relatively few explore these outcomes in the long term.11,15–19 Short-term results of surgical reduction are good.9–13 Recent studies estimate that the long-term conversion rate to total knee arthroplasty for tibial plateau fractures is around 10%,18,19 being higher for bicondylar fractures. However, they also suggest that inadequate reduction of unicondylar fractures carries a much higher risk.18
Many of the studies are heterogeneous, failing to select a specific fracture type, relying on simple radiological studies, and failing to differentiate the particular characteristics of each patient. This means that many long-term functional results are biased.
Our study aims to identify the factors that most influence long-term functional and quality of life outcomes after surgical treatment for Schatzker type 2/AO 41B3 fractures, by strictly selecting previously healthy patients who have suffered an unexpected fracture of the external tibial plateau. To this end, we will use radiological tests, including telemetry and CT scans, as well as functional and quality of life assessment scales to study these factors in the medium to long term.
Material and methodsA retrospective study was conducted at our tertiary hospital after approval from the ethics committee.
Data from patients with external tibial plateau fractures classified as AO 41B3 and Schatzker type 2 who were hospitalised between 2013 and 2018 were analysed from our hospital's computer database.
The inclusion criteria were:
- 1
Non-pathological AO 41B3/Schatzker type 2 fractures (defined by preoperative CT).
- 2
ASA less than or equal to III.
- 3
No previous surgical injury to the same or contralateral limb.
- 4
Independent ambulation prior to the fracture.
- 5
A minimum of 3 years since the fracture.
- 6
Age between 18 and 85 years.
- 7
No knee arthroplasty as treatment after the fracture.
All patients who did not meet the above criteria were excluded, as were those who could not be contacted for follow-up. All patients who met the inclusion criteria completed a questionnaire and underwent a physical examination and radiological studies (telemetry and computed tomography scan [CT]).
The clinical data collected from patients included age, sex, side of fracture, use of implant, use of graft, days to surgery, years after surgery, ASA, range of motion (ROM) in extension and flexion.
Patients completed the KOOS questionnaires – which analysed pain, daily activities, functionality, and quality of life – the EQ-5D profile, and the VAS.
The radiological tests performed prior to surgery were assessed by the authors, and the fracture classification was determined by consensus according to the OTA/AO classification. All patients with a fracture history of more than 3 years underwent teleradiology of the lower limbs and a CT scan. The radiographic analyses were evaluated by two independent radiologists.
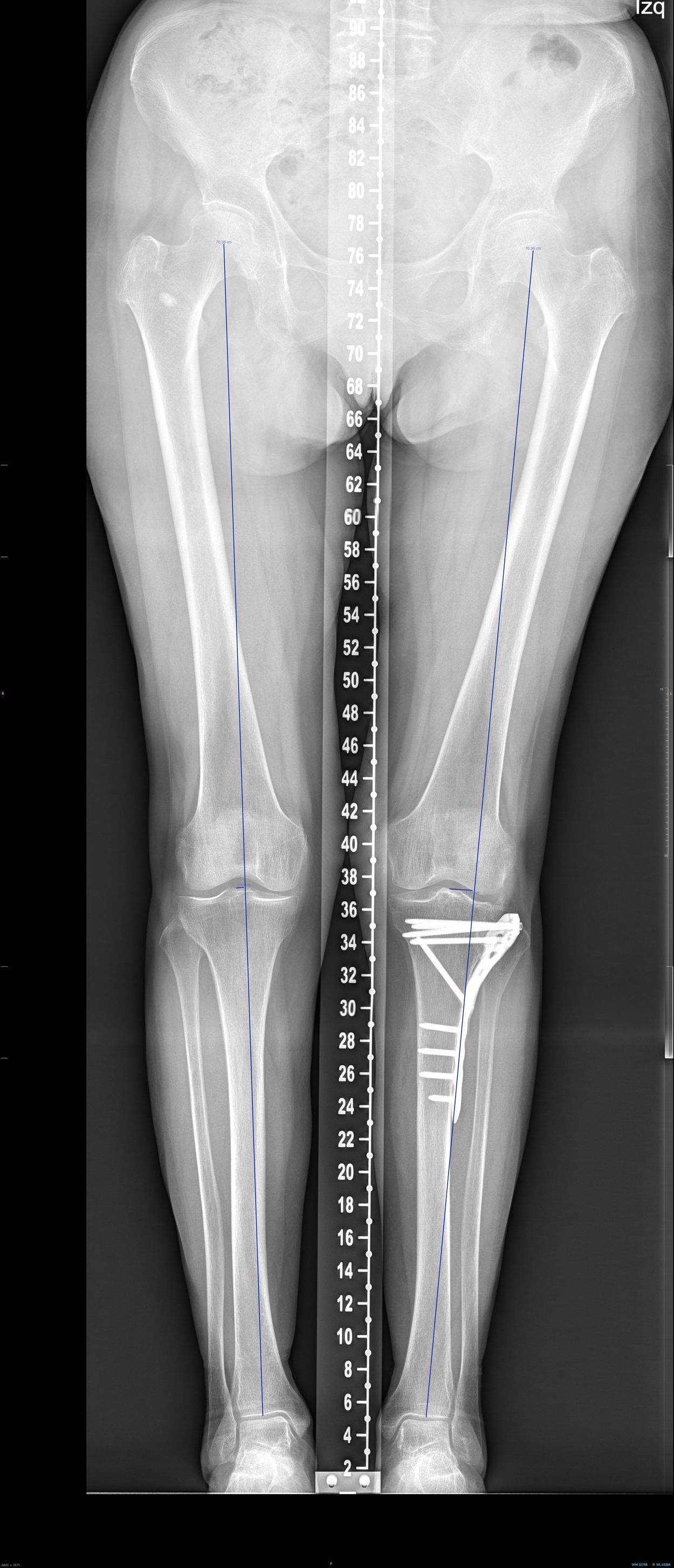
Deviation in millimetres of the load axis relative to the contralateral limb, the medial proximal tibial angle (MPTA) of both limbs, and the difference in degrees between them were analysed using telemetry (Fig. 2).
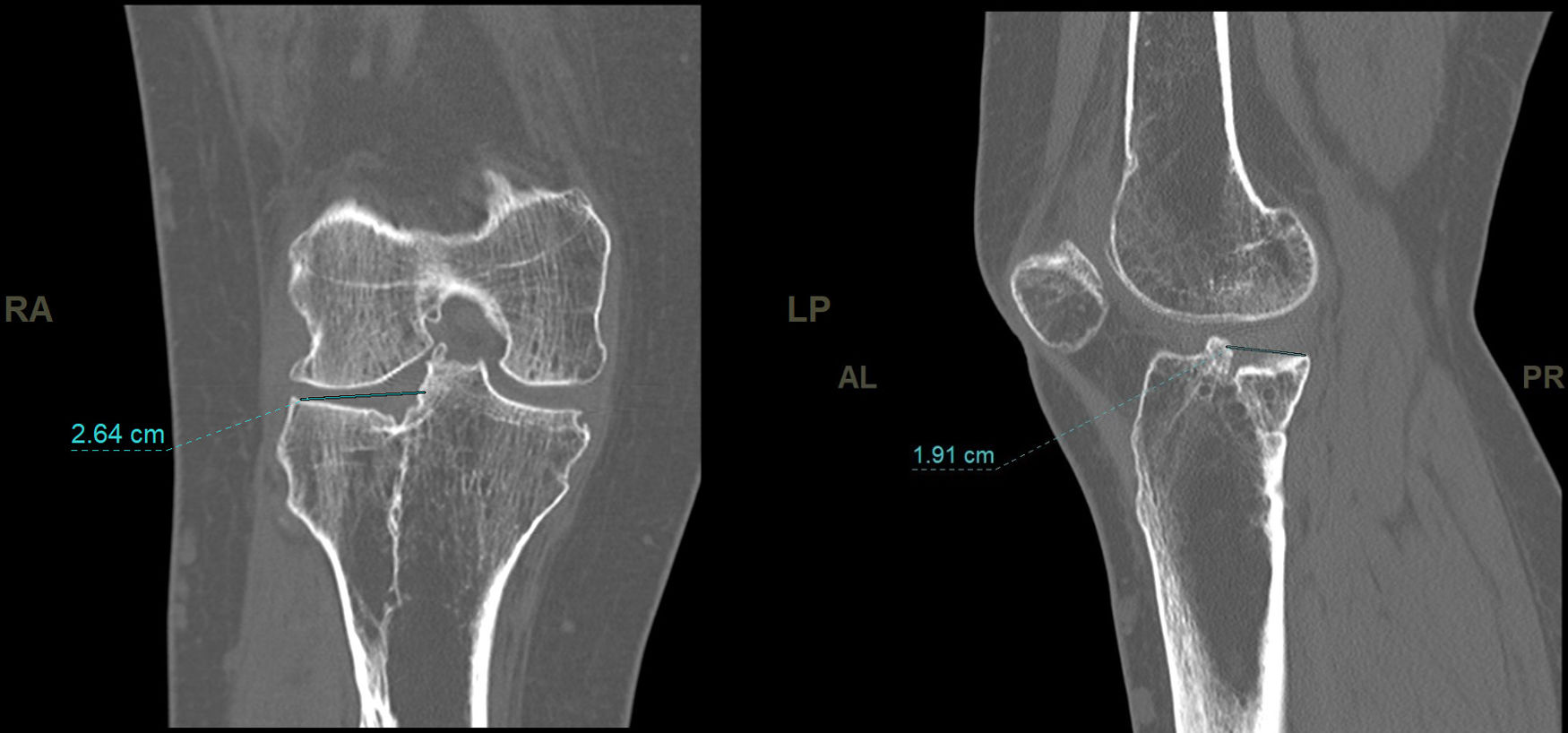
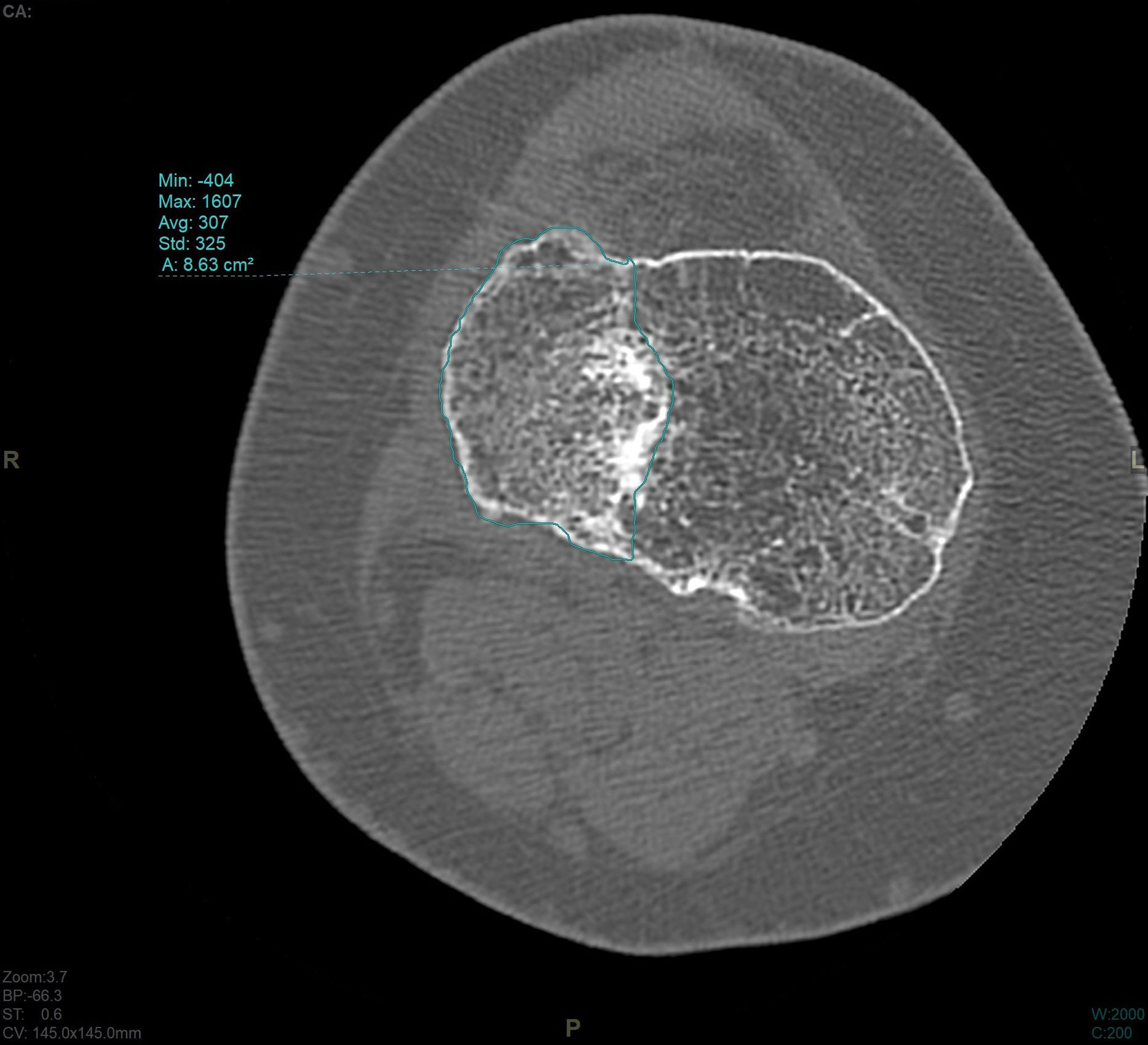
In the CT study, volumetric acquisition was performed using a multi-slice scanner at .6mm thickness, followed by multiplanar reconstruction at 1.5mm slice intervals. In coronal plane reconstruction, the point of greatest fracture depression in millimetres, corresponding to the maximum joint step, and the maximum width/transverse diameter in millimetres were analysed. In the sagittal plane, the maximum anteroposterior joint step diameter in millimetres and the maximum external tibial plateau slope in degrees were measured (Fig. 3). Post-processing in the axial plane involved delimiting the fracture contour and calculating the affected area in cm2, as well as determining the maximum anteroposterior and transverse diameters in mm (Fig. 4).
The results were analysed using the non-parametric Mann–Whitney U-test and Spearman's non-parametric correlation coefficient, Rho. A p-value of less than .05 was taken to indicate statistical significance.
ResultsA total of 203 tibial plateau fractures were recorded in our hospital database between 2013 and 2018. Of these, 73 fractures (36%) corresponded to AO classification 41B3/Schatzker 2. Thirty-six patients met the inclusion criteria and 37 did not (5 because they underwent total knee arthroplasty and 32 patients could not be located or did not meet the inclusion criteria described above). Of the 36 who responded to the questionnaire, 9 declined to undergo CT after being informed of the radiation exposure, and therefore a total of 27 patients were ultimately analysed. The mean age of the patients was 53.3 years, with a standard deviation (SD) of 12.6 years, ranging from 25 to 78 years. Of the patients, 70.4% (n=19) were female. Most patients were ASA II or lower. Thirteen fractures were on the right side and 14 on the left.
The mean time to surgery was 8.4 days (SD: 3.6 days). The follow-up time (examination, questionnaires, radiographic tests) since surgery was 4.8 years (range 3–8 years).
Except for one patient (3.7%) in whom cannulated screws were used; the rest of the patients (n=26) were treated with locking compression plates. Forty-four point four percent (n=12) required grafting. All surgeons in the department participated in treating this type of fracture without subspecialisation, considering it to be a general trauma pathology. No deep wound infections were detected, but three patients had superficial problems that were resolved without surgery. At the time of the questionnaire, 12 patients had undergone further surgery to remove osteosynthesis material more than a year after the fracture.
In the teleradiology analysis, the difference in the mean axis deviation from the contralateral leg was 12mm. The mean difference in MPTA was −1.1 degrees.
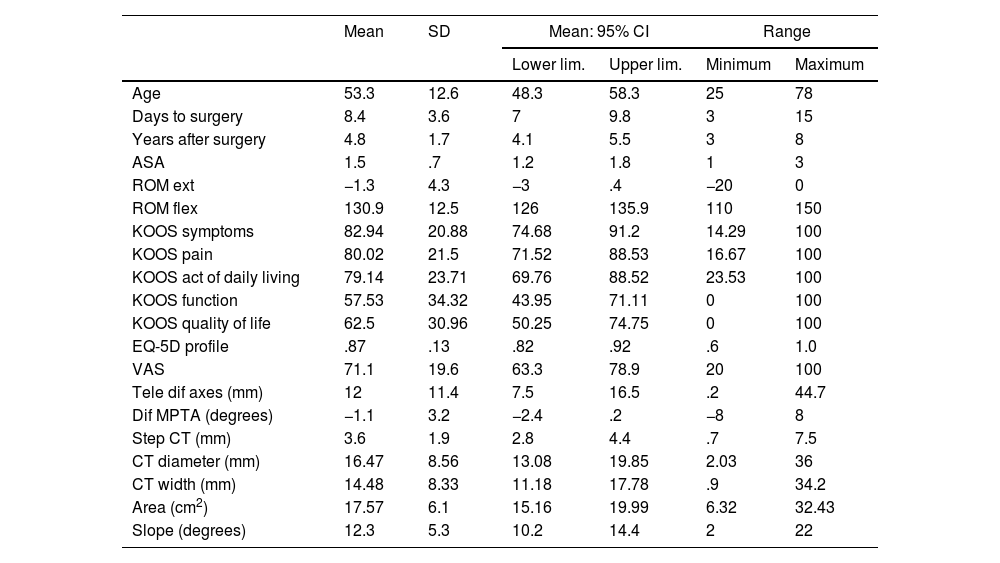
The mean step measured on CT was 3.6mm (SD: 1.9mm). The mean area measured on CT was 17.57cm2 (SD: 6.1cm2). The mean slope was 12.3 degrees (SD: 5.3 degrees).
The rest of the measurements analysed, as well as the KOOS, EQ-5D profile, and VAS scales, are shown in Table 1.
Variables.
| Mean | SD | Mean: 95% CI | Range | |||
|---|---|---|---|---|---|---|
| Lower lim. | Upper lim. | Minimum | Maximum | |||
| Age | 53.3 | 12.6 | 48.3 | 58.3 | 25 | 78 |
| Days to surgery | 8.4 | 3.6 | 7 | 9.8 | 3 | 15 |
| Years after surgery | 4.8 | 1.7 | 4.1 | 5.5 | 3 | 8 |
| ASA | 1.5 | .7 | 1.2 | 1.8 | 1 | 3 |
| ROM ext | −1.3 | 4.3 | −3 | .4 | −20 | 0 |
| ROM flex | 130.9 | 12.5 | 126 | 135.9 | 110 | 150 |
| KOOS symptoms | 82.94 | 20.88 | 74.68 | 91.2 | 14.29 | 100 |
| KOOS pain | 80.02 | 21.5 | 71.52 | 88.53 | 16.67 | 100 |
| KOOS act of daily living | 79.14 | 23.71 | 69.76 | 88.52 | 23.53 | 100 |
| KOOS function | 57.53 | 34.32 | 43.95 | 71.11 | 0 | 100 |
| KOOS quality of life | 62.5 | 30.96 | 50.25 | 74.75 | 0 | 100 |
| EQ-5D profile | .87 | .13 | .82 | .92 | .6 | 1.0 |
| VAS | 71.1 | 19.6 | 63.3 | 78.9 | 20 | 100 |
| Tele dif axes (mm) | 12 | 11.4 | 7.5 | 16.5 | .2 | 44.7 |
| Dif MPTA (degrees) | −1.1 | 3.2 | −2.4 | .2 | −8 | 8 |
| Step CT (mm) | 3.6 | 1.9 | 2.8 | 4.4 | .7 | 7.5 |
| CT diameter (mm) | 16.47 | 8.56 | 13.08 | 19.85 | 2.03 | 36 |
| CT width (mm) | 14.48 | 8.33 | 11.18 | 17.78 | .9 | 34.2 |
| Area (cm2) | 17.57 | 6.1 | 15.16 | 19.99 | 6.32 | 32.43 |
| Slope (degrees) | 12.3 | 5.3 | 10.2 | 14.4 | 2 | 22 |
Quantitative statistical analysis was performed between age, days to surgery, ROM in extension, ROM in flexion, ASA, sex, laterality, and use or non-use of graft with the difference in telemetry axes, difference in MPTA degrees, slope degrees, CT area, and CT step.
We found statistically significant correlations (p<.05) between: days to surgery and area size in cm2 (p=.042) and step in mm (p=.028); that is, the longer the delay, the larger the area and the greater the step; being male presents a positive correlation with having a greater step (p=.025), larger area (p=.007), and greater slope (p=.039) compared to females.
Qualitative statistical analysis was performed between KOOS symptoms, KOOS pain, KOOS daily activities, KOOS function, KOOS quality of life, EQ-5D profile, and VAS with differences in telemetry axes, differences in MPTA degrees, slope degrees, CT area, and CT step.
A statistically significant relationship was observed between the residual fracture area and the values of KOOS symptoms (p=.015), KOOS function (p=.012), EQ-5D profile (p=.038), and VAS (p=.049), with a larger affected area corresponding to a worse patient condition. We also detected significant correlations between increased joint step and KOOS symptoms (p=.005), KOOS pain (p=.026), KOOS activities of daily living (p=.049) and KOOS function (p=.007), with a larger step corresponding to a worse patient condition (Figs. 5 and 6).
The rest of the analyses (difference in telemetry axes, difference in MPTA degrees, slope degrees) did not detect statistical significance.
DiscussionTibial plateau fractures involve the weight-bearing surface of the knee joint. It is important to restore its anatomy to improve overall function and minimise disability and rates of post-traumatic osteoarthritis.6–19
The optimal treatment for tibial plateau fractures has been controversial for several decades and remains so today. Although studies published in recent years analysing AO 41B3 tibial plateau fractures after surgical treatment show good results, most have small patient groups, heterogeneous fracture types, or short-term follow-ups.9–13 Recent long-term studies show that anatomical reduction is critical in preventing the need for arthroplasty.18,19
To preserve knee function, it is essential to ensure reduction as close to anatomical as possible at the time of surgery and to allow early mobilisation of the knee by restoring alignment, length, stability, and joint congruity.9–19 With this in mind, it is important to understand the shape of the fracture and choose the appropriate surgical method.1–8
In our study, we analysed the long-term functional and radiological outcomes of the most common type of tibial plateau fracture (AO 41B3/Schatzker 2), as well as the predictive factors that influence these outcomes, in patients who underwent surgery (osteosynthesis). Few studies7,13 focus solely on the most common pattern of tibial plateau fracture, and even fewer select patients without comorbidities that could compromise the study's final outcome.
Patient-reported results constitute the most effective measure to assess the effectiveness of treatment after surgical procedures, as they reflect their perception and are not observer-reported. The most commonly used outcome measures include pain scales (VAS) and quality of life questionnaires such as the EQ-5D. In our study, we also used the Knee Injury and Osteoarthritis Outcome Score (KOOS) questionnaire, a validated patient-reported measure of short- and long-term functional outcomes after knee fractures.9,16
Classic studies20,21 assessing the most important factors for achieving good results after tibial plateau fractures found no relationship between degree of joint depression and functional outcomes. Studies such as that by Lansinger et al.,20 considered functional outcomes to be acceptable if depression of the articular surface was less than 10mm. However, the main limitation of these studies was often inadequate analysis of the radiographs, since measurements made using simple radiography and/or telemetry are less accurate and more observer-dependent. Subsequent studies2,9,12,13 analysed the results using CT. Studies by Singleton et al.9 analysed tomography slices to evaluate articular depression. Following a 3.9-year follow-up period, they observed that patients with lower levels of residual joint depression (less than 2.5mm) experienced less disability and achieved significantly higher scores on the IOWA, Oxford, KOOS and WOMAC scales. Rosteius et al.12 performed a postoperative CT scan within the first 72h after surgery. The intraarticular step and gap sizes, as well as the comminution area, were studied. Changes in these parameters, together with MPTA deviation, correlate with poorer functional outcomes. Both studies analysed several types of tibial plateau fracture. Therefore, these studies’ potential limitations are their short follow-up time, small patient numbers, and analysis of several fracture types. Despite our study having a small sample size, it analyses a single type of fracture in healthy patients with a follow-up period of more than 3 years. It also takes into account long-term postoperative telemetry and CT scans, and analyses functional outcomes using subjective tests that allow the patient's condition to be assessed.
Post-surgery CT scans enable more precise measurements to be taken of the extent of depression and bone defect remodelling. Even when the initial reduction appears to be correct, a significant proportion of patients experience an increase in articular surface depression.9–15 This may be due to post-surgical assessment using X-ray rather than CT, which underestimates the degree of reduction. However, it may also be due to different surgical treatment strategies, such as the type of osteosynthesis and the stability of the assembly, as well as post-operative strategies, such as the load on the joint. Early weight-bearing remains a controversial topic in various recent studies. Although the trend is towards early weight-bearing and mobilisation,22,23 it is still unclear in which situations and in what way this should be done. Some studies show alterations in parameters such as condylar width24 that could affect long-term results. Therefore, more specific studies seem necessary.22–24
Most recent studies observe a correlation between articular step/gap and the patient's functional status. Our current results corroborate the findings of the last decade, which advocate better functional outcomes with a smaller joint step. This conclusion states that even small depressions of 2mm can impact the quality of patients’ functional outcomes. Therefore, anatomical reduction of the joints should be prioritised.9–13 The mean step obtained in our long-term series is 3.6mm, which explains the poorer KOOS scale scores.
One of the most noteworthy aspects of our study is our analysis of long-term joint involvement. There is a clear correlation between the area of the tibial plateau affected by the fracture and the patient's clinical condition15,18,19: the larger the affected area, the poorer the expected outcome. While this result is synergistic with the maximum joint step, it takes into account the entire affected area, regardless of its degree of depression. In our study, the posterolateral area is the most affected and the most frequently poorly reduced, in line with other studies,2 which can be explained by difficult access to this anatomical area and, consequently, poor fixation. This has led to new treatment strategies for accessing this area,25–27 since traditionally (as in our study), these fractures were treated using lateral locking compression Plates 6–8 with or without bone grafting. However, good fixation in the posterolateral column was difficult to achieve.
Another factor to consider in terms of prognosis is any alteration to the axis of the affected limb. Several studies have found a correlation between valgus deviation in these fractures and worse outcomes.9–12 In our study, we found no significant differences, although it should be noted that comparing the difference in both limbs may suggest that varus knees ultimately achieve a less symptomatic neutral alignment. A specific analysis of knees with residual valgus could yield poorer scores.
In our study, delayed surgery was associated with poorer functional outcomes. Temporary external fixation was not used in any case; instead, immobilisation splints were used. No neurovascular complications were reported prior to surgery. As with other fractures, the integrity of soft tissues and the urgency of surgical treatment appear to influence functional prognosis. Being male was also associated with poorer outcomes.
The small sample size could be considered a limitation of our study, as only 27 patients out of the 73 Schatzker type 2 fractures collected were followed up. Difficulties were encountered in the follow-up, as some patients could not be contacted, did not meet the selection criteria, and others declined to undergo CT.
Another weakness of the study is that it involved only 5 patients who had undergone knee arthroplasty prior to the study. Although they were excluded from the inclusion criteria, the reasons for their treatment could still influence the final results. Another weakness is the absence of a detailed study of associated soft tissue injuries, which may also influence the results.
Despite the relatively small number of patients, statistical significance was obtained in multiple results. The strict selection criteria, which excluded patients with pathologies that could affect the final functional outcome, are a strength of the study, even though they reduced the final sample size and the patients’ overall age. While our study can be extrapolated to middle-aged patients, it draws few conclusions about elderly patients with high comorbidity.
Another limitation is the lack of comparability with the available literature, as few studies differentiate between comorbidities that affect the outcome when studying all types of tibial plateau fractures.
The variability in terms of surgeons (not belonging to specific units) could be another weakness of the study; however, it provides a clear perspective on the complexity of these fractures and the necessary specialisation required for their treatment in different orthopaedic surgery and traumatology departments.
This study suggests the need for new surgical treatment strategies for external unicondylar fractures with depression and vertical fracture lines, based on CT and 3D imaging, to preserve joint anatomy. It also raises the possibility of developing new classifications that consider previous depression and comminution. The study also raises the possibility of developing postoperative treatment protocols that allow weight-bearing and movement without depression, which could affect the final outcome. Alternatively, there may be a need to standardise CT as a short-term control test to assess joint depression, which could have repercussions on the quality of life of these patients.
In conclusion, our study shows that restoring the joint line, avoiding large depressions and minimising residual joint involvement are the most important factors in achieving good long-term results and patient satisfaction.
Level of evidenceLevel II evidence.
Conflict of interestsThe authors have no conflict of interests to declare.